* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Psychopharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Orphan drug wikipedia , lookup
Compounding wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
List of comic book drugs wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Drug interaction wikipedia , lookup
Theralizumab wikipedia , lookup
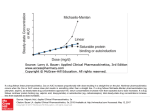
PHARMACOKINETICS INTRODUCTION 1. Definition: Is a study of what the body does to a drug -In Pharmacokinetics an attempt is made to quantify the various dispositional parameters regarding; • • • • Absorption Distribution Metabolism Excretion ADME 1 PHARMACOKINETICS--• • The relationship between the time course of drug concentrations attained in different regions of the body during and after dosing is termed pharmacokinetics (‘what the body does to the drugs’) To distinguish it from pharmacodynamics (‘what the drug does to the body’ i.e. events consequent on interaction of the drug with its receptor or other primary site of action) 2 PHARMACOKINETICS--• 1. 2. 3. 4. Pharmacokinetic knowledge contributes in many ways to practice of therapeutics, which include: Distinguishing between pharmacokinetic and pharmacodynamic causes of variation in and unexpected responses to drugs Evolving concepts that are common to all drugs; thus information gained about one drug helps in anticipating the pharmacokinetics of another drug Often explaining the manner of use of a drug and occasionally suggesting a more convenient or effective dosage regimen Often allowing anticipation of the likely outcome of a therapeutic manoeuvre. 3 Relationship between dose and effect Pharmacokinetics focuses on: • Dose administered • Absorption • Concentration in circulation---- in tissues • ↕ ---- elimination • Pharmacodynamics focuses on: • Drug concentration at site of action • Pharmacological effect • Clinical response -effectiveness & toxicity 4 Pharmacokinetics---• The standard dose of a drug is based on clinical trials in volunteers and patients who have average ability to: • Absorb • Distribute • & eliminate the drug • The doses obtained in clinical trials will in no way be suitable for every patient 5 Pharmacokinetics--• Several diseases like heart failure, renal failure, require dosage adjustments • These disease conditions modify specific pharmacokinetic parameters • The two basic pharmacokinetics parameters are volume of distribution and Clearance • (A good strategy for understanding the topic of pharmacokinetics is to read on the following and tackle the examples) 6 Single –compartment model or (One-compartment open model) • In this model the human body is considered to be one compartment, consisting of a single well stirred compartment with an apparent Volume of distribution (Vd): • Vd relates the amount of drug in the body (Q) to the concentration of the drug (C) in blood of plasma according to the following equation: Amount of drug in body (Q) Vd= ____________________= Units in Vol. plasma drug concentration (Cp) 7 Single –compartment model… • • • • Therefore Vd = Q/Cp Equation----------1 Q= Dose administered Cp=plasma concentration C can be measured from plasma (Cp) or from blood (Cb) • The Vd calculated from equation 1 is an apparent volume it is not a physical space • It is a hypothetical space if the drug could be uniformly distributed in the body Vd is calculated from equation ---1 above 8 EXERCISE 1 • Mrs. Jones was given the anticoagulant Warfarin at a dose of 200mg.The plasma concentration (Cp) was later measured to be 20 micrograms/ml • Calculate the theoretical Volume of distribution (Vd) of Warfarin in this patient • Approximately in which body water compartment is your drug likely to occupy in the table 1 below? (see next slide) 9 Table 1:Distribution of body water in a man of average build • • • • • Type Vol (Lts) Plasma 3.5 Interstitial 12 ECF 15.5 ICF 26.5 -------• TBW 42 % of body wt 5 17 22 38 -------60 10 Vd------• Remember that: • In some cases the Vd of a drug can exceed that of total body water • E.g. the Vd for propranolol is 3Lts of plasma this theoretical volume gives an index of how widely it is distributed in the body • Digoxin Vd is 500 Lts/70 kg man exceeding TBW see the table 1 above • The higher the Vd of a drug the more extensively it is distributed in the body 11 Clearance ( ml/min or Litres /h) • Drug elimination from the body is expressed as clearance • Clearance is the intrinsic ability of the body or its organs of elimination (usually kidneys and liver) to remove drug from the blood or plasma • Clearance is expressed as a volume/unit of time 12 Clearance---• Clearance principles are similar to the concepts in renal physiology • CL = Rate of elimination ----------------------------- Equation 2 Concentration Clearance is expressed in equation 2 above 13 Clearance---• It is important to recognize that clearance by itself does not indicate how much drug is being removed • Clearance only represents the volume of blood or plasma which would be completely cleared of a drug if it were present • Renal clearance, CLr is defined as the Vd of plasma containing a drug that is removed by the kidney in Unit time; 14 Renal clearance (CLr) Expressed by the equation; CLr = CuVu CP Cu = Urinary Concentration of drug Vu = Rate of urine flow Cp = plasma drug concentration 15 Total clearance • CLt = CLm +CLr + CL other • t= total body clearance is a sum of the different drug clearance mechanisms • m=metabolism • r=renal • t=total • CL other includes drug clearance by other routes like the lungs, sweat etc. 16 Capacity limited elimination OR Saturable metabolism • This is sometimes called saturable metabolism or saturation pharmacokinetics • This happens when the concentration of a drug approaches a value at which its metabolizing enzymes are saturated, its rate of metabolism becomes independent of the amount of drug undergoing the process 17 Capacity limited elimination OR Saturable metabolism… • This is called zero order kinetics • For any relatively small change in dose there may be a large change in plasma concentration if metabolism is saturated • Examples of drugs which exhibit saturable metabolism are Ethanol, Phenytoin & Aspirin • Many more drugs exhibit these kinetics at toxic concentrations 18 Elimination rate constant (Ke) • Represents the fraction of volume of distribution (Vd) which will be cleared of the drug per unit of time Ke is expressed by the following equation; Ke = CL ------- Equation 3 Vd E.g. A drug with a clearance of 10L/ day and a Vd of 100 L would have an elimination rate constant (Ke) of: 19 Elimination rate constant--• 10 L/day =0.1/ day 100L • 10/100= 0.1/day • This essentially defines “first- order elimination kinetics” where the fraction eliminated per unit time remains unchanged 20 Half life • • • Half-life of a drug = T1/2 Is the time required to change the amount of drug in the body by one halfduring elimination (or during a constant infusion) T1/2 is useful in designing drug dosage regimens. 21 Half life T ½ is expressed by the following equation T1/2 = .693 x Vd = 0.7xVd------ Equation 4 CL CL Note ; Most drugs exhibit first order kinetics where the rate of elimination is directly proportional to drug concentration. Drug concentrations then decays exponentially 22 Time to reach steady state drug concentration in plasma/blood (Cpss) • The time to reach steady state drug concentrations is calculated from the following equation: • Cpss = 4-5 x half life • This means it takes between 4-5 half lives to reach steady state concentrations in plasma/blood. • Cpss = steady state plasma concentrations 23 EXERCISE 2 • Mr Silver was given Drug X 80 mg for a specific infection. If the half life of Drug X is 4 hours (i) Calculate the time that will be required for drug X to reach Cpss in plasma (ii) What will be the drug level in plasma (Cp) after 4 half – lives elimination ? (iii) Calculate the total drug eliminated from the body after 4 half - lives 24 Half life and Ke (elimination rate constant) relationship • If the clearance is 10 ml per minute and suppose the elimination half -life is 70 minutes The Kel is CL =10 = 0.1 ---equation 5 Vd 100 • Kel is also equal to 0.693 = 0.693 t1/2 70 =0.7 = 0.01 70 25 Drug accumulation • When doses are repeated a drug can accumulate in the body until dosing stops • this is because it takes time to eliminate the drug from the body • Accumulation will occur if the dosing interval is shorter than 4 half lives • An index of accumulation is called ACUMULATION FACTOR= 26 Drug accumulation… • Accumulation factor 1 = ----------------- equtn. 6 Fraction lost in one dosing interval or = 1 -------------1- fraction remaining 27 Bioavailability • Is the fraction (F) of unchanged drug reaching the systemic circulation following administration by any route • The area under the blood concentration time curve (AUC) is a common measure of the extent of bioavailability • AUC = Area under the curve (s) 28 Area under curve (AUC) 29 Rate of drug administration • Please note that the rate of drug administration can be expressed by the following equation: = F X DOSE-------------------equation 7 • F= bioavailability fraction • (tau) = is the dosing interval 30 Exercise 3 • What is the administration rate for digoxin 0.25 mg (250 mcg) given once daily as : • Tablet and as for elixir Given that F for the tablet and elixir is 0.62 & 0.77 respectively? Please give your answers in mcg. 31 DRUG DOSAGE REGIMENS • The objective of a dosage regimen in therapeutics is to prescribe: doses, the size whose timing will provide the maximum therapeutic benefit at the minimum cost in unwanted effects. This is achieved by considering the pharmacokinetic factors that determine the dose concentration relationship Calculation of dosage regimens allow individualization of doses to achieve target therapeutic concentrations 32 Dosage regimens--• Target plasma concentration of some tablets may be available from tables in textbooks • They are a guide to show you some of the effective drug concentrations in certain disease conditions • However these are not to be relied upon 100% • Because, in some cases the target drug concentration may vary depending on the severity of a specific disease condition 33 Drug dosage regimens--• • Some of the effective concentration of some drugs (or target concentrations ) have been worked out They are available in some text books 34 Loading dose • When the time to reach Cpss (steady state plasma concentrations) is long especially with drugs with a long T1/2 • It is desirable to give an initial loading to promptly raising the concentration of a drug in plasma to the target concentration • Loading dose is described in the following equation: • Loading dose (amount of drug in the body immediately following the loading dose= Vd x Tc/F ----equation 8 • Vd = volume of distribution • Tc = Target concentration 35 • F= Bioavailability fraction EXERCISE 4 • Estimate the loading dose for oral digoxin which would be necessary to attain a target plasma level of 1.5 ng/ml. • Assume: Vd = 7.3 L/Kg; F of the tablet = 0.62 36 Maintenance dose • • • Maintenance dose: In most clinical situations drugs are administered to maintain a steady state concentration in the body (Cpss) Enough is given in each dose to replace the drug eliminated since the preceding dose To calculate the maintenance dose proceed as follows: 37 first calculate the dosing rate • • • • Dosing rate = CL X Tc CL=Clearance Tc= Target concentration Then proceed in the next step to calculate the maintenance dose using the dosing rate as shown below 38 Maintenances dose--• Maintenance dose is calculated in -------------------------equation 8 below: • Maintenance dose Dosing rate = __________ X DI F DI=Dosing interval F = bioavailability (fraction of the dose absorbed) 39 Example: maintenance dose calculation • A target plasma Theophylline concentration of 10mg|L is desired to relieve acute bronchial asthma in a patient. If the patient is a non smoker and otherwise normal except for bronchial asthma we may use mean Clearance given in table 3-1 on page 41 by Katzung et al 40 Maintenance dose calculation--Clearance of theophyline in tables is given as 2.8 L/h| 70 kg . Since the drug will be given I.V Infusion, F=1 Dosing rate =CL X Tc ---------------equation 9 =2.8 L|h (CL) x 10mg/L (Tc) : In this patient the proper infusion Or dosing rate IV will be 28 mg|h Maintenance dose = dosing rate/F x dosing interval in time. 41 Maintenance dose-• The maintenance dose of theophylline will be given orally (F=0.96 from F tables) • Maintenance dose is equal to = dosing rate/F x Dosing interval = 28mg/hr x 12 hrs/0.96 The maintenance dose = 350 mg 12 hourly 42 Effect of repeated doses Figure 8-9 Predicted behaviour of single-compartment model with continuous or intermittent drug administration. Smooth curve A shows the effect of continuous infusion for 4 days; curve B the same total amount of drug given in eight equal doses; and curve C the same total amount of drug given in four equal doses. The drug has a halflife of 17hours and a volume of distribution of 20litres. Note that in each case a steady state is effectively reached after about 2days (about three half-lives), and that the mean concentration reached in the steady state is the same for all three schedules. Downloaded from: StudentConsult (on 30 October 2009 09:11 AM) © 2005 Elsevier 43 Effect of repeated doses • The figure above shows a relationship between frequency of dosing and maximum and minimum plasma concentrations when a steady state concentration is desired • The smooth rising black line shows plasma concentration achieved by 100mg by iv infusion 44 Effect of repeated dosing--• The doses of 100mg twice a day and the 200 mg per day curves are shown on the same scale • In each of the three cases the mean steady state plasma concentration is the same at 10 mg/L this is achieved when a steady state concentration of the drug is reached 45 Two compartment model • It is common for drugs with significant lipid solubility to show evidence of distribution into more than one compartment after i/v injection. • The implication is that their concentration does not behave as though homogenous in one compartment, but is better modelled by being considered homogenous in each of two (central and peripheral) compartments 46 Two compartment model… • In this model the body is considered to be 2 compartments • With a central compartment usually the plasma (intravascular) • And a peripheral compartment (extra vascular) • Remember that two compartment model only affects the periodic time course of drug action • Read more 47 Uses of pharmacokinetics--• As a diagnostic tool • As a mean to evaluate the extent and rate of delivery of a drug • To predict and understand adverse drug reactions • As a mean for predicting drugs levels in tissues 48 Uses of pharmacokinetics--• As means of comparing animals within species or among species in drug handling • As means for quantitating biological variability • As means for mathematically describing drug levels in a biological system • Lastly, for explaining the manner of a drug’s use and suggesting improved dosage regimens 49 • Further Reading! 50