* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 4 Depressants
Survey
Document related concepts
Transcript
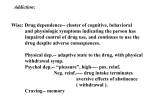
ALCOHOL #1 DRUG CH3CH2OH ethanol Average BC use is 8.8L of pure (100%) alcohol per person per year in 2007!! (equiv to 0.5L per day of beer) Alcohol is absorbed quickly: 58% in 30 min; 93% in 90 min BUT LIVER CAN ONLY OXIDIZE ALCOHOL at ~ 15g (½ ounce) per hour 1 Beer = 360 mL x 5% (EtOH) = 18 mL ~ ½ oz. (1 shot of spirits ~ same) so drinking faster than 1 beer or 1 shot per hour leads to accumulation of alcohol in blood. “0.08" = 80 mg alcohol per 100 mL blood A 70kg person reaches ‘.08’ with 3 beers and then eliminates about 1 beer per hour i.e. 5 beers over 2 h will keep you at .08 BUT it depend on weight, metabolism, amount of fat, etc. Alcohol dissipates throughout all tissues so heavier people can drink more but remain under limit NOTE THIS SAYS NOTHING ABOUT WHETHER YOU ARE IMPAIRED OR NOT!!!! Alcohol has a double action: between 0.01 and 0.05% inhibitions are removed, makes us happy but above this it is a CNS depressant 0.05% start to get clumsy, slow reaction times, risk taking 0.1% most are visibly drunk >0.2% most blackout >0.3% for most is coma (5-10h), then maybe death Tolerance develops so levels rise in experienced drinkers The lethal dose is about 700g for most ( i.e. about 1.5L of scotch straight down) ACTION 1 Stimulates acid production 2 Causes dilation of periphery blood vessels of skin - warm feeling, hot flushes, red face not good to give to hypothermia/drowning victims 3 Diuretic - stimulates urine production 4 Depresses sexual ‘performance’ in males ALCOHOL, THE BRAIN, DOPAMINE AND GABA GABA (g-aminobutyric acid): INHIBITORY neurotransmitter Dopamine: the main EXCITORY neurotransmitter When GABA is high, dopamine levels are low (balanced) Release of dopamine causes powerful excitation of the brain. Amphetamines, cocaine, nicotine and heroin all increase dopamine levels (not all by the same mechanism, for example cocaine inhibits the re-uptake that normally occurs after the message has been sent). Vigabatrin (see Section 3) inhibits the enzyme that breaks GABA down, increasing GABA levels, which forces down dopamine levels ALCOHOL also appears to enhance the effect of GABA: ‘makes things sluggish’ ALCOHOL appears to weaken the effects of glutamine, another excitory neurotransmitter, presumably by occupying the receptors ORDER of ALCOHOL affects are: Cerebral Cortex (processes thoughts) Alcohol depresses the behavioural inhibitory centers: become more talkative, self confident, less socially inhibited Slows information processing: see, think, hear less clearly Limbic System (controls emotions) get angry, quiet, aggressive, withdrawn... Cerebellum (co-ordinates muscles) get less control, eg. touching finger to nose, balance... Other Effects of Alcohol: Hypothalmus (controls secretions of some hormones) increase sexual arousa inhibits secretion of the anti-diuretic hormone, which increases urination. Medulla (controls body functions like breathing) body temp falls, blood pressure falls, stop breathing! Stomach irritates lining, so vomiting; increases stomach acid Skin increases blood flow to skin (flushing) Muscles reduces blood flow (aches) Abuse: increases liver enzymes must drink more to feel the same effect nerve activity increases to compensate, but when not drinking causes irritability and delirium Get liver cell death, hardening of tissues: cirrhosis Get stomach ulcers Get higher blood pressure heart compensates for initial lowering GETTING RID OF ALCOHOL Kidneys eliminate ~5% in urine Lungs eliminate ~5% in breath (BREATHALYSER) Liver oxidizes most: 1 CH3CH2OH 2 CH3CHO CH3CO2Excreted, fat build-up 1 Alcohol dehydrogenase (cytochrome P450 type) NAD co-enzyme (forms NADH) 2 Aldehyde dehydrogenase (oxidation) Heavy drinkers build up more P-450 type enzymes: greater tolerance BUT ALSO get more fat deposition and scarring of the liver (CIRRHOSIS) Apr 2001 study reports men increase alcohol dehydrogenase 2x faster than women: greater liver damage Building up too much NADH also starts non-normal biochemical pathways: CH2OH HO abnormal HO NH NADH COOH CHO normal NH HO NAD serotonin aldehyde nerve cell ends CH3CHO can react with many amines; possibly responsible for hangovers NH DISULFURAM [Antabuse] inhibits aldehyde dehydrogenase leads to acetaldehyde buildup; if you drink you vomit, get headaches, chest pains....(effective but not a lot of fun!) Oral naltrexone [Revia, 1994]: reduce drink cravings Vivitrol is naltrexone embedded in polymer microspheres for once monthly injections Nalmefene is approved in US (mainly for heroin addicts) HO HO Et S N Et Et S S O N S O OH N Et OH N O Disulfuram Naltrexone Nalmefene FETAL ALCOHOL SYNDROME 1972- U. Washington Alcohol crosses placenta, but baby lacks liver enzymes, so levels in baby stay ~ 2x those in mother ALCOHOL is a TERATOGEN -affects development of fetus -DAYS 18-50 CRITICAL small heads joint-limb abnormalities heart-genital defects Symptoms: upper lip vertical groove absent upper lip thin nose short flattened brief attention spans mental retardation hyperactivity ~4000 children born per year with FAS in Canada (ca. 1 per 1000 live births) Depressants (downers) Sleeping Pills - Barbiturates Bayer first made barbituric acid in Germany in 1864 from urea and malonic acid (apples) O HOOC NH2 + O NH2 Urea HOOC R1 R2 - 2H2O NH R1 NH R2 O O R1 = R2 = H Barbituric acid Malonic acid no acid group! Barbituric acid itself is not active, but use of substituted malonic acids does give active ones Divided by length of action: LONG ACTING activation: 30-60 min duration: 6-12 h Phenobarbital (LUMINAL) R1, R2 = Et, Ph [1912 anti convulsant for epileptics] INTERMEDIATE activation: 30 min duration: 3-6 h Amobarbital (AMYTAL) R1, R2 = Et, i-pentyl Butabarbital R1, R2 = Et, sec-butyl Talbutal R1, R2 = allyl, sec-butyl Barbital (VERONAL) R1, R2 = Et, Et [used to put euthanize dogs since 1903] 2001: Kodiak, Alaska Eagles stagger ‘drunk’: had eaten cats from local dump – vets had euthanized cats with barbiturates but had not cremated or buried! ‘Blue Birds’ SHORT ACTING activation: 15 min duration: < 3 h Pentobarbital (Nembutal) [Yellow Jackets, Goof Balls] R1, R2 = Et, sec-pentyl Secobarbital (Seconal) [Red Devils, Red Birds] R1, R2 = allyl, sec-pentyl ULTRA-SHORT activation: < 10 sec duration: < 30 min Thiopental (PENTOTHAL) Na+ salt increases solubility Used as a quick knockout before an operation in tandem with a longer lasting anaesthetic O ONa N N Et NaO S s-Pentyl NH N O O Thiopental Methohexital Methohexital (BREVITAL): <7 secs ~ 7 mins recovery more rapid than pentothal, dose 1mg/kg ACTION (next slide) Barbiturates (and valium) ENHANCE the action of GABA (g-aminobutyric acid) in suppressing dopamine (the brain activator) All excitable nervous tissue is depressed, BUT CNS is especially affected THUS respiratory depression (controlled by brain) is the OVERDOSE mechanism NO blood-brain barrier, so short acting are the most dangerous. About 1000 accidental + 3000 suicides per year in US The diazepams bind close to the GABA receptor and increase the affinity of GABA for its receptors, which diminishes the excitation of nerves; it also alters rate of peptide formation in neurons, which induces amnesia. This is potentiated by alcohol. ANTIDOTES: need a stimulant eg. ephedrine Remain in blood stream for > 24 h (driving) Body develops tolerance - same enzymes as alcohol Doses > 400mg per day cause severe withdrawal: irritability, insomnia, convulsions, delirium ANESTHETICS Act on brain to produce unconsciousness and insensitivity to pain Pre-1860 Alcohol 1846 Diethyl Ether (CH3CH2)2O Morton, a Boston dentist, safe because of large gap between effective and toxic dose, BUT EXPLOSIVE with air, flammable and causes nausea 1847 Chloroform CHCl3 Non-flammable, but much smaller safety gap - hard on liver; Queen Victoria used it in childbirth 1869 Chloral hydrate (Mickey Finn’s) CCl3CH(OH)2 from Cl2 and alcohol; movie knock out drops 1896-1903, Whisky row in Chicago: ‘Lone Star house girls’ gave to their customers to sedate them to remove cash! 1880 Laughing gas N2O (use 1:1 with O2; brain damage with air!) Still in wide use, non-toxic, no odor (food aerosol cans – fat soluble) - some giddiness/exhilaration 1934 Cyclopropane very potent, but very flammable, not used now (1964 explosion killed 6) MODERN ONES: many halogenated ethers Desflurane HCF2-O-CF2CF2H Isoflurane HCF2-O-CHClCF3 Enflurane HCF2-O-CF2CHFCl Sevoflurane CF3-CH(OCH2F)-CF3 Methoxyflurane CH3-O-CF2CHCl2 Halothane CF3-CHBrCl irritating but short acting, BP up easy to inhale easy to inhale, BP down They have different MAC Minimum Alveolar Concentrations: conc. at which 50% of humans cease to feel pain eg. Desflurane (Suprane) = 6% in 100% O2 Typical anesthetic sequence: Prior to injection: muscle relaxant like succinylcholine to partially block the acetylcholine sites - allows less anesthetic to be used and no muscle spasms CH2COOCH2CH2NMe3+ CH2NMe3+ -OH 2Cl- CH2COOCH2CH2NMe3+ succinylcholine CH2OCOCH3 acetylcholine sometimes also a tranquilizer (valium) and an injection of atropine to dry up secretions Anesthetic administered: Quick knockout: pentothal (sometimes fentanyl) Keep patient out: 3% isoflurane in 50-70% N2O - rest O2 ACTION stops acetylcholine from working: saturates nerve endings, maybe involving a shape change RECOVERY slow by diffusion of the agent out via breathing usually sick for several hours; take two days to fully eject LOCAL ANESTHETICS 1860 Cocaine ( but name applies to family) PABA esters H2N CO2Et H2N benzocaine para-aminobenzoic acid (ethyl ester) CO2CH2CH2NHEt2+ -Cl procaine paba-(choline ester) Topical: Benzocaine: sunburn creams, sprays, throat lozenges, insect bites Dental: Procaine (Novocaine) 350-600 mg (injection) needs a vasoconstrictor (e.g. epinephrine ~ 1 in 105) otherwise too quickly absorbed away from injection site Since 1948 the more powerful amides have been used N NHCONHEt+ -Cl lidocaine NHCO mepivacaine Lidocaine [Abbott]; Xylocaine [Astra] (120-200 mg) amides hydrolyze more slowly than esters: don’t need vasoconstrictor Mepivacaine (Carbocaine, Isocaine) 400mg (once only) can block whole jaw for 20-40 mins Speciality: BuNH CO2CH2CH2NHMe2+ -Cl tetracaine PrO H2N CO2CH2CH2NHEt2+ -Cl proparacaine Tetracaine (Pontocaine) 5-20mg as spinal anesthetic, lasts 2-3 h Proparacaine (Opthaine) for ophthalmic use These all appear to alter the membranes of the nerve cells, stopping Na+ passage, stopping the impulses. TRANQUILIZERS BENZODIAZEPINES (Valium types) R N O Y Z N A B Name R Z Y A B Diazepam (Valium) CH3 Cl H H H Lorazepam H Cl OH Cl H Flurazepam -CH2CH2NEt2 Cl H H F Flunitrazepam CH3 NO2 H F H VALIUM = diazepam: oral dose 2-30mg 5mg valium = ‘0.08’ blood alcohol in terms of driving Injection for minor surgery: no feeling or memory Generic lorazepam (ATIVAN) most popular (2, 5, 10 mg) Flunitrazepam = ROHYPNOL ‘ the date rape drug’ available in Europe, Mexico, S. America for insomnia - now made BLUE With alcohol: unconscious in ~30 mins, lasts ~ 12h, no memory of incident NOTE: GHB g-hydroxybutyric acid HOCH2CH2CH2COOH also known as date rape drug recently Ketamine (an approved Canadian anesthetic + vet) has has appeared on streets (controlled substance!) Cl O Known as Special K,..... get ‘spaced out’, hallucinations like ‘near death experiences’ NH liquid (iv, smoked,...) crystals (.HCl salt) inj, snorted,... Benzodiazapine receptors directly located in brain and do not affect other tissues (see slide 20 of this section for mechanism: Half-lives in body of 1-3 days! Withdrawal symptoms can persist for 3-4 weeks(!): anxiety, restlessness, bizarre dreams Side effect: some patients get orgasms - prompts complaints of fondling, etc. Safer than the barbiturates: more difficult to overdose CARBAMATES H2N-CO-OR R= -CH2 CH2OCONH2 mepbromate -CH2 CH2OCONH-iPr soma Mepbromate (Equanil, Miltown) 400mg Soma 350 mg Both are also used as muscle relaxants, eg. in back pills act more like barbiturates as sleeping pills, but depress respiratory center less, so suicide or overdose less likely ROBAXIN (methocarbamol) 500/750 mg most common back-ache medication CH3O (skeletal muscle relaxant) O O O NH2 OH Often sold in combination, egs. Robaxacet = methocarbamol + acetaminophen Robaxisal = methocarbamol + ASA Robaxisal-C = methocarbamol + ASA + codeine Seem particularly safe: adults have been known to consume 30-50 g/day (!!) with no serious effects.