* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Appropriate use of antimicrobial agents
Onchocerciasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Neonatal infection wikipedia , lookup
Bioterrorism wikipedia , lookup
Leptospirosis wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
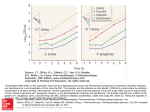
Appropriate use of antimicrobial agents Dr Olga Perovic, CMID/NHLS/WITS 2009 Introduction • Since evolution of antimicrobials large number of agents are available. • But their administration may be create unnecessary effects: – Antimicrobial overuse – Antimicrobial resistance – Inappropriate use • No organism identification • No susceptibility testing • No host factors taken in consideration when antimicrobials chosen. 5/23/2017 How to choose the appropriate antimicrobial agents? 1. The right antibiotic for disease. 2. Antibiotic should have the most narrow spectrum of activity for particular disease. 3. Administration of antibiotics according to severity of disease and host factors. 4. To consider the ways that body handles a drug? 5. To avoid unwanted effects of the drugs? 6. Duration of the treatment. 7. Antibiotic that is less likely to select for resistance. 8. Antibiotic that cure the patient. 5/23/2017 1. The right antibiotic for disease • What is needed? – Consider mechanism of activity. • Bactricidal activity, • Bacteriosatic activity. 5/23/2017 What is right direction? •Bacteriocidal –Mechanism of action •Antibiotics break down cell wall. •Antibiotics that prevent DNA synthesis. •Bacteristatic –Mechanism of action •Antibiotics that inhibit protein synthesis. •Antibiotics that inhibit nucleotide synthesis. •Antibiotics that replace essential metabolites. Organisms that are causes of severe disease such as meningitis, endocarditis should be treated with bactericicdal agents. 5/23/2017 2. The most narrow activity of selected antibiotic for disease • Can we determine right agent? – Laboratory testing • Submit specimen from correct site of infection. • Isolate an infectious organism • Identify and perform. susceptibility. • Show serological rising of titer for disease. 5/23/2017 MIC/MBC and correlation with disk diffusion method 5/23/2017 3. How to administer antibiotic? •Route of administration –Oral –IM –IV –Subcutaneus 5/23/2017 •Penetration of antibiotics at site of infection in high concentration. •Host factors –Age –Pregnancy –Genetic abnormalities –Renal and hepatic dysfunction –Site of infection. 4. What are the ways that body handles a drug? • • • • 5/23/2017 Absorption Distribution Metabolism Excretion Example of absorption of antibiotics from the gastrointestinal tract Well absorbed Poorly absorbed Not absorbed Penicillin V Penicillin G Aminoglycosides Amoxicillin Ampicillin Vancimycin Cloxacillin Methicillin Carbapenems Oral cephalosporins: Cephalexin, Cefuroxime Cefixime Cefpodoxime Quinolone Chloramphenicol Azithromycin Clarithomycin Erythromycin Doxicycline Tetracycline 5/23/2017 5. Duration of treatment • Short – To treat as long as is clinically indicated. Once patient is better to stop treatment. • Long – Until organism is eradicated. – Certain conditions that need long duration: • Endocarditis • Cystic fibrosis • Bone and joint infections. 5/23/2017 6. Unwanted effects • Special attention for patients with – Renal failure. – Hepatic failure. – Neutropenic patients. – Allergy. 5/23/2017 7. Characterization of bacterial resistance to antibiotics • Genetics versus parental strain. • Biochemical (presence or absence of a resistance mechanism). • Microbiologic (elevated MIC). • Clinical (therapeutic outcome). • Intrinsic (present in all members of a given genus or species). • Acquired (present only in certain isolates of a genus or species). 5/23/2017 Resistance to antibiotics ß-lactamases in gram-negative ß-lactamases in gram-positive ß-lactam PBPs and altered PBP Efflux pump Porins 50 30 Permeability Methylation of the 23S rRNA changes 50S rRNA result is no binding of macrolides 5/23/2017 Linezolid-mutation of 23S rRNA gene specific for S. aureus and E. faecalis 7. Antibiotics that most likely select for resistance! • Antibiotics that causes “collateral damage” – Cephalosporins – Quinolones 5/23/2017 8. What drug does to the body? • Pharmacodynamic feature of antibiotics. – An antimicrobial agent may inhibit growth and replication (static effect) or cause bacterial cell death (cidal). – Concentration is important (one antibiotic may be bacteriosatic at low concentration but bactericicdal in high concentrations. • Pharmacodynamics relationships – Concentration-dependent killing agents – Time-dependent killing agents – Activity of antibiotics measured by MIC (minimum inhibitory concentration). 5/23/2017 AUC/MIC ratio •Cmax/MIC ratio-the maximum serum concentration of the drug (Cmax) divided by the MIC. Predict efficacy and development of resistance. AUIC is AUC/MIC ratio- the area under the 24-hour serum concentration curve (AUC) divided by the MIC. A predictor of bacterial/clinical success. Cmax and AUC are covariant: when Cmax increases, AUC increase also. •Time above MIC (T>MIC). The time that serum drug concentrations stay higher than the MIC for the organism. 5/23/2017 The pharmacodynamic properties of major antibiotic groups Pd ß-lactams aminoglycosides macrolides fluoroquinolones Timedependent killing +++ +/- +++ + Concentration dependent killing +/- +++ + +++ Best predictor of response Time above MIC Cmax/MIC ? AUIC 5/23/2017 Summary-kill the bug! • Facts: appropriate therapy saves lives! • Actions: – Diagnose and identify the etiologic agent – Culture the patient’s specimen(s). – Target EMPIRIC therapy to likely pathogens based on hospital antibiogram. – Target DEFINITIVE therapy based to accurate identification of organism/s and susceptibility (MIC) RESULTS. – Monitor therapy outcome. 5/23/2017