* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
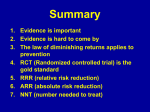
The Use Of Adjuvants In Pain Management Stewart W. Stein, M.D. Medical Director, Good Shepherd Hospice Objectives • Understand basic principles of pain transmission • Understand the role of adjuvants in the management of pain • Understand advantages and disadvantages of various agents in the management of chronic pain • Understand the use of other modalities in pain management. Ascending Pathways • A-delta fibers are myelinated (insulated with a myelin sheath). The pain is fast and well localized, like the initial prick or stinging sensation following an injury. • C fibers are nonmyelinated and smaller than A-delta fibers. They transmit pain much slower. The pain is more lasting, generalized and described as a dull ache. 3 Ascending Pathways • After afferent A-delta (myelinated and fast) and C-fibers (unmyelinated and slow) synapse with the interneurons. • These cross over to the contralateral side and ascend primarily via the spinothalamic tracts to the thalmus and cortex. Ascending Pathways 5 Pathophysiology • Nociceptor activation / Types of receptors: • Mechanical • Thermal • Chemical • Respond to stimuli that approach or exceed harmful intensity by undergoing conformational, electrical and biochemical changes WHO Pain Ladder 7 • Adjuvant Analgesics Adjuvant Analgesics • “Non-opioids with analgesic efficacy” • Primarily used to treat neuropathic pain syndromes although also effective in management of nociceptive pain when used as adjuvants to other medications Adjuvant Analgesics Step 1 Agents on the WHO ladder • Non-steroidal anti-inflammatories (NSAIDS) • Antidepressants (TCA’s) • Anticonvulsants / Antiepileptics (AED’s) • Cortisteroids • Bisphosphonates • Anesthetics • N-Methyl D-aspartate antagonists (NMDA) Acetaminophen / Paracetamol • Mechanism of action unclear but may inhibit cyclooxygenase in the CNS • Acetaminophen can cause liver damage if dose exceeds 4 grams a day • Risk of hepatic injury is increased in patients having pre-existing liver damage (alcoholism, hepatitis) • Acetaminophen has also been shown to cause renal damage. NSAIDS • Mechanism of action is the inhibition of cyclooxygenase to decrease prostaglandin synthesis • May have central action at the spinal cord level • They do have a ceiling effect • Tolerance and physical dependence is NOT seen! • Can be associated with end-organ toxicity Neuropathic Pain Syndromes Trigeminal neuralgia Post-herpetic neuralgia Diabetic neuropathy Chemotherapy-induced neuropathy Plexopathies Phantom limb pain Complex regional pain syndrome Central post-stroke (damage to thalamus, cortical or subcortical structures) Syringomyelia Sympathetically maintained pain syndrome (RSD) Adjuvant Analgesics • Tricyclic Anti-depressants • Inhibit reuptake of norepinephrine and serotonin in nerve endings in the spinal cord and in the brain • NMDA antagonism Antidepressants • Tricyclic Antidepressants • Tertiary amines: • • • • amitriptyline doxepin imipramine clomipramine • Secondary amines: • desipramine • nortriptyline Antidepressants • Serotoninergic agents • • • • • Fluoxetine Paroxetine Sertraline Citalopram Escitalopram Antidepressants • SNRI’s (serotonin / norepinephrine reuptake inhibitors) • Venlafaxine • Desvenlafaxine • Duloxetine Antidepressants • Used for: • • • • Analgesia Depression Insomnia (even pruritis) Antidepressants: • Mechanism of action is inhibition of reuptake of neurotransmitters (serotonin, norepinephrine and dopamine) • Only tricyclic antidepressants have analgesic properties independent of their antidepressant activity Antidepressants: Side Effects • • • • • • • Nausea Sedation Confusion Xerostomia Tachycardia Drug interactions (Anticholinergic ) Side Effects of TCA’s ?MI • Long term use of TCA’s is associated with a 2.2 relative risk of myocardial infarction and a 1.7fold increase in mortality vs. placebo or SSRI’s. (screen elderly with EKG?) • American Journal of Medicine (2000) Jan;108(1):2-8 • European Heart Journal (2004) 25 (1): 3-9 AED’s (Antiepileptic Drugs) Mechanism of action of AED’s: • Slow recovery of voltage gated Na channels from depolarization (carbamazepine, phenytoin) • Indirect or direct enhancement of inhibitory Gama-aminobutyric acid neurotransmission (Valproic acid, Tiagabine) • Inhibition of excitatory glutamatergic neurotransmission (lamotrigine) Mechanism of action of AED’s • Block voltage dependent Ca++ channel (Gabapentin and Pregabalin) • Carbonic anhydrase inhibition (Topiramate, Zonisamide) Mechanism of action of AED’s: 25 New AED’s (Anti-Epileptic Drugs) • • • • • • • • Gabapentin Topiramate Levitiracetam Tiagabine Oxcarbazepine Lamotrigine Felbamate Pregabalin Use of AED’s: • Start with a low evening dose • Increase GRADUALLY over 4-6 weeks depending on response. (Typically effective at higher doses) New AED’s Side Effects • • • • • • • • Drowsiness Unsteadiness Aplastic anemia (CB) Dizziness Confusion Rash (VPA) Ataxia Nausea and vomiting Gabapentin • Established efficacy in treatment of post herpetic neuralgia • Most common mistake is failure to titrate to effective doses (900mg ineffective in managing PDN in one series) Gabapentin • Titration Schedule: • Day 1: 300mg po at HS • Day 2: 300mg po bid • Day 3: 300mg po tid • Titrate 100-300mg per day over next 2 weeks to target dose of 1800mg. Continue titration over 2 more weeks to 3600mg if indicated for effect. Higher doses have also been successfully used. Pregabalin • Advantages include predictable absorption across the GI tract. Not metabolized or protein-bound. Minimal drug-drug interactions. • Multiple studies demonstrate effective pain relief and decreased sleep interference in PHN and PDN Pregabalin • Dosing schedule • Days 1-3: 50mg po tid • Days 4-7: 100mg po tid • Thereafter 200mg po tid. • Taper dose over 7 days to discontinue Lamotrigine • Demonstrated efficacy in trigeminal neuralgia. • Utility in vascular HA’s and PDN suggested by open label studies Lamotrigine • Dosing: • Start at 25-50mg po daily • Increase by 50mg per day per week until effective or an arbitrary maximum is reached (usually around 900mg daily in 2-3 divided doses) Topiramate • Studies demonstrate utility in management of cluster headache and diabetic neuropathy • Effective dose range is 200-400mg daily in divided (2) doses • Associated with weight loss • Side effects may include abnormal thinking, delusional and psychotic thinking, kidney stones. Carbamazepine • Used in trigeminal neuralgia since the 1960’s! • Starting dose is 200mg po bid. Effective dose is usually 400-1000mg per day. • Induces P450 system so potential for drugdrug interactions. • Aplastic anemia occurs in 1:200,000. More commonly, a reversible leukopenia or thrombocytopenia may occur. Oxcarbezapine • An analog of carbamazepine that retains many therapeutic properties of the drug while avoiding toxicities. (No bone marrow suppression or induction of P450 system) • Start with 300mg at HS. Increase weekly by 300-600mg until effective up to a maximum of 1200-2400mg per day. Phenytoin • Mixed results in trials (1970’s) for PDN. • Usual dose 200-400mg po daily • Side effects include nausea, diplopia, dizziness, confusion, gingival hyperplasia and rarely Stevens-Johnson syndrome. • Induces P450 cytochrome system Valproic acid • Demonstrated efficacy in migraine HA’s. • Side effects include nausea, vomiting, sedation, rash, ataxia and appetite stimulation • 40% develop increased transaminases. • 1:50,000 will develop HEPATIC FAILURE Also part of the equation …. • NNT: The number of patients that need to be treated with a particular drug in order for one patient to experience a 50% reduction in pain • NNH: The number of patients that need to be treated with a particular drug in order for one patient to drop out due to adverse effects TCA (amitriptyline) • NNT = 2-3 • NNH = 14.7 AED (gabapentin) • NNT = 5.1 (Includes all doses, high and low) • NNH = 26.1 Opioids • Morphine NNT = 2.5 • Oxycodone NNT = 2.6 • Tramadol NNT = 3.9 • NNH for tramadol = 9.0 • NNH morphine and oxycodone = not significant Bisphosphonates • Pamidronate and Zolendronic acid • Localize to bone and inhibit osteoclastic activity • Widely studied in treatment of metastatic bone pain • Risk of osteonecrosis of the mandible. Corticosteroids • Inhibit arachodonic acid (prostaglandin synthesis) resulting in anti-infalmmatory action • Also a membrane stabilizer (blocking cfiber transmission) NMDA Receptors • Located mostly in the dorsal horn of the spinal cord • Activated by chronic, painful stimulus leading to allodynia, hyperalgesia, and neuropathic pain. • Also responsible for opioid tolerance. Therefore: • Blocking NMDA results not only in improved pain control but also reverses opioid tolerance to varying degrees. NMDA receptor antagonists: • Methadone • Ketamine • Dextromethorphan Ketamine • Useful in refractory neuropathic pain states • Useful to “reset” opioid sensitivity in an opioid-tolerant patient • Also very useful for procedures such as painful wound care Neuropathic pain: How do we proceed? • If we were to look only at pain relief, the order would be: TCA opioids tramadol gabapentin / pregabalin (recall NNT) BUT…. • If criteria are to be both relief of pain AND quality of life, the order would be: Gabapentin / pregabalin Tramadol Opioids TCA’s Nerve Blocks: Celiac Plexus Block • Used with upper abdominal malignancies • Variable benefit • (alcohol neurolysis most common) Nerve Blocks: Mandibular / Maxillary / Gasserian ganglion block • Used in head and neck cancer pain. Phenol / alcohol used for neurolysis • Radiofrequency ablation also used • Post neurolytic dysesthesia can occur Axial therapy • Both presynaptic and post synaptic opioid receptors within the dorsal horns of the spinal matter inhibit synaptic transmission from the peripheral afferent nociceptor to the second order spinal neuron. Axial Therapy • Intrathecal • subarachnoid • Epidural • requires 10 times the intrathecal volume to spread medication over several dermatomal segments Axial Therapy • Advantages: • Effective • Markedly reduced side effects. • Disadvantages: • • • Surgical procedure Infection CSF leak Axial vs. Oral Opiate Dosing • • • • Oral morphine = 300mg IV morphine = 100mg Epidural = 10mg morphine Intrathecal = 1mg morphine Other Modalities Vertebroplasty • Cement (polymethyl methacrylate) is injected into the damaged vertebra and acts as an internal splint. Useful in osteoporosis and cancer-associated fractures Other Modalities • TENS • Stimulates large “A” fibers that then close the gate for pain coming in from “C” fibers. Used in acute and chronic pain syndromes. • Low intensity: not reversed by naloxone • High intensity: reversed by naloxone Other Modalities • Acupuncture: Possibly acts on reward center (dopamine and serotonin) • May increase muscle blood flow • May reduce gastric acid and correct gastric arrhythmia, thereby reducing nausea and vomiting. Questions & Comments