* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pharmacokinetics & Pharmacodynamics
Nicotinic agonist wikipedia , lookup
Orphan drug wikipedia , lookup
Compounding wikipedia , lookup
Plateau principle wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Drug discovery wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Drug design wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
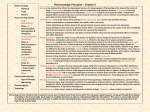
Principles of Pharmacology Pharmacokinetics & Pharmacodynamics Pharmacokinetics Movement of drugs in the body Four Processes Absorption Distribution Metabolism Excretion Drug concentration at sites of action influenced by several factors, such as: Route of administration Dose Characteristics of drug molecules (e.g., lipid solubility) Drug Absorption Routes of Drug Administration Oral (per os, p.o.) Inhalation Mucous membranes intranasal (sniffing) sublingual rectal suppositories Injection (parenteral) vapors, gases, smoke intravenous (IV) intramuscular (IM) subcutaneous (SC) intraperitoneal (IP; nonhumans only) Transdermal DRUG ABSORPTION Lipid solubility pKa = pH at which 50% of drug molecules are ionized (charged) Only uncharged molecules are lipid soluble. The pKa of a molecule influences its rate of absorption through tissues into the bloodstream. pH varies among tissue sites e.g., stomach: 3-4, intestines: 8-9 pKa and Lipid Solubility Image from McKim, 2007, p. 14 Routes of Drug Administration Oral Drug Administration Advantages: relatively safe, economical, convenient, practical Disadvantages: Blood levels are difficult to predict due to multiple factors that limit absorption. Some drugs are destroyed by stomach acids. Some drugs irritate the GI system. Routes of Drug Administration Advantages of Injection Routes Absorption is more rapid than with oral administration. Rate of absorption depends on blood flow to particular tissue site (I.P. > I.M. > S.C.). Advantages specific to I.V. injection No absorption involved (inject directly into blood). Rate of infusion can be controlled. A more accurate prediction of dose is obtained. Routes of Drug Administration Disadvantages/Risks of Injection A rapid onset of action can be dangerous in overdosing occurs. If administered too fast, heart and respiratory function could collapse. Drugs insoluble in water or dissolved in oily liquids can not be given I.V. Sterile techniques are necessary to avoid the risk of infection. Drug Distribution Cell Membranes Capillaries Drug affinities for plasma proteins Bound molecules can’t cross capillary walls Blood Brain Barrier Tight junctions in capillaries Less developed in infants Weaker in certain areas, e.g. area postrema in brain stem Cerebral trauma can decrease integrity Placenta Not a barrier to lipid soluble substances. Termination of Drug Action Biotransformation (metabolism) Liver microsomal enzymes in hepatocytes transform drug molecules into less lipid soluble by-products. Cytochrome P450 enzyme family Termination of Drug Action Elimination Two-stage kidney process (filter, absorption) Metabolites that are poorly reabsorbed by kidney are excreted in urine. Some drugs have active (lipid soluble) metabolites that are reabsorbed into circulation (e.g., pro-drugs) Other routes of elimination: lungs, bile, skin Termination of Drug Action Kidney Actions excretes products of body metabolism closely regulates body fluids and electrolytes The human adult kidney filters approx. 1 liter of plasma per minute, 99.9% of fluid is reabsorbed. Lipid soluble drugs are reabsorbed with the water. Termination of Drug Action Factors Influencing Biotransformation Genetic Environmental (e.g., diet, nutrition) Physiological differences (e.g., age, gender differences in microsomal enzyme systems) Drug Interactions Some drugs increase or decrease enzyme activity e.g., carbamazepine stimulates CYP-3A3/4 e.g., SSRIs inhibit CYP-1A2, CYP-2C Drug Time Course Time Course Studies important for predicting dosages/dosing intervals maintaining therapeutic levels determining time to elimination Elimination Half-Life time required for drug blood levels to be reduced by 50% Approx. 6 half-lives to eliminate drug from body With repeated regular interval dosing, steady-state concentration reached in approx. 6 x half-life Therapeutic Drug Monitoring TDM important for clinical decisions Plasma levels rough approximation of tissue/receptor concentrations TDM goals assess medication compliance avoid toxicity enhance therapeutic response Tolerance & Dependence Mechanisms of Tolerance Metabolic (Pharmacokinetic, Dispositional) Cellular-Adaptive (Pharmacodynamic) Behavioral Conditioning Dependence Abstinence Syndrome Not all addictive drugs produce physical dependence. Some nonaddictive therapeutic drugs (e.g. SSRIs) can produce physical dependence. Pharmacodynamics Drug actions at receptor sites and the physiological/chemical/behavioral effects produced by these actions Studies of drug mechanisms of action at the molecular level Provides basis for rational therapeutic uses and the design of new, superior therapeutic agents Drug-Receptor Interactions Receptors found on membrane spanning proteins Ligands (neurotransmitters, drugs) attach inside spaces between coils, held by ionic attractions Continuous series of amino acid loops Reversible ionic binding of ligand activates receptor by changing protein structure. Intensity of transmembrane signal is determined by percentage of receptors occupied. Drugs may influence transmembrane signal by binding to neurotransmitter receptor or to nearby site. Drug-Receptor Interactions Drug/Receptor Binding Mimic actions of neurotransmitter at same site (agonist) Bind to nearby site and facilitate neurotransmitter binding (agonist) Block actions of neurotransmitter at same site (antagonist) Receptor Structures Ion Channel Receptors Carrier Proteins G Protein-Coupled Receptors Enzymes Drug-Receptor Specificity Alterations to a drug’s chemical structure may influence potency e.g., amphetamine vs. methamphetamine Many drugs have multiple sites of action Some sites of action are responsible for side effects e.g., tricyclic antidepressants: sedation, dry mouth, blurred vision Dose-Response Relationships Potency Efficacy Dose-Response Functions Efficacy (ED50 = median effective dose) Lethality (LD50 = median lethal dose) Therapeutic Index = LD 50 /ED 50 100 100 Death Percent of Subjects Dead Percent of Subjects Sedated Sedation 75 50 25 0 75 50 25 0 0.01 0.1 1 Dose (mg/kg) 10 100 10 100 1000 Dose (mg/kg) 10000