* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapters 1 - Canadian Liver Foundation
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of HIV-protease inhibitors wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Theralizumab wikipedia , lookup
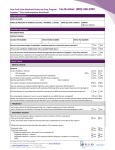
Protease Inhibitors in Chronic Hepatitis C: An Update COMPLETE SLIDE DECK (Chapters 1 – 6) Edited by Morris Sherman MD BCh PhD FRCP(C) Associate Professor of Medicine University of Toronto November 2012 Management of Hepatitis C: Updated Guidelines from the Canadian Association for the Study of the Liver (CASL) Robert P. Myers, MD, MSc Associate Professor, Liver Unit Division of Gastroenterology University of Calgary Objectives: HCV Management Review updated CASL recommendations for management of HCV genotype 1* Burden of HCV in Canada Pre-treatment assessment Triple therapy including boceprevir and telaprevir Adverse effects Drug-drug interactions Antiviral resistance * Recommendations for non-1 genotypes are unchanged from the 2007 CASL HCV guidelines. Burden of HCV in Canada Significant medical and economic burden Seroprevalence unknown Risk Group Population Prevalence Prevalent Cases Proportion of Cases 268,200 52% 140,000 58% Current IDU 84,400 62% 52,500 22% Previous IDU 183,800 48% 87,500 36% Transfusion 3,325,700 0.8% 25,900 11% Hemophilia 2,200 40% 900 0.4% Other 27,624,300 0.27% 75,800 31% Total 31,220,500 0.8% 243,000 100% IDU, total Remis RS. PHAC 2007 Burden of HCV in Canada Modelled incidence ~8,000 incident cases annually (80% IDUs) Proportion diagnosed unclear (<80%) HCV-related complications rising Insufficient manpower to treat all cases 900 Cirrhosis 800 700 600 Decomp 500 400 HCC 300 Transplant 200 100 0 1967 1972 1977 1982 1987 1992 1997 2002 2007 2012 2017 2022 2027 Year Remis et al. PHAC 2007 Liver-related death vs. no treatment (%) Antiviral Therapy Must be Maximized to Make an Impact 100 90 80% SVR rate 60% SVR rate 40% SVR rate 34% ↓ 80 68% ↓ 70 60 50 40 30 20 0 Current* 25% 50% 75% 100% Proportion of population treated * Assumes 30% Dx & up to 25% Rx’d in 2010. Outcomes at 2020. Davis GL et al. Gastroenterology 2010; 138(2):513-21 Burden of HCV in Canada: CASL Recommendations A large population-based seroprevalence survey should be conducted to accurately define the prevalence of hepatitis C in Canada. The design of the study should include populations with an increased risk of hepatitis C, particularly IDUs and immigrants from endemic countries. Increased resources are necessary to improve hepatitis C treatment capacity in Canada, including the training of expert treaters and public funding for treatment nurses. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Who Should Be Treated? CASL Recommendations Myers RP et al. Can J Gastro 2012; 26(6):359-75 Who Should Be Treated? CASL Recommendations All patients with chronic HCV, particularly those with liver fibrosis, should be considered candidates for antiviral therapy. Patients with extrahepatic manifestations of HCV should be considered for antiviral therapy. Persistently normal ALT does not exclude significant liver disease nor preclude the need for antiviral therapy. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Pre-Treatment Assessment: Is Liver Biopsy Really Necessary? Some fibrosis assessment necessary Prognosis Necessity of treatment Surveillance for HCC & varices F2 threshold less important with improved therapies Biopsy is imperfect Sampling error; variability in pathologic interpretation Numerous noninvasive alternatives to biopsy Bedossa P et al. Hepatology 2003; 38(6):1449-57 Pre-Treatment Assessment: Non-invasive Measures of Fibrosis Test (Reference) Components Cut-off F2-F4 vs. F0-F1 Sensitivity/specificity F2-F4 vs. F0-F1 FibroScan (Castera, 2005) Liver stiffness by transient elastography ≥7.1 kPa 67% / 89% APRI (Shaheen, 2007) AST/ULN x 100 Platelets ≥0.5 ≥0.7 ≥1.5 81% / 50% 84% / 70% 35% / 91% FibroTest (Poynard, 2004) α2M, haptoglobin, apo-A1, GGT, bilirubin ≥0.58 56% / 83% α2M, HA, TIMP-1 ≥0.36 77% / 73% α2M, HA, GGT, bilirubin ≥0.50 89% / 63% α2M, HA, AST, platelets, PT, urea ≥0.50 75% / 78% FibroSpect II (Patel, 2004) Hepascore (Adams, 2005) FibroMeter (Leroy, 2005) Pre-Treatment Assessment: CASL Recommendations Assessment of Disease Severity All patients with HCV should have an assessment for the severity of liver fibrosis. Acceptable methods include liver biopsy, TE (FibroScan), and serum biomarker panels (e.g. APRI, FibroTest, Fibrometer), either alone or in combination. Alternatively, cirrhosis can be confidently diagnosed in some patients with clear clinical or radiographic evidence. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Pre-Treatment Assessment: CASL Recommendations Virologic Testing HCV RNA and genotype testing are essential to the management of patients with chronic hepatitis C. HCV RNA testing should be performed using a sensitive quantitative assay (lower limit of detection ≤ 10-15 IU/mL) with a broad dynamic range. Standardized results should be expressed in IU/mL and be available within a maximum of 7 days in order to facilitate management decisions. Although genotype 1b has higher response rates vs. genotype 1a, testing for HCV subtype is not indicated This may change with newer DAAs available in the future Myers RP et al. Can J Gastro 2012; 26(6):359-75 Interleukin 28B (IL28B) Associated with viral clearance ~50% of ethnic variation in SVR rates Strongest pre-treatment predictor of SVR, but on-treatment response more important 100 P=1.06x10-25 80 SVR (%) Single-nucleotide polymorphisms (SNPs) on chromosome 19 Encodes IFN-λ3 P=2.06x10-3 P=4.39x10-3 P=1.37x10-28 Numbers on bars represent n 60 40 20 102 433 336 0 70 91 30 14 35 26 186 559 392 T/T T/C C/C T/C C/C T/C C/C T/C C/C EuropeanAmericans AfricanAmericans Hispanics Combined rs12979860 SVR (%) Non-SVR (%) Ge. Nature 2009. Suppiah. Nat Genet 2009. Tanaka. Nat Genet 2009. Thomas. Nature 2009. Pre-Treatment Assessment: CASL Recommendations IL28B Genotyping The IL28B genotype may provide valuable information regarding the likelihood of SVR and the probability of qualifying for shortened treatment duration in previously untreated patients with genotype 1. The role of IL28B genotyping is limited in treatmentexperienced patients and those with genotypes other than 1 and 4. A non-favourable IL28B genotype does not preclude antiviral therapy. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Antiviral Therapy for HCV Genotype 1: CASL Recommendations Triple therapy including peginterferon (PEG-IFN), ribavirin (RBV), and a protease inhibitor (telaprevir or boceprevir) is the new standard of care in treatment-naïve and previous treatment failures. Boceprevir (800 mg every 8 hours with food) is administered after a 4-week lead-in period of PEG-IFN and RBV. Duration of therapy depends on patient characteristics and treatment response. Telaprevir (750 mg every 8 hours with non-low fat food) should be started simultaneously with PEG-IFN and RBV and given for the initial 12 weeks of therapy. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Response-Guided Therapy (RGT): CASL Recommendations RGT - the tailoring of treatment duration based on early viral kinetics - can be employed in selected patient subgroups. Boceprevir: HCV RNA negative at weeks 8 through 24 Telaprevir: HCV RNA negative at weeks 4 through 12 SVR rates of ~90% have been reported with 24 to 28 weeks of therapy in patients qualifying for RGT. Partial responders treated with telaprevir, patients with cirrhosis, and prior null responders should not receive RGT. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Adherence to Antiviral Therapy: CASL Recommendations Adherence to treatment and to futility rules, and close monitoring of concomitant drugs and side effects are particularly important with PI-based therapy. Optimal management of this population should be conducted by well-trained, experienced personnel. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Futility Rules: CASL Recommendations Strict adherence to futility rules is vital to limit exposure to potential side effects of these costly therapies that will not achieve SVR, and to reduce emergence of antiviral resistance. All therapy – including PEG-IFN and RBV – must be discontinued if futility rules are met: Boceprevir: HCV RNA ≥100 IU/mL at week 12 or detectable at week 24 Telaprevir: HCV RNA >1,000 IU/mL at week 4 or 12, or detectable at week 24 Identical futility rules apply to treatment-naïve and treatment-experienced patients. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Futility Rules Indicate Treatment Failure Even if the Viral Load Has Declined 107 1,800,000 HCV RNA (IU/mL) 106 99.9% reduction: Continue? 105 104 1,230 103 475 102 If futility rules met, RNA is rising! Stop therapy! 10 1 W0 W1 W2 W3 W4 Slide courtesy of Dr. J. Feld. Adverse Effects of the Protease Inhibitors (PIs) PI-based therapy associated with more adverse effects than PEG-IFN and RBV dual therapy No data to support switching from one PI to another to manage toxicity Major adverse effects differ by PI Boceprevir: anemia (~50%), dysgeusia (~40%) Telaprevir: anemia (~40%), rash (~40%), anorectal symptoms (~30%) Myers RP et al. Can J Gastro 2012; 26(6):359-75 Adverse Effects of the Protease Inhibitors (PIs): CASL Recommendations Treatment with PIs should be supervised by experienced personnel and adverse effects monitored closely. Close monitoring of hemoglobin levels is essential during antiviral treatment for HCV, particularly during the administration of PIs. Management of anemia may include any of the following strategies: RBV dose reduction (first line), transfusion of packed red blood cells, and/or erythropoietin administration. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Drug-Drug Interactions (DDIs) Boceprevir and telaprevir are substrates and inhibitors of CYP3A4* CYP3A4 metabolizes many common drugs Potential increased drug concentrations with PI coadministration Drugs that induced CYP3A4 may reduce PI concentration (i.e. antiviral treatment efficacy) Numerous potential DDIs with PI-based therapy Antiarrhythmics, anticoagulants, anticonvulsants, antihistamines, antibacterials, antiretrovirals, statins, herbal products, immunosuppressants, OCPs, phosphodiesterase inhibitors, and some sedatives/hypnotics * Minor elimination pathways include P-glycoprotein and aldoketoreductase. Drug-Drug Interactions (DDIs): CASL Recommendations Prior to the initiation of PIs, potential DDIs must be considered, including those attributable to prescription and over-the-counter pharmaceuticals and herbal preparations. Review product monographs and useful online resources for potential DDIs prior to initiating therapy. http://www.hep-druginteractions.org/ http://medicine.iupui.edu/clinpharm/ddis/ Myers RP et al. Can J Gastro 2012; 26(6):359-75 Antiviral Resistance HCV RNA change from baseline (Log10 IU/mL) All resistance variants pre-exist Not caused by PIs, but unmasked by selective pressure Reflect inadequate response to PEG-IFN/RBV Predominant cause (80-90%) of incomplete viral suppression, breakthrough, or relapse Genotype 1a > 1b 1 Modest or null IFNa-ribavirin effect 0 -1 -2 Resistant HCV -3 -4 Wild-type, sensitive HCV -5 Study time Pawlotsky JM. Hepatology. 2011 May; 53(5):1742-51 Antiviral Resistance: CASL Recommendations In order to reduce the development of antiviral resistance to the PIs, patients who meet futility rules indicating a high likelihood of treatment failure should discontinue therapy immediately. Dosage reductions of boceprevir and telaprevir should not be utilized to manage treatment-related side effects. To prevent resistance, PIs must be stopped if either PEG-IFN or RBV are discontinued. There is no role for pre-treatment resistance testing. Myers RP et al. Can J Gastro 2012; 26(6):359-75 Summary: CASL Guidelines for the Management of HCV Must maximize case-finding, referral, and antiviral Rx to reduce HCV burden in Canada. Barriers to treatment (e.g. need for biopsy) should be minimized. New therapies (boceprevir and telaprevir) markedly improve SVR rates in genotype 1 (treatment-naïve and experienced), but are complex and have additional side effects. Important Hepatitis C Protease Inhibitor Drug Interactions in Mono and HIV Coinfection Alice Tseng, Pharm.D., FCSHP, AAHIVP Toronto General Hospital University of Toronto Outline Review principles of drug interactions Understand how the pharmacology of DAAs contribute to drug interactions Highlight important HCV drug interactions Outline a strategy for identifying and managing drug interactions Identify pertinent HCV drug interaction resources Drug Interactions Pharmacodynamic Change in pharmacological effect of a drug Additive, synergistic, or antagonistic activity or toxicity e.g., ribavirin + AZT = anemia Pharmacokinetic Change in the amount of drug(s) in body Absorption, distribution, metabolism, elimination may be affected Often involves CYP450 system or transporters Interactions Affecting Drug Metabolism Majority of drugs transformed to inactive forms prior to elimination through Phase I (oxidation) or Phase II (conjugation) reactions Phase I primarily involves cytochrome P450 system Superfamily of microsomal heme-containing enzymes Primarily located in liver, small bowel; also kidney, lung, brain CYP3A is the most abundantly expressed isoenzyme, is involved in the metabolism of ~50% of clinically used drugs others: CYP2D6, 2C9, 2B6, 1A2, etc. P-glycoprotein Efflux membrane transporter which prevents drug accumulation in cells; has broad substrate specificity, and inhibiting or inducing the activity of this protein can lead to significant alterations in drug exposure Terms Definition Interaction Impact Common Examples Substrate Agent which is primarily cleared via a certain enzymatic pathway Rate of drug breakdown is affected by presence of enzyme inhibitors or enzyme inducers antidepressants, azoles, benzodiazepines, statins, corticosteroids, calcium channel blockers, macrolides, rifamycins, HIV PIs & NNRTIs Inhibitor Agent which competes with another drug for binding at enzymatic site Decreased clearance macrolides, azoles, HIV of substrate drug; quick protease inhibitors onset & resolution of interaction effect Inducer Drug that stimulates the production of additional metabolic enzymes Increased clearance of substrate drug; slower onset and resolution of interaction effect anticonvulsants, rifamycins, HIV NNRTIs, St. John’s wort Boceprevir and Telaprevir Pharmacology Boceprevir Telaprevir Dosing 800 mg q8h with food 750 mg q8h with food (20 g fat) Substrate CYP3A4, P-gp, AKR CYP3A4, Pgp 3A4, P-gp 3A4, P-gp, renal transporters (?) Inhibitor Inducer No inducing effects in vitro (in vivo?) = +++ potential for interactions with other drugs can be clinically significant sometimes unpredictable Potential Consequences of DAA Drug Interactions Interactions may occur in a two-way manner: Concentrations of DAA may be altered by other drug(s) Concentrations of concomitant drug(s) may be altered by DAA Potential consequences include: Increased risk of toxicity Decreased efficacy Statin Interactions Most statins are P450 substrates DAAs can significantly increase statin levels: Atorvastatin: 130% with boceprevir, 7.88-fold with telaprevir Pravastatin: 60% with boceprevir risk of toxicity, including myopathy and rhabdomyolysis Boceprevir Lovastatin, Simvastatin Telaprevir CONTRAINDICATED Atorvastatin May need to atorvastatin dose; do not exceed >20 mg/d CONTRAINDICATED Pravastatin Start with recommended dose and monitor for toxicity. Possible in statin; use with caution. Rosuvastatin, Fluvastatin Possible in statin; use with caution. [Victrelis & Incivek Product Monographs, 2011. FDA HIV/AIDS Drug Safety Communication, March 1, 2012] Atorvastatin Interactions with Boceprevir and Telaprevir Atorvastatin 20 mg + telaprevir: Atorvastatin AUC 7.88-fold 30,000 100 25,000 Atorvastatin alone Atorvastatin + Boceprevir 20,000 15,000 10,000 5,000 Concentration (ng/mL) Atorvastatin concentration (pg/mL) Atorvastatin 40 mg + boceprevir: Atorvastatin AUC 130% and Cmax 170% vs. atorvastatin alone 0 10.0 With telaprevir 1.00 Without telaprevir 0.10 0.01 0 8 16 24 Time (hrs) 32 40 Suggest atorvastatin dose with concomitant BOC; monitor for symptoms of statin toxicity if using >40 mg/d atorvastatin Hulskotte EGJ et al. HEP DART 2011, Koloa, Hawaii, poster 122 48 0 10 20 30 Nominal time (hrs) 40 50 Combination is contraindicated Lee JE et al. Antimicrob Agents Chemother 2011, 55(10):4569-74 Effect of Steady-State Telaprevir on the Pharmacokinetics of Amlodipine 5 mg Concentration (ng/mL) 5.00 Calcium channel blockers (CCBs) With telaprevir Amlodipine, diltiazem, felodipine, nifedipine, nicardapine, verapamil are CYP3A4 substrates Concentrations may be by boceprevir or telaprevir Use with caution, clinical monitoring Consider dose reduction 0.50 Without telaprevir 0.05 0.01 0 50 100 150 200 250 Nominal time (hrs) Amlodipine AUC 179% Monitor for dose-related toxicity Lee JE et al. Antimicrob Agents Chemother 2011, 55(10):4569-74 Antihypertensive Medications Class Examples Potential DAA Interactions ACEI Enalapril, lisinopril, ramipril (renal) Not expected ARBs Losartan (2C9>>3A4 to active metabolite) Candesartan, irbesartan (2C9) Eprosartan, olmesartan, telmisartan, valsartan (biliary) Possible effect Low Not expected Betablockers Propranolol (2D6, 3A4, 2C19), carvedilol (2D6, 2C9> 1A2, 2E1, 3A4) Acebutolol, labetalol, metoprolol, pindolol (2D6) Atenolol, nadolol (renal) Possible Calcium channel blockers Amlodipine, diltiazem, felodipine, nifedipine, verapamil (3A4) Risk of CCB exposures; use with caution Diuretics Hydrochlorothiazide, furosemide, spironolactone (renal) Indapamide (2C9, 2D6, 3A4) Not expected Possible Low Not expected Treatment of Depression in HCV Place in Therapy Examples (route of metabolism) Potential DAA Interactions First Line Escitalopram, citalopram (2C19, 3A4>>2D6) 35% with TVR, no interaction with BOC Second Line Paroxetine, fluoxetine (2D6), bupropion (2B6) Sertraline (2B6>2C9/19, 3A4, 2D6), venlafaxine (2D6>3A4), desvenlafaxine (UGT>>3A4), mirtazapine (2D6, 1A3, 3A4) Low Possible Third Line Nortriptyline (2D6) Imipramine (2D6, 1A2, 2C19, 3A>UGT) Low Possible No Evidence Modafinil (3A4; induces 3A4) Amantadine (not metabolized) Possible ; DAA Not expected Avoid Duloxetine (1A2, 2D6) - CONTRAINDICATED Additive risk of hepatotoxicity Methadone Interactions Methadone is metabolized by CYP2B6, CYP2C19 & CYP3A, 85% protein bound; R-isomer is biologically active enantiomer Boceprevir interaction: In the presence of steady-state boceprevir, R-methadone AUC 16%, Cmax 10%; no clinical effects noted including opioid withdrawal Boceprevir exposures not affected by methadone Telaprevir interaction: In the presence of steady-state telaprevir, R-methadone Cmin 31%, Cmax 21% and AUC 21%, but median unbound Cmin of R-methadone was similar before and during telaprevir coadministration and no withdrawal symptoms were noted A priori methadone dose adjustments are not required when initiating DAA therapy, but close monitoring is recommended, with methadone dose adjustments if necessary Hulskotte et al. 2012, Van Heeswijk et al. 2011. Hormonal Contraceptives with DAAs Hormonal contraceptives may not be as effective in women taking boceprevir or telaprevir Boceprevir (Victrelis): 99% AUC drospirenone, 24% AUC EE Use 2 alternate effective methods of contraception during treatment with BOC and Peg IFNa/RBV Drospirenone (Yaz®, Yasmin®, Angelique®) is contraindicated Telaprevir (Incivek): 28% AUC, 33% Cmin of EE Use 2 additional non-hormonal methods of effective birth control during TVR dosing and for 2 months after the last intake of TVR. Benzodiazepine Interactions Majority are substrates of CYP3A4 Risk for prolonged/excessive sedation Oral midazolam & triazolam are contraindicated with boceprevir and telaprevir IV midazolam: consider dose, close monitoring for respiratory depression or prolonged sedation Other benzodiazepines: dose and monitor Consider using benzodiazepines that are glucuronidated: Lorazepam, oxazepam, temazepam Inhaled Corticosteroids Corticosteroids are CYP3A4 substrates Potential for corticosteroid concentrations resulting in significantly reduced serum cortisol concentrations Inhaled/nasal fluticasone, budesonide: Avoid co-administration with HCV PIs if possible, particularly for extended durations. May wish to use corticosteroid associated with less adrenal suppression (e.g., beclomethasone, ciclesonide) Use lowest possible dose, consider non-steroidal options Victrelis & Incivek. Product Monographs, 2011 PDE5 Inhibitors (sildenafil, tadalafil, vardenafil) PDE5 inhibitors are substrates of CYP3A4 Potential for DAAs to concentrations Dose-related side effects (headache, vasodilation, dyspepsia, visual disturbances) Contraindicated with DAAs if using for PAH For erectile dysfunction, use a lower dose with DAAs: Sildenafil: 25 mg q48h, tadalafil: 10 mg q72h Do not use vardenafil Interactions Between HCV & HIV Medications Challenges in treating HIV/HCV co-infected patients Additive toxicities: Anemia: ribavirin, zidovudine, DAAs CNS: interferon, efavirenz Potential for negative 2-way interactions concentrations of HIV agents concentrations of HCV DAAs Antiretroviral Treatment Options for Patients on Boceprevir or Telaprevir Protease Inhibitors (PIs) Boceprevir Telaprevir Avoid with ritonavir-boosted protease inhibitors Avoid ritonavir-boosted darunavir, fosamprenavir and lopinavir Atazanavir/ritonavir OK Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) Integrase Inhibitor Maraviroc Nucleoside Reverse Transcriptase Inhibitors Avoid efavirenz Dose with efavirenz Etravirine (?) Etravirine OK No data Rilpivirine OK Raltegravir OK No data potential / maraviroc; potential benefit on fibrosis? Tenofovir OK Avoid AZT (anemia) Managing Drug Interactions: 1) Medication Reconciliation Ensure medication records are up to date at each visit Prescription, OTC, vitamins/herbals, recreational drugs, inhalers, topical, prn agents Confirm doses, prn drugs Include all agents that have been started or stopped Patient education: Encourage patients to ask before taking any new prescription/non-prescription drug or supplement Communication with other HCP! Managing Drug Interactions: 2) Identify Potential Interactions Use a systematic approach to identify combinations of potential concern Apply knowledge of known PK characteristics Overlapping CYP pathways, substrate, inducer, inhibitor High index of suspicion with key classes of drugs Utilize current drug information resources: Product monographs, CPS, literature Conference abstracts, specialized HCV drug interaction websites Drugs Contraindicated with Boceprevir and Telaprevir (1) a1-adrenoreceptor antagonist Alfuzosin Antiarrhythmics Quinidine, propafenone, serious/life-threatening cardiac amiodarone. arrhythmia Flecainide (TVR) Antimycobacterials Rifampin Ergot derivatives Hypotension, cardiac arrhythmia Loss of virologic response Acute ergot toxicity Herbal product St. John’s wort Loss of virologic response Statins Lovastatin, simvastatin. Atorvastatin (TVR) Myopathy including rhabdomyolysis Neuroleptic Pimozide Serious/life-threatening cardiac arrhythmia Victrelis & Incivek. Product Monographs, 2011 Drugs Contraindicated with Boceprevir and Telaprevir (2) PDE-5 inhibitor Sildenafil. tadalafil (BOC); vardenafil (TVR) Visual abnormalities, hypotension, prolonged erection, syncope Sedatives/ hypnotics Oral midazolam, triazolam Increased sedation or respiratory depression Other Cisapride, astemizole, terfenadine Serious/life-threatening cardiac arrhythmia Anticonvulsants (BOC) Carbamazepine, phenytoin, phenobarbital Loss of virologic response OC (BOC) Drospirenone Hyperkalemia Aldosterone antagonist (TVR) Eplerenone Hyperkalemia Triptans (TVR) Eletriptan Coronary artery vasospasm, MI, vent. tachycardia, VF Victrelis & Incivek. Product Monographs, 2011 Managing Drug Interactions: Therapeutic Options Determine clinical significance Evaluate therapeutic options: Alter drug dose/dosing frequency Substitute with alternate agent Can any drugs be permanently or temporarily discontinued while on DAA treatment? Consider patient convenience and cost factors Patient counselling & close monitoring is critical Summary High potential for pharmacokinetic interactions between directly acting antivirals and other drug classes Consequences may include therapeutic failure and increased toxicity Often, interactions can be managed, but heightened level of awareness is needed Use a systematic approach to identify and manage individual drug regimens Importance of a specialized, inter-disciplinary team including pharmacy Additional Resources General Hansten PD. Science Med 1998;16-25. Kashuba ADM, Bertino JS Jr. Drug Interactions in Infectious Diseases, 2nd edition, c. 2005, pp:13-39. Metheny CJ et al. Pharmacotherapy 2001;21:778-96. Interactions in HCV and HIV: Kiser J et al. Hepatology 2012;55:1620-8. Tseng & Foisy. Curr Infect Dis Rep 2012;14:67-82. Internet Toronto General Hospital Immunodeficiency Clinic; www.hivclinic.ca Liverpool Pharmacology Group; www.hep-druginteractions.org www.hcvdruginfo.ca Side Effects of Antiviral Therapy for Hepatitis C Dr. Mark Levstik, FRCP(C) Associate Professor Medicine Division of Gastroenterology Multiorgan Transplant Unit London Health Sciences Centre Side Effects with Boceprevir and Telaprevir Hematological: (common to both PIs) Anemia, Neutropenia Effect is additive with INF and RBV Gastrointestinal Dysgeusia (BOC) Diarrhea (TVR & ? BOC) Anorectal irritation (TVR) Dermatological Telaprevir specific rash Side Effect Comparison of Phase III studies Adverse Effect Peg Interferon/ RBV Boceprevir/ P/R Anemia <100g/dl 30% 50% 17% 36% Rash 19% 17% 34% 56% Fatigue 59% 58% 50% 56% Diarrhoea 15% 20% 17% 26% Nausea 42% 46% 28% 39% Dysgeusia 16% 35% 3% 10% 7% 29% Anorectal Peg Interferon/ Telaprevir/ RBV P/R Dysgeusia and anemia increased with boceprevir; Rash, anorectal irritation and anemia increased with telaprevir. Incivek Product Monograph, June 2012 Victrelis Product Monograph, August 2012 Safety of Protease Inhibitors in Real Life: CUPIC Study Patients HCV genotype 1 infection Compensated cirrhosis (Child Pugh A) Treatment-experienced Relapsers Partial responders ( >2 log10 HCV RNA decline at Week 12 but never negative) Null responders theoretically excluded Treated in the French early access program (From February 2011) Hezode C et al. EASL 2012, Abstract 8 CUPIC: Treatment Regimen Interim analysis Peg-IFN + RBV BOC + Peg-IFN α-2b + RBV Follow-up BOC : 800 mg/8h; peg-IFNα-2b : 1,5 µg/kg/week; RBV : 800 -1400 mg/d TVR + Peg-IFN α-2a + RBV Peg-IFN α-2a + RBV Follow-up TVR : 750 mg/8h; peg-IFNα-2a : 180 µg/week; RBV : 1000- 1200 mg/d 0 4 8 12 16 36 Weeks 48 72 SVR assessment Hezode C et al. EASL 2012, Abstract 8 CUPIC: Patients Characteristics Baseline patient characteristics similar between BOC and TVR The CUPIC cohort had more advanced liver disease than in registration trials. In BOC arm 26% would not meet RESPOND-2 inclusion criteria In TVR arm 34% would not meet REALIZE inclusion criteria Previous treatment response (%) BOC TVR Partial responders 49 52 Relapsers 48 40 3 8 Null responders Hezode C et al. EASL 2012, Abstract 8 CUPIC: Preliminary Safety Findings (16-Week Interim Analysis) Patients, n (% patients with ≥ 1 event) Boceprevir n=159 Telaprevir n=296 Serious adverse events (%) 38.4 48.6 Premature discontinuation Due to SAEs (%) 23.9 7.4 26.0 14.5 Death (%) 1.3 2.0 Infection (Grade 3/4) (%) 2.5 8.8 0 0 6.8 0.7 Pruritus (Grade 3/4) (%) 0.6 3.7 Hepatic decompensation (%) 4.4 4.4 Rash Grade 3 (%) Grade 4 (SCAR) (%) Hezode C et al. EASL 2012, Abstract 8 CUPIC: Preliminary Safety Findings (16-Week Interim Analysis) Patients, n (% patients with ≥ 1 event) Anemia (%) Grade 2 (8.0 – <10.0 g/dL) Grade 3/4 (<8,0 g/dL) EPO use Blood transfusion Neutropenia (%) Grade 3 (500 – <1000/mm3) Grade 4 (<500/mm3) G-CSF use Thrombopenia (%) Grade 3 (25 000 – <50 000) Grade 4 (<25 000) Thrombopoïetin use Boceprevir (n=159) Telaprevir (n=296) 22.6 10.1 66.0 10.7 19.6 10.1 56.8 15.2 4.4 0.6 3.8 4.0 0.7 2.4 6.3 0.6 1.9 11.8 1.3 1.7 Hezode C et al. EASL 2012, Abstract 8 Take Home Message from CUPIC PI therapy in patients with cirrhosis is associated with more severe and more frequent AEs Anemia Increased EPO use, ribavirin dose reductions and transfusions Increased risk of severe infection Increased risk of hepatic decompensation Boceprevir Specific Side Effects Dysgeusia and decreased appetite more prevalent than control Hematological side effects more prevalent than control in Phase 2/3 naïve studies: Neutropenia (<0.75 x 109 /L): 31% vs. 18% in controls Platelets (< 50 x 109 /L): 3% vs. 1 % in controls Anemia: 50% vs. 30% in controls Grade II (<100 g/L): 49% vs. 29% Grade III (<85 g/L) : 6% vs. 3% Erythropoietin use 47% vs. 24% and pRBC 3% vs. 1% Victrelis Product Monograph, August 2012 Telaprevir Specific Side Effects Rash, anorectal disorders, diarrhea and anemia more common than control Rash seen > 50%, leads to 6% discontinuations Mild – 37% Moderate – 14% Severe – 5% Anorectal disorders seen with increase in diarrhea, itching and burning: 29% vs. 7% in controls Anemia: 32% vs. 15% in controls Grade II (<9.0-9.9 g/dL): 27% vs. 27% Grade III (7.0-8.9 g/dL) : 51% vs. 24% Incivek Product Monograph, June 2012 Anemia Management Mechanism of RBV-Associated Anemia RBV uptake into RBC adenosine kinase RBV-triphosphate Erythrocytes lack enzymes to hydrolyze RBV phosphates RBV-phosphates are “trapped” Erythrocyte T1/2 > 40 days RBV concentration in RBC 60-fold higher than serum (60:1) Marked depletion of RBC adenosine triphosphate (ATP) Impairs anti-oxidant defense mechanisms Induces RBC oxidative membrane damage Premature extravascular RBC removal by the reticuloendothelial system De Franceschi L. Hepatology 2000; 31:997-1004 Ribavirin Dose Reduction vs. EPO ? Retrospective analyses of Boceprevir phase III studies have suggested that reducing the dose of RBV did not alter the SVR rate. In patients treated with PEG+RBV (dual therapy), the effect of RBV dose reduction ON SVR was minimal if occurring when HCV-RNA was undetectable. Sulkowski MS et al. J Hepatol 2011; 54:S194-5. Reddy KR et al. Clin Gastroenterol Hepatol 2007; 5:124-9 Boceprevir Anemia Management: Erythropoietin vs. Ribavirin Dose Reduction Study Genotype 1 patients, naive of treatment, Hb < 150 g/L at baseline 687 patients treated with boceprevir RGT After completion of 4 week PEG-IFN/RBV lead-in, all patients initiated boceprevir Hemoglobin ≤100 g/L Randomisation Erythropoietin (40,000 IU/wk SC) n = 251 EPO: erythropoietin PEG-IFN: peginterferon RBV: ribavirin Ribavirin dose reduction (DR) n = 249 Hemoglobin ≤ 85 g/L: Secondary Strategy (EPO, RBV DR, transfusion) Poordad et al. EASL 2012, Abstract 1419 Results – Primary and Key Efficacy End Points End-of-treatment response, relapse, and SVR were comparable between RBV DR and EPO arms (95% CI) 100 82 82 RBV DR 71 75 Patients (%) -0.7% (-8.6, 7.2)* 71 EPO 50 25 203/249 205/251 178/249 178/251 10 10 19/196 19/197 0 EOT Response SVR Relapse DR, dose reduction; EOT, end of treatment; EPO, erythropoietin; RBV, ribavirin; SVR, sustained virologic response. *The stratum-adjusted difference (EPO vs. RBV DR) in SVR rates, adjusted for stratification factors and protocol cohort. Poordad et al. EASL 2012, Abstract 1419 Summary - Anemia Management Ribavirin dose reduction does not decrease SVR No advantage to Erythropoietin use, but may be used Consider pRBC transfusion to maintain safe Hb DAA should not be reduced DAA should not be restarted or continued without Peg/RBV Ribavirin may be increased once Hb recovers Protease Inhibitors: Management of Anemia Hb < 100 g/L any time during treatment Boceprevir Telaprevir RBV dose reduction Up to 3 x 200 mg increments* Reduce RBV to 600 mg/day Hb < 85 g/L Hb > 85 g/L EPO: 40-60,000 IU/wk AND/OR Transfusion Maintain RBV dose reduction * Note: First dose reduction of 400mg if patient receiving 1400mg/day RBV dose reduction to 600 mg can be used with Boceprevir as wel Rash Management - Telaprevir Rash Rash more prevalent in DAA but >50% with Telaprevir Rash can be categorized: Mild to moderate: < 30% of skin area Moderate: 30-50% of skin area Severe: generalized rash may progress with bullae, vesicles < 5% of patients Incivek Product Monograph, 2012 Rash Management Recommendations Mild: Watchful monitoring Oral antihistamines, moisturizers, topical steroids Moderate: < 50% body Monitor closely for progression/systemic symptoms Antihistamines, moisturizers, topical steroids Worsening/Severe: > 50% body ( < 4% of patients ) Stop telaprevir, observe closely for 7 days IF no better, stop Ribavirin, observe for 7 days. IF no better, stop Pegylated Interferon Incivek Product Monograph, 2012 Hézode C. Liver International. 2012; 32 Suppl 1:32-8 Cacoub P et al. Journal of Hepatology. 2012; 56(2):455-63 Telaprevir Severe Rash < 1% DRESS: Drug rash with eosinophilia and systemic symptoms Rash, fever, facial edema ± hepatitis/nephritis Eosinophils may not be present Stevenson-Johnson Syndrome Fever, target lesions and mucosal erosions/ulcers STOP ALL drugs Requires hospitalization May require systemic steroids Incivek Product Monograph, 2012 Hézode C. Liver International. 2012; 32 Suppl 1:32-8 Cacoub P et al. Journal of Hepatology. 2012; 56(2):455-63 Other Side Effects of Boceprevir and Telaprevir Gastroenterological Side Effects Nausea, vomiting, diarrhea Small meals three times daily with PI dosing useful Fiber, loperamide aid with loose stool Dysgeusia noted in Boceprevir patients Metallic taste, rarely leads to dose reduction or discontinuation Improved with chocolate administration Gastroenterological Side Effects: Telaprevir Nausea, vomiting and diarrhea common with TPV/PEG/RBV Anorectal irritation: Anorectal burning, itch and hemorrhoidal irritation common: > 29% Therapy: Frequent small meals, 21g fat per dose Fiber, loperamide and topical hydrocortisone therapy, help relieve symptoms Incivek Product Monograph, 2012 Hézode C. Liver International. 2012; 32 Suppl 1:32-8 Cacoub P et al. Journal of Hepatology. 2012; 56(2):455-63 Management of Depression Occurs in up to 37% of patients Conduct pre-therapy and routine assessments with CES-D or other depression scale Adjust interferon dose or discontinue therapy according to depression severity May warrant use of antidepressants Recommended agents to use with BOC and TVR: Escitalopram, citalopram (see Dr. Tseng’s chapter on DDIs) Direct-Acting Antiviral Therapy: Boceprevir and Telaprevir Patient side-effect education is important to success Pre-therapy recommendations include: Multivitamin, hydration, acetaminophen analgesia Dietary recommendations to decrease GI toxicity effects ( small meals, fiber, loperamide ) Skin care through moisturizers and antihistamines Close patient and hepatitis team communication Monitor and pre-empt severe side effects Drug and duration specific Case Study: Treatment Naive Edward Tam MD FRCPC Medical Director LAIR Centre Ms. MH 31 year old female Diagnosed in 2004 with genotype 1a HCV Previous IVDU Otherwise healthy Meds: Milk thistle No Biopsy ALT 1-2 x ULN on serial monitoring Ms. MH Followed periodically with monitoring of liver biochemistry FibroScan December 9, 2010: 4.9 kPa What evidence supports the use of Milk Thistle? Is FibroScan a reliable and accurate tool for fibrosis assessment? Does it represent a viable alternative to liver biopsy? FibroScan versus Liver Biopsy 1.00 Sensitivity 0.75 0.50 AUROC (95% CI) ≥ F2: 0.74 (0.68-0.80) ≥ F3: 0.89 (0.84-0.94) F4: 0.94 (0.90-0.97) 0.25 0.00 0.00 0.25 0.50 0.75 1.00 1-Specificity Myers RP et al. Can J Gastroenterol. 2010 Nov;24(11):661-70 Ms. MH FibroScan December 9, 2010: 4.9 kPa (consistent with stage 0 – 1 fibrosis) Discussions with patient throughout 2011 regarding therapy Although no medical urgency, very keen to pursue therapy for personal reasons Ms. MH January 6, 2012, treatment initiated with pegylated interferon alpha-2b (120mcg) plus ribavirin (500mg BID), as planned lead-in to boceprevir-based treatment. Week 0 HCV RNA 5.29 logs ALT 106 Hb 144 Plts 295 Neutrophils 6.0 Ms. MH: Week 4 Results Week 0 Wk 2 Wk 4 5.29 logs -- Undetectable ALT 106 53 33 Hb 144 120 108 Plts 295 236 214 Neutrophils 6.0 2.0 2.0 HCV RNA Given the undetectable HCV RNA at the end of WK4 lead-in (dual therapy), is adding Boceprevir necessary? Significance of Lead-in Response SPRINT-2: SVR based on degree of early interferon response (log decline in HCV RNA at week 4 of P/R in all patients (cohort 1 + cohort 2) PR48 BOC RGT 100 % of patients with SVR 89 90 90 89 89 89 97 80 79 80 BOC/PR48 70 72 74 65 60 58 60 45 40 33 43 28 28 30 21 20 0 0 5 Log10 viral load decrease after weeks of P/R lead-in Vierling et al. EASL 2011. Results Through Week 12 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Undetectable -- Undetectable -- Undetectable ALT 33 27 26 22 28 Hb 108 107 101 91 94 Plts 214 179 177 175 174 Neutrophils 2.0 1.3 1.6 1.2 1.2 HCV RNA Boceprevir added with 5th interferon injection HCV RNA remains undetectable Due to worsening anemia and fatigue, RBV dose reduced to 600mg total daily dose after wk 10 results Results Through Week 24 Wk 12 Wk 16 Wk 20 Wk 24 Undetectable -- -- Undetectable ALT 28 32 25 24 Hb 94 105 101 103 Plts 174 171 164 169 Neutrophils 1.2 1.4 1.0 1.0 HCV RNA HCV RNA remained undetectable through week 24, and patient qualifies for shortened duration therapy (to D/C at week 28) Case Study: Cirrhosis Nir Hilzenrat, MD Gastrointestinal Division, Department of Medicine, SMBD- Jewish General Hospital, Associate Professor of Medicine, McGill University, Montreal, Quebec Case History 58 year old woman, acquired hepatitis C from blood transfusion 30 years prior Symptoms – mild fatigue and depression ALT 2xULN Synthetic function normal Viral load 3x105 IU/mL Liver biopsy (2002) F 3/4, activity 2/4 Case History Previous treatment in 2000 with pegylated interferon and ribavirin < 1 log drop at week 12 Treatment discontinued Treatment-related side effects Severe fatigue Fall in Hb level (148 g/L to 108 g/L). Comments Previous treatment failures classified into Null responder Viral load does not fall by 2 logs at week 12 Partial responder Viral load falls by > 2 logs, but never negative Relapser Viral load negative on therapy but positive after therapy Telaprevir (REALIZE study ) response in null responders was 29% (21/72) Boceprevir (PROVIDE study) response in null responders was 40% (19/47) Zeuzem, S. et al. N Engl J Med 2011; 364: 2417-28 Bronowicki, JP., International Liver Congress 2012, Abstract 204, EASL 2012 Comments Probability of response with F3 or F4 and prior treatment failure (48 weeks of therapy) Telaprevir Boceprevir % n % n Relapser 87 48/55 83 15/18 Partial responder 34 11/32 46 6/13 Null responder 14 7/50 - - Vertex Pharmaceutical (Canada) Incorporated. Product Monograph: Incivek (Telaprevir tablets). http://pi.vrtx.com/files/canadapm_telaprevir_en.pdf (Accessed February 1, 2012) Bruno,S., Boceprevir in Addition to Standard of Care Enhanced SVR in Hepatitis C Virus Genotype-1 With Advanced Fibrosis/Cirrhosis: Subgroup Analysis of SPRINT-2 and RESPOND-2 Studies, Oral Presentation, EASL 2011 Case Continued Patient made aware of low probability of cure (15-40%) However, she was willing to start treatment It was accepted that we will assess the continuity of the treatment based on the response rate, i.e., HCV-RNA level, and the severity of adverse effect during the treatment Fibroscan prior suggested cirrhosis ALT x 4 ULN Liver synthetic function normal Viral load 2.8x106 IU/ml Case Continued Treatment was started with Peg INF/RIBA and boceprevir At week 4 viral load decline was 0.8 logs Question How important is the magnitude of the decline in viral load following the lead-in phase (TW4) of the PR & BOC treatment? Importance of 4-Week HCV RNA in Boceprevir Triple Therapy In RESPOND-2 likelihood of SVR for relapsers and partial-responders was associated with response to interferon in the lead-in phase SVR in all patients SVR in F3/F4 < 1 log drop at wk 4 33% 14-25% > 1 log drop at wk 4 73% 55-87% Bruno,S., Boceprevir in Addition to Standard of Care Enhanced SVR in Hepatitis C Virus Genotype-1 With Advanced Fibrosis/Cirrhosis: Subgroup Analysis of SPRINT-2 and RESPOND-2 Studies, Oral Presentation, EASL 2011 Bacon BR et al. N Engl J Med 2011;364:1207-17 Comments In the PROVIDE study, the SVR for null responders was 40% Week 4 HCV RNA < 1 log decline from baseline SVR 36% Week 4 HCV RNA >1 log decline from baseline SVR 55% Bronowicki, JP., Sustained Virologic Response (SVR) in Prior PegInterferon/Ribavirin (PR) Treatment Failures After Retreatment with Boceprevir (BOC) + PR: PROVIDE Study Interim Results, International Liver Congress 2012, Abstract 204, EASL 2012 Case Continued The result was discussed with the patient. She was made aware that the likelihood of achieving SVR is poor. However, the patient asked to reassess the probability of her success rate after 4W of PR & BOC treatment, i.e., 8W of the whole treatment. Question The HCV RNA at week 8 was undetectable What is the likelihood of achieving SVR? Question How long should she be treated for? At week 12 and 24 the HCV RNA remained undetectable Usual side effects, anemia, fatigue and depression Question What are the recommended approaches for this patient (i.e. cirrhotic null responder to previous PR treatment) according to the American Association of the Study of Liver Diseases (AASLD) and Canadian Association of the Study of Liver Diseases (CASL) updated guidelines? Investigational Anti-HCV Drugs Beyond Boceprevir and Telaprevir Stephen D. Shafran MD, FRCPC, FACP Professor, Division of Infectious Diseases Department of Medicine University of Alberta Investigational Drugs for HCV with Activity in Humans Direct-acting antivirals (DAAs) Non-DAAs Peginterferon lambda (IFN-) Tarabivirin Pro drug of ribavirin Higher ratio of liver to RBC distribution than RBV Less anemia than with RBV Silibinin (milk thistle extract, IV formulation) Cyclophilin inhibitors (eg. Alisporivir*) * Development on hold due to cases of pancreatitis Pegylated Interferon Lambda IFN- (a type III interferon) receptors are expressed in hepatocytes but in fewer other cells than IFN-a (a type I interferon). In a phase-IIa trial in treatment-naïve patients, pegIFN- 120-180 μg weekly + RBV resulted in similar or higher virologic responses at weeks 4 and 12 vs. pegIFNa-2a + RBV with less toxicity.1 1. Muir A et al. AASLD 2010. Abstract 821 EMERGE: PegIFN-λ/RBV vs. PegIFNa-2a/RBV Wk 24: GT 2 or 3 Wk 48: GT 1 or 4 PegIFNa-2a 180 μg/wk + RBV (n=133) Treatment naïve patients with genotype 1-4 HCV infection (n=526) PegIFN- 120 μg/wk + RBV (n=128) PegIFN- 180 μg/wk + RBV (n=131) PegIFN- 240 μg/wk + RBV (n=134) Zeuzem S et al. EASL 2011. Abstract 1360 EMERGE: PegIFN-/RBV vs. PegIFNa-2a/RBV: Preliminary Results to Week 12 PegIFNa-2a Parameter (%) PegIFN- 180 μg 120 μg 180 μg 240 μg GT1/4 RVR 5.8 6.0 14.7* 16.5* GT1/4 cEVR 38 55* 56* 56* GT 2/3 RVR 31 43 76* 67* GT 2/3 cEVR 86 90 97 83 Myalgia 30 11 6.1 9.0 Fever 29 7 7 6 Hb < 10 g/dL 44 21 15 13 ANC < 750 15 0 0.8 0 PLT < 25 1.5 0 0 0 Conjugated bilirubin 2.3 5.5 8.5 19.7 * p<0.05 compared with PegIFNa-2a Zeuzem S et al. EASL 2011. Abstract 1360 EMERGE: PegIFN-/RBV vs. PegIFNa-2a/RBV: Efficacy and Safety in Genotypes 2 & 3 SVR rates comparable in pegIFN arm vs. pegIFNa-2a 100 SVR24 (%) Lambda 180 µg (N = 29) Alfa 180 µg (N = 30) 6.9 44.8 RBV dose reduction (Hb associated) 0 23.3 Neutrophils < 750/mm3 0 27.6 Platelets < 100,000/mm3 0 24.1 PegIFN dose reduction (hematologic reason) 0 23.3 6.9 13.3 75.9 65.5 60.0 53.3 40 20 0 Fewer hematologic AEs and ALT/AST elevations with pegIFN- Adverse Event, % 80 60 N = 30 29 29 30 Alfa Lambda Lambda Lambda 180 µg 120 µg 180 µg 240 µg Hb < 10 g/dL or ∆ > 3.4 g/dL ALT/AST > 5 to 10 x ULN PegIFN- 180 μg dosage chosen for phase III trials Zeuzem S et al. EASL 2012. Abstract 10 Proteins encoded by the HCV genome: Three validated targets and four classes of DAAs 5’ UTR region 3’ UTR region 9.6 kb RNA Polyprotein C E1 E2 p7 NS2 NS3 4A Polyprotein NS4B NS5A Polyprotein processing 1 C Core E1 E2 Envelope Glycoproteins NS5B p7 NS2 Protease 2 NS3 NS4A Serine Helicase Serine Protease Protease Cofactor NS4B NS5A RNA binding NS5A inhibitors NS3-4A protease inhibitors 2 3 NS5B RNA-dependent RNA polymerase NS5B polymerase inhibitors 1 Nucleoside analogs Non-nucleoside analogs 3 4 Adapted from Asselah T et al. Liver International 2011; 31 Suppl 1:68-77 HCV NS3/NS4A Protease Inhibitors (1) Inhibit cleavage of viral polyprotein chain, essential to HCV replication. Very active against genotype (GT) 1. A single nucleotide mutation in the NS3 region (R155K) results in resistance in GT 1a, but two mutations are required for resistance in GT 1b. Some have activity against non-1 genotypes, but very little clinical data exist. “First generation” NS3 PIs (boceprevir and telaprevir) are linear ketoamides and are associated with anemia; “Second generation” NS3 PIs are macrocyclic and are not associated with anemia. HCV NS3/NS4A Protease Inhibitors (2) The two most developed after BOC/TVR are simeprevir (TMC-435)1 and faldaprevir (BI-201335)2. Both are in fully enrolled phase 3 clinical trials vs. dual PegIFN + RBV controls; results are expected in early 2013. Simeprevir and faldaprevir are dosed once daily (150 and 120 mg, respectively) and do not produce additive anemia beyond PegIFN + RBV. Simeprevir is associated with some increase in bilirubin due to reversible inhibition of OATP1B1 and MRP2 transporters. Faldaprevir inhibits glucuronyl transferase and can cause a Gilbert’s like syndrome (similar to the HIV protease inhibitor, atazanavir). Faldaprevir is also associated with rash and photosensitivity. 1. Fried MW et al. AASLD 2010. Abstract LB-5 2. Sulkowski M et al. EASL 2011. Abstracts 60 and 66 HCV NS3/NS4A Protease Inhibitors (3) Two NS3 PIs (danoprevir1 and ABT-4502) are being developed for administration with low dose ritonavir. Ritonavir, an HIV protease inhibitor, is a potent inhibitor of CYP3A4; ritonavir increases exposure of drugs metabolized principally via CYP3A4. Other NS3 PIs are under development, including asunaprevir (BMS-650032), MK-5172, GS-9451, sovaprevir (ACH-1625), whereas the development of several others has been terminated. 1. Rouzier R et al. EASL 2011. Abstract 62 2. Lawitz E et al. EASL 2011. Abstract 1220 HCV NS5A Inhibitors NS5A is a protein with no known enzymatic function, but a definite, yet poorly defined role in viral replication. NS5A inhibitors are very potent and pangenotypic in the replicon system1. They are significantly more active vs. genotype 1b than genotype 1a. Daclatasvir, the most developed NS5A inhibitor, is given once daily, and is in phase 3 in treatment naïve patients with genotypes 1 and 4, and in phase 2 for genotypes 2 and 3, and for genotype 1 in the HIV co-infected. NS5A inhibitors in phase 2 are ABT-267 and GS-5885 NS5A inhibitors have no “signature” toxicity to date2. 1. Gao M et al. Nature 2010; 465:96-100 2. Pol S et al. Lancet Infect Dis 2012; 12(9):671-7 Antiviral Activity of Daclatasvir in Combination with PegIFNa2a + RBV in Treatment of Naïve Patients with Chronic HCV Genotype 1 Infection Day 1 Week 48 Placebo + PegIFNa-2a 180 µg/wk + RBV 1000/1200 mg/d Treatment naïve HCV GT1 patients n=48 Week 72 SVR 24 Daclatasvir 3 mg QD + PegIFNa-2a 180 µg/wk + RBV 1000/1200 mg/d Daclatasvir 10 mg QD + PegIFNa-2a 180 µg/wk + RBV 1000/1200 mg/d Daclatasvir 60 mg QD + PegIFNa-2a 180 µg/wk + RBV 1000/1200 mg/d Pol S et al. Lancet Infect Dis 2012; 12(9):671-7 Daclatasvir (DCV) with PegIFNa-2a + RBV: Virologic Response at Weeks 4, 12 & SVR (ITT) PR Percent HCV RNA negative (<10 IU/mL by Roche TaqMan) 100 PR + DCV 3 mg PR + DCV 10 mg PR + DCV 60 mg 92 83 83 83 83 83 80 58 60 42 40 42 42 25 20 8 0 RVR cEVR SVR (24) 12 patients per treatment arm; the 60 mg QD dose was selected for phase 3 Pol S et al. Lancet Infect Dis 2012; 12(9):671-7 HCV NS5B Polymerase Inhibitors NS5B is a RNA-dependent RNA polymerase, responsible for viral RNA synthesis The viral polymerase is the “classic” target for antiviral drugs (eg. DNA-dependent DNA polymerase in HSV and VZV or RNA-dependent DNA polymerase [reverse transcriptase] in HIV and HBV) As with HIV RT inhibitors, there are two subtypes of NS5B inhibitors, Nucleoside/nucleotide analogues Act as RNA chain terminators High barrier to resistance Pan-genotypic Non-nucleoside inhibitors Least potent class of DAA Low barrier to resistance HCV NS5B Polymerase Inhibitors: Drugs with Antiviral Activity in Humans Nucleoside/nucleotide analogues Mericitabine (RG-7128) Sofosbuvir (GS-7977/ PSI-7977) VX-135 (ALS-2200) Non-nucleoside inhibitors Tegobuvir (GS-9190) Setrobuvir (ANA-598) ABT-333 (lead Abbott NNI) ABT-072 (back-up Abbott NNI) VX-222 BI-207127 IFN-Free, All Oral Regimens with SVR Data As of October 2012, 5 pharmaceutical companies have presented pilot data demonstrating that SVR can be achieved in small numbers of patients. The majority of IFN-free regimens to date continue to include ribavirin. Only one study to date has included patients with cirrhosis (SOUND C-2). The most common combination of agents in IFN-free regimens for genotype 1 has been a 3-drug combination of a NS3 PI, a NS5B non-nucleoside (NN) inhibitor and ribavirin. For GT 2 & 3, IFN-free regimens demonstrating SVR are sofosbuvir with either RBV or daclatasvir. IFN Free SVR: The Very First Report (Daclatasvir + Asunaprevir in GT1 Prior Null Responders) Daclatasvir+asunaprevir Follow-up HCV RNA (log10 IU/mL) 7 6 5 4 3 2 LLOQ LLOD 1 0 1 2 3 4 6 8 10 12 16 20 24 Week SVR was achieved in 2/9 GT 1a and 2/2 GT 1b prior null responders to PR with 24 weeks of DCV + ASV (all enrolled patients were non-cirrhotic) On therapy breakthrough was common in GT 1a Lok AS et al. EASL 2011; NEJM 2012;366:216-24 Dual Oral Therapy with Daclatasvir and Asunaprevir x 24 Weeks for HCV GT1b Study conducted in Japan All had genotype 1b Treated with asunaprevir (NS3 PI) and daclatasvir (NS5A inhibitor) x 24 weeks Virologic Response (%) Prior Null Responders (n=21) [6 IL-28B CC] IFN Ineligible/Intolerant (n=22) [16 IL-28B CC] Week 4 RVR 52 86 Week 12 cEVR 91 91 EOTR 91 86 SVR24 91 64 Suzuki F, et al. EASL 2012. Abstract 14 PILOT: NS3 PI + NN + RBV: Virologic Responses HCV RNA Negative (%) n = 11, HCV GT1, treatment-naïve, non-cirrhotic; 8 GT1a, 3 GT 1b Only IL-28B CC patients were enrolled, so that they would have a high probability of salvage with PegIFN + RBV in the event that all-oral therapy failed All were treated with ABT-450/r 150/100 mg QD + ABT-072 400 mg QD + RBV 1000/1200 mg/d 100 100 100 91 91 82 80 60 40 20 n/N 11/11 11/11 10/11 10/11 9/11 Wk 4 (RVR) Wk 12 (EOT) SVR12 SVR24 SVR36 0 Lawitz E, et al. EASL 2012. Abstract 13 CO-PILOT: NS3 PI + NN + RBV: Virologic Responses HCV RNA negative (%) Because of the favorable results in PILOT, CO-PILOT was open to all IL-28B genotypes and explored prior PR non-responders; All had genotype 1 and were non-cirrhotic In CO-PILOT, a different NS5B non-nucleoside inhibitor was used (ABT-333) than in PILOT (ABT-072) 100 90 90 95 95 93 79 80 RVR eRVR SVR4 SVR12 93 79 77 59 60 47 47 40 20 0 ABT-450/r 250/100 mg QD + ABT-333 + RBV Treatment naive (n = 19; 17 G1a, 2 G1b) * 11 partial responders, 6 null responders ABT-450/r 150/100 mg QD + ABT-333 + RBV Treatment naive (n = 14; 11 G1a, 3 G1b) ABT-450/r 150/100 mg QD + ABT-333 + RBV Prior PR Non-responders* (n = 17; 16 G1a; 1 G1b) Poordad F et al. EASL 2012. Abstract 1399 INFORM-SVR: NS3 PI + Nucleoside + RBV in GT1: SVR12 by HCV Subtype and IL28B Genotype Data shown are patients treated with 24 weeks of mericitabine + danoprevir/r + ribavirin; all were treatment naïve and non-cirrhotic SVR12 rates were encouraging in GT1b but disappointing in GT1a 100 80 SVR12 (%) All (n = 64) GT1a (n = 43) GT1b (n = 21) 100 71 60 76 80 60 50 44 41 40 40 27 26 20 n/N = 0 32 25 20 26/64 11/43 15/21 Overall n/N = 0 6/19 4/15 CC 2/4 20/45 7/28 13/17 IL28B Genotype Non-CC Gane E et al. EASL 2012. Abstract 1412 SOUND-C2: NS3 PI + NN ± RBV: SVR12 by Study Arm N=362; the largest IFN-free study to date All had GT1 and were treatment naïve; 10% had cirrhosis All received faldaprevir 120 mg QD + RBV 1000/1200 mg/d Patients were randomized to 5 arms, 4 containing BI-207127, 600 mg TID (3 arms) or 600 mg BID (one arm) for 3 different durations RBV-free arm was stopped prematurely due to high relapse rate SVR12 (%) 100 80 60 59 61 68 56 39 40 20 n/N 0 BI 207127 Dosing 48/81 49/80 43/77 53/78 18/46 TID 16 wks + RBV TID 28 wks + RBV TID 40 wks + RBV BID 28 wks + RBV TID 28 wks (no RBV) Zeuzem S et al. EASL 2012. Abstract 101 SOUND-C2 BID Dosing Arm: Higher SVR12 in Patients With GT1b or GT1a-IL28B CC SVR According to IL28B and HCV Subtype: BID 28 Wks + RBV (ITT) 100 82 75 80 SVR12 (%) 84 60 40 32 20 n/N = 0 7/22 6/8 31/37 9/11 1a non-CC 1a CC 1b non-CC 1b CC HCV Subtype and IL28B Genotype Boehringer Ingelheim has decided to undertake additional studies of this 3-drug regimen only in patients with GT1b and those with GT1a who are IL-28B CC Zeuzem S et al. EASL 2012. Abstract 101 Sofosbuvir (GS-7977) Nucleotide NS5B inhibitor Once daily oral dosing with no food effect No described toxicity to date Pangenotypic No virological breakthroughs reported to date Studied in combination with RBV or daclatasvir or simeprevir* In GT2 & 3, sofosbuvir + RBV x 12 weeks achieved SVR24 in 10/10 patients; sofosbuvir + RBV x 8 weeks achieved SVR12 in 10/10 patients (all non cirrhotic) Two phase 3 RCTs are fully enrolled in GT2 & 3 (including cirrhotics); results expected EASL 2013 FISSION: Treatment naïve patients randomized to sofosbuvir + RBV x 12 weeks vs. PegIFN + RBV x 24 weeks FUSION: Treatment failure patients randomized to 12 wk vs. 16 wk of sofosbuvir + RBV * No data have been presented on sofosbuvir + simeprevir Gane E et al. EASL 2012. Abstract 1113 Sofosbuvir + RBV x 12 Weeks: Results in GT1 Treatment Naïve Patients In ELECTRON, 25/25 achieved EOT; 22/25 (88%) achieved SVR4 and 3/25 (12%) relapsed1 In QUANTUM, 17/17 achieved EOT; 10/17 (59%) achieved SVR4, and 7/10 (41%) relapsed2 Combined ELECTRON and QUANTUM SVR in GT1 naives is 32/42 (76%) Only non-cirrhotic patients were enrolled in ELECTRON and QUANTUM Future studies in GT1 will examine Longer treatment durations of Sofosbuvir + RBV The addition of a third antiviral drug 1. Gane E et al. EASL 2012. Abstract 1113 2. Gilead Press Release, Apr 19, 2012 The Canadian Liver Foundation gratefully acknowledges the participating health care professionals for their contributions to this project and for their commitment to the liver health of Canadians. The Canadian Liver Foundation (CLF) was the first organization in the world devoted to providing support for research and education into the causes, diagnoses, prevention and treatment of all liver disease. Through its chapters across the country, the CLF strives to promote liver health, improve public awareness and understanding of liver disease, raise funds for research and provide support to individuals affected by liver disease. For more information visit www.liver.ca or call 1-800-563-5483. This project made possible through the financial support of Merck Canada Inc. The views, information and opinions contained herein are those of the authors and do not necessarily reflect the views and opinions of Merck Canada Inc.