* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Gastrointestinal Physiology
Survey
Document related concepts
Transcript
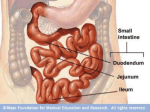
Gastrointestinal Physiology Most images courtesy Joe Haeberle, UVM Splanchnic Circulation • Vasoconstrictors- Ang II, endothelin, NE (a2-agonists), PGF2a, Vasopressin • Vasodilators- Ach, Adenosine, Bradykinin, CGRP, histamine, NO, VIP, b2-agonists Vasorelaxation cGMP GPCR dilator Gs cAMP Decreased free Ca++ AC Vascular Smooth Muscle Cell Splanchnic Circulation (cont’d) • Myogenic Control- resistance vessels can close themselves off in times of high MAP – a mechanism for autoregulation • Postprandial Hyperemia- increases in blood flow to organs in response to a meal – mediated through intrinsic VIP release • Villar countercurrent mechanisms- make villi susceptible to ischemic necrosis – oxygen is shunted between arteriole and venule Intrinsic Nervous System (gut brain) • Nerves that interconnect within GI organs and plexuses, independent of the autonomic system. – Auerbach’s, Meissner’s plexus contribute! • Receptor neurons are sensory (detect stretch, damage), effector neurons are motor (cause SM contraction) • Excitatory NT’s- Ach, Subst. P • Inhibitory NT’s- VIP, NO – what causes contraction/relaxation of smooth muscle? Gastrointestinal Smooth Muscle • Single-unit (gap junctions, coordinated contraction) • Activated/inhibited by many neurotransmitters, hormones • Contraction can be tonic or phasic depending on location/purpose of muscle cells – GI Wall vs. Sphincter Smooth Muscle Excitation/Contraction Coupling • Slow Waves cause “Spike Potentials” during Ach stimulation • Spike Potentials lead to increased [Ca++] • [Ca], hormones – – activate MLCK phosphorylates MLC Slow Waves and SM Contraction Questions: 1. Where are the slow waves the most frequent Orad in the GI system? 2. Which cells initiate slow Interstitial Cells of wave activity? • Slow Waves are regular changes in SM VM. • They do not cause SM contraction unless they reach a threshold and cause action potentials. • They are propagated along the GI tract. • Parasympathetic Stimulation and other inputs increase the probability that VM will reach threshold. Cajal Slow Waves vs. MMC’s • In fasting individuals, slow waves persist, but contractions diminish, until an MMC. • MMC (migrating motor complex) is a set of strong contractions that lasts a few minutes in one section of the digestive tract, then moves aborally. • These complexes last 90 minutes and will restart in the stomach approximately every 90 minutes as long as you’re fasting. • Their roles – to flush remaining food and bacteria into the large intestine. – to tell you that you’re hungry! GI Smooth Muscle (cont’d) • Less-obvious differences between Skeletal/Cardiac and Smooth muscle: – 1. Primary site of activation is thick filament (myosin light chain) instead of thin (TnC) – 2. Smooth muscle undergoes pharmacomechanical coupling (hormones can contract SM without changing VM.) • e.g. agents that induce MLC phosphorylation directly • Similarities: – 1. Both have actin/myosin and use cross-bridging to contract • SM has 15:1 ratio of thin:thick filaments – 2. Both are activated by intracellular [Ca++] • Smooth Muscle Activators and Inhibitors: – Activators: Ach, Histamine – Inhibitors: NO, VIP Saliva! • Salivary Amylase (ptyalin) • Lingual Lipase • Mucins (glyco-proteins) • Fluid – Hypotonic – High [K+] • With increased salivary flow, [HCO3-]and osmolarity increase • Secretion is inhibited by sleep Saliva Secretion Control Esophageal Peristalsis • 1o Peristalsis: – Initiated by swallowing (not after vagotomy) • 2o Peristalsis: – Caused by residual food in esophagus • Vagal nuclei run the show (ambiguus, DMN) • SM Peristalsis persists after vagotomy (enteric NS takes over) Diseases of the Esophagus • Achalasia: – Stenosis of LES, dilation of body of esophagus • “bird-beak” appearance on barium study • Hiatal Hernia – LES protrudes into thoracic cavity • LES tends to be patent due to negative pressure in thoracic cavity • LES Tone: – Increased by Ach, Gastrin – Decreased by Sympathetics, PGE1 Acid Regulation in the Stomach More Acid Regulation Gastric Emptying • Contraction in the stomach – Orad <<<< Caudad (3/minute) – Primarily peristaltic • Solid food is usually forced back into stomach for mixing • Duodenum contracts much more often but is phasic (pseudosphincter) Regulation of Gastric Emptying • Chyme entering the duodenum activates intestinal receptors. • This leads to increased contraction of the duodenum and decreased contraction of the stomach (Delayed Gastric Emptying) • Secretin, CCK, and GIP (enterogastrone) are released by the duodenum and feed back on the stomach to slow down. Stomach Pathophysiology • Dumping Syndrome – Uncontrolled gastric emptying due to lack of feedback inhibition by duodenum • post-surgical • neurological deficit – Un-digested food makes it to the colon – Patient barely makes it to the bathroom • Pyloric Stenosis – Projectile vomiting – Pediatric disease • failure to thrive • projectile vomiting after breast feeding (wall’s sign) • caused by atresia, improper formation of duodenum Gastric and Duodenal UlcersH. pylori • Gastric-stomach. Duodenal-obvious. • Peptic- hydrochloric acid/pepsin present • 80% of gastric, 90% of duodenal ulcers are due to H. pylori infection – weakens mucus barrier – causes acid production (decreased Bicarb) • NSAIDs can also contribute (COX-1) • Gastrin Carcinomas- secrete gastrin – cause excessive acid secretion • Treatment? – triple therapy (2 antibiotics, one antacid or bismuth) – vagotomy Pancreatic and Bile Secretions • Acid in Duodenum activates Secretion of Secretin to initiate HCO3- secretion • AA, Lipids stimulate Gastrin (quick response) and CCK (prolonged response) to initiate pancreatic enzyme secretion. • CCK also causes GB contraction, Sphincter of Oddi relaxation, and increased Bile Salt excretion by the liver. Components of Bile • 50% Bile Acids (Cholic, chenodeoxycholic, deoxycholic, and lithocholic acid – Product of Cholesterol + 7aHydroxylase, most is recycled from distal ileum – Form micelles- amphipathic – pK= approx. 7 if unconjugated – conjugated to taurine or glycine- pK goes down, allows them to be soluble in the intestine • Phospholipids (lecithin) – solubilized by bile salts • Cholesterol • Bile pigments – bilirubin glucuronide Bilirubin Metabolism senescent RBC heme BilirubinAlbumin Adduct Macrophages (spleen) Bilirubin (indirect) Urine Systemic Circulation (urobilin) Feces (stercobilin) Bilirubin Glucuronide Portal Circ. Urobilinogen Bile Duct Intestinal Flora Hepatocyte Enterohepatic Circulation • • • • • Most ile acids are taken up by distal ileum epithelial cells by 2o active transport when they are no longer needed for digestion. They travel to the liver via the portal vein and are taken up by hepatocytes through the NTCP channel for recycling. They re-enter the bile canaliculus through the BSEP (bile salt exchange pump) Other pumps exist for bilirubin glucuronide (MDR2), cations (MDR1) and phospholipids (MDR3). Bile acid-dependent bile secretion involves osmotic gradients created by the transport of bile acids. Liver Pathophysiology- Cholestasis • Cholestasis is the absence of bile flow – 2 Main Causes: • Failure to secrete bile acids and salts (no osmotic gradient) • Obstruction of the biliary tree (cholelithiasis, cholangitis, tumor) – Cholestasis leads to jaundice (yellow skin/sclera) due to bilirubin backup in plasma • Indirect Bilirubin- unconjugated • Direct Bilirubin- conjugated Intestinal Reflexes • Vagovagal - Vagal sensory nerves relay stretch information to the brainstem, releasing vagal efferents to (e.g.) parietal and G cells in the stomach. • Intestinointestinal- distention of one portion of the intestine leads to decreased contractions caudad of the bolus. • Gastroileal, gastrocolic - Stomach activity leads to ileocecal relaxation and increased mass movements in the colon – These reflexes are mediated through both long and short nervous pathways (extrinsic and intrinsic) and hormones (CCK, gastrin) Absorption of Sugars • Polysaccharides are broken down in the mouth, stomach, and small intestine • Disaccharidases (e.g. sucrase) further digest them into monosaccharides, which are taken up by special transporters: 2’ AT fac. diffusion fac. diffusion Absorption of Water/ Lytes • Most water is absorbed in the small intestine (approx. 7-9 L/ 24 hours!), another 600 mL/day is absorbed in the colon. • Small intestine- water follows nutrients • Large intestine- water follows electrolytes! – Na+ enters via its concentration gradient, pumped out the basolateral side by ATPase – Cl- is exchanged for HCO3-, which is excreted. Absorption of Proteins/ Lipids SCFA’s • Good bacteria in the colon produce Short Chain Fatty Acids from carbohydrates. • These acids have been shown to kill harmful bacteria and nourish colon epithelial cells. • The End