* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The pathophysiology of Alzheimer`s disease
Survey
Document related concepts
Transcript
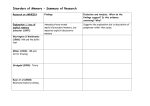
REVIEW THE PATHOPHYSIOLOGY OF ALZHEIMER’S DISEASE AND DIRECTIONS IN TREATMENT — Ann S. Morrison, PhD, RN, CS,* and Constantine Lyketsos, MD, MHS† ABSTRACT The pathophysiology of Alzheimer’s disease (AD) is complex, involving several neurotransmitter systems and pathophysiologic processes. The 3 hallmarks of AD—β-amyloid plaques, neurofibrillary tangles, and neuronal cell death—are well known and central factors in AD pathology. These hallmarks, combined with our information on neurotransmitter involvement, are specific to AD based on the timing, sequence, and location of these changes. This article reviews the pathophysiology and course of brain damage seen during AD progression, from preclinical to severe stages. Understanding these processes is fundamental in understanding AD progression and symptom manifestation, and in assessing the potential risks and benefits of therapeutic interventions. There are now 5 approved drugs for the cognitive symptoms of AD—4 acetylcholinesterase inhibitors (approved for mild to moderate AD) and 1 noncompetitive glutamate receptor antagonist (approved for moderate to severe AD). Recent studies with these drugs are focusing on longerterm follow-up (1 year and beyond), in addition to more “clinically relevant” outcomes, such as measures of function and nursing home *Clinical Nurse Specialist Coordinator, Department of Psychiatry, Alzheimer’s Disease Research Center, The Johns Hopkins Hospital, Baltimore, Maryland. †Professor of Psychiatry and Behavioral Sciences, Codirector, Division of Geriatric Psychiatry and Neuropsychiatry, The Johns Hopkins Hospital, Baltimore, Maryland. Address correspondence to: Ann S. Morrison, PhD, RN, CS, Clinical Nurse Specialist Coordinator, Department of Psychiatry, Alzheimer’s Disease Research Center, The Johns Hopkins Hospital, 550 Broadway Avenue, Baltimore, MD 21205. E-mail: [email protected]. 256 placement. Other treatments (vitamins E and/or C, nonsteroidal anti-inflammatory drugs, and statins [cholesterol-lowering drugs]) show some promise in preventing or delaying AD progression, although more data are needed. There are now several published guidelines for the treatment of AD. Although some may argue that the effect of these drugs is modest, any preservation of function and delay of nursing home placement has important and permanent consequences for the patient and caregiver. The profound and sometimes rapid loss of memory and function with AD underscores the importance of trying at least 1 of these treatments in a patient with AD. (Adv Stud Nurs. 2005;3(8):256-270) ALZHEIMER’S DISEASE PATHOPHYSIOLOGY CHANGES IN BRAIN STRUCTURE Alzheimer’s disease (AD) pathology can be characterized on a macro level as the progressive loss of brain tissue. As the disease progresses, neurons die in a particular pattern over time. One of the earliest signs of AD is memory loss, particularly short-term recall. The brain areas involved in memory include the cortex, especially the hippocampus (Figure 1).1 Preclinical AD begins in the entorhinal cortex, which connects the hippocampus, the structure responsible for memory formation (short- and long-term memory; Figure 2), to the cerebral cortex.1 Several studies, such as ones including magnetic resonance imaging, suggest that neuronal loss (measured by atrophy in select regions) may start years before signs of memory loss emerge.2,3 Vol. 3, No. 8 n October 2005 REVIEW Figure 2. Brain Changes in Preclinical Alzheimer’s Disease Figure 1. Major Areas of the Brain Corpus Callosum Cerebral Cortex Thalamus Cerebral Cortex Hypothalamus Hippocampus Cerebellum Brain Stem Hippocampus Side view of the brain Entorhinal Cortex Reprinted with permission from Alzheimer’s Disease Education and Referral Center Web site. Available at: http://www.alzheimers.org/unraveling/04.htm. Accessed June 17, 2005.1 Copyright ©2002, Christy Krames. As the brain atrophies, cerebrospinal fluid fills in the space previously occupied by brain tissue. In mild to moderate AD, patients experience more prominent memory loss (eg, difficulty recalling wellknown names and confusion about familiar places), a decline in the ability to process complex thoughts (eg, difficulty with balancing the checkbook or preparing a meal), and mood and personality changes. In the brain, atrophy extends to other areas of the cerebral cortex (Figure 3).1 At the later stages of AD progression, the cortex has atrophied in areas that control speech, reasoning, sensory processing, and conscious thought (Figure 4).1,4 As expected with this degree of brain atrophy, the symptoms of severe AD increase in severity (ie, impaired longterm memory, seizures, incontinence, weight loss, no recognition of loved ones, inability to sit up, and groaning/moaning/grunting). The progression of atrophy throughout the brain is diagrammed in Figure 5.1 DEGENERATIVE PROCESSES IN ALZHEIMER’S DISEASE On a micro level, AD is characterized by 3 neuropathologic hallmarks: extracellular plaques of β-amyloid protein (amyloid plaques), intracellular neurofibrillary tangles (NFTs), and neuronal degeneration. Plaques and NFTs were first discovered by Alois Alzheimer in a 1906 autopsy of a demented patient. Although they are a defining component of AD, they are not unique to AD. Plaques and NFTs occur with normal aging and in some other neurodegenerative disorders. In AD, plaques and NFTs are localized to areas in the brain that correspond to clinical symptoms. Advanced Studies in Nursing n Figure 3. Brain Changes in Mild to Moderate Alzheimer’s Disease Cortical Shrinkage Moderately Enlarged Ventricles Shrinkage of Hippocampus Reprinted with permission from Alzheimer’s Disease Education and Referral Center Web site. Available at: http://www.alzheimers.org/unraveling/04.htm. Accessed June 17, 2005.1 Figure 4. Brain Changes in Severe Alzheimer’s Disease Extreme Shrinkage of Cerebral Cortex Severely Enlarged Ventricles Extreme Shrinkage of Hippocampus Reprinted with permission from Alzheimer’s Disease Education and Referral Center Web site. Available at: http://www.alzheimers.org/unraveling/04.htm. Accessed June 17, 2005.1 257 REVIEW Figure 5. Brain Damage and Atrophy During Alzheimer’s Disease Progression A B C A, preclinical Alzheimer’s disease; B, mild to moderate Alzheimer’s disease; and C, severe Alzheimer’s disease. Reprinted with permission from Alzheimer’s Disease Education and Referral Center Web site. Available at: http://www.alzheimers.org/unraveling/04.htm. Accessed June 17, 2005.1 β-amyloid plaques are thought to play the central role in AD pathogenesis (the “amyloid hypothesis”), with several diverse pathophysiologic processes that follow (Figure 6), described as an “amyloid cascade.”5 The AD pathophysiologic cascade is complicated, but each discovery of a neurotransmitter or pathologic process leads to the potential discovery of new therapeutic targets. The β-amyloid hypothesis β-amyloid plaques are clumps of insoluble peptides that result from the abnormal cleavage of amyloid precursor protein (APP), the exact function of which is unknown. APP is normally cleaved by 3 enzymes—βsecretase, γ-secretase, and α-secretase. Cleavage by βsecretase, followed by γ-secretase, yields a soluble 40 amino acid peptide (Figure 7).1 In AD, a variant form of the γ-secretase cleaves APP at an incorrect place, creating a 42 amino acid peptide called Aβ42 or Aβ, which is not soluble and aggregates into identifiable clumps termed β-amyloid plaques (Figure 8).1 α-secretase actually serves a protective function as it cleaves APP at a site that prevents Aβ formation. Genetic studies of AD support the role of γ-amyloid plaques and β-secretase in AD pathogenesis. Three genes have been identified in familial AD (APP, PS1 [presenilin 1], and PS2) and all are known to be involved with the formation of Aβ. (The use of italics indicates a gene, whereas normal font indicates the protein made from the gene.) APP is the gene that codes for APP (the protein) and is located on chromosome 21. Interestingly, people with Down’s syndrome (trisomy 21—3 copies of chromosome 21) ultimately 258 develop AD at a younger age than the general population.6 PS1 and PS2 are genes that code for presenilin, the catalytic subunit of γ-secretase. There are at least 20 known mutations of APP, more than 140 known mutations in PS1, and approximately 10 in PS2.6,7 Immunization against Aβ is under investigation as a treatment in animals and humans.8-11 Neurofibrillary tangles are seen as dying or dead neurons when viewed after histologic staining. NFTs result from the destruction of neuronal microtubules caused by the modification of their supporting protein, tau (Figure 9).1 Microtubules are essential components of neuronal cell structure; they act as tracks along which nutrients are delivered and neuronal transmission is propagated in the neuronal axon. During AD pathogenesis, tau proteins become hyperphosphorylated, disrupting their bonds to microtubules, thus collapsing microtubule structure and Figure 6. Diagram of the Amyloid Cascade Cytoplasm γ-secretase γ-secretase Cell membrane α-secretase p3 Extracellular space Aβ β-secretase APP β-APP α-APP Aβ generation Oxidation Excitotoxicity Aβ aggregation Inflammation Tau hyperphosphorylation Neuron Senile plaque with microglial activation Cell death Neurofibrillary tangles Cognitive and behavioral abnormalities Neurotransmitter deficit APP = amyloid precursor protein. Reprinted with permission from Cummings. N Engl J Med. 2004;351:56-67.5 Vol. 3, No. 8 n October 2005 REVIEW destroying the neuron’s transport and communication system. Neuronal cell death ensues. Although the causal relationship is unclear, hyperphosphorylation of tau is thought to occur after plaque formation.12,13 The cholinergic hypothesis Loss of cholinergic neurons is another well-established pathology of AD. By late-stage AD, the number of cholinergic neurons is dramatically reduced; in some parts of the brain there is more than 75% loss.14 Acetylcholine is an important neurotransmitter in brain regions involving memory, and loss of cholinergic activity correlates with some aspects of cognitive impairment. Cholinergic abnormalities are the most prominent neurotransmitter changes in AD. Acetylcholine binds to 2 postsynaptic receptor types: muscarinic and nicotinic. Presynaptic nicotinic receptors influence the release of neurotransmitters important for memory and mood—acetylcholine, glutamate, serotonin, and norepinephrine—all of which have been implicated in AD pathology. The glutamatergic/excitotoxicity hypothesis Glutamate is the primary excitatory neurotransmitter in the brain. In the central nervous system, it is virtually ubiquitous and is estimated to be involved in roughly 66% of all brain synapses.15,16 Glutamatergic neurons are also critical because they form projections to other areas of the brain, including cholinergic neurons, thus influencing cognition. In AD, the pathology associated with glutamatergic neurons is not with glutamate itself but with the levels of pre- and postsynaptic glutamate receptors. Of the 3 types of postsynaptic glutamate receptors, AD pathology has only been linked to 1 type, the N-methyl-D-aspartate (NMDA) receptor, which appears to undergo sustained low-level activation in AD brains, causing sustained low-level neurotransmission. This dysregulation at the glutamate NMDA receptor is thought to perpetuate a vicious cycle of neuronal damage, in which continuous activation of the receptor leads to chronic calcium influx within the neuron that interferes with normal signal transduction.17 It also leads to increased production of APP, which, as noted earlier in this article, is associated with higher rates of plaque development and hyperphosphorylation of tau protein (thus NFT formation) followed by neuronal toxicity.18-21 Glutamate is cleared from the synapse by reuptake into the nerve terminal and surrounding glial cells. Advanced Studies in Nursing n Figure 7. The Structure of Amyloid Precursor Protein Relative to the Cell Membrane β-amyloid Enzymes Amyloid precursor protein is a transmembrane protein. Cleavage by β-secretase, followed by γ-secretase, yields a soluble 40 amino acid peptide. This peptide is shown here in green. Copyright ©2002, Christy Krames. Figure 8. Insoluble Aggregates of Aβ42 β-amyloid Plaque Copyright ©2002, Christy Krames. Figure 9. The Role of Tau Protein in Neuronal Cell Death Stabilizing Tau Molecules Healthy Neuron Microtubules Disintegrating Microtubule Microtubule Subunits Fall Apart Tangled Clumps of Tau Proteins Diseased Neuron Disintegrating Microtubules Copyright ©2002, Christy Krames. 259 REVIEW Dementia patients also appear to have reduced numbers of glutamate reuptake sites or abnormal expression of a glutamate transporter, which may be linked to NFT formation.22,23 nases COX-1 and COX-2, in the AD brain.28 It is interesting to note that the inflammation in AD is chronic and localized to discrete areas of the brain, as are the other types of cellular damage with AD.29 The oxidative stress hypothesis In AD brains, Aβ induces lipid peroxidation and generates reactive oxygen and nitrogen species; these are oxygen or nitrogen molecules containing an unpaired extra electron (termed species) that reacts with other molecules to achieve a stable configuration. During this process, the reactive species forms a molecular bond with another molecule, while a high-energy electron (termed a “free radical”) is thrown off. The reaction is permanent, thus structurally and functionally altering the molecule to which the reactive species is attached. The free radical is left to cause cellular and molecular damage. This oxidative damage can occur in virtually all types of neuronal macromolecules (eg, lipids, carbohydrates, proteins, and nucleic acids). The brain is especially vulnerable to damage from oxidative stress because of its high oxygen consumption rate, abundant lipid content, and relative paucity of antioxidant enzymes compared to other organs. In neurons, oxidation can result in numerous problems, including upregulation of proinflammatory cytokines and irreparable DNA damage.24,25 Oxidative stress is thought to be important early in AD progression because it is temporally linked to the development of plaques and NFTs.26 Other neurotransmitter deficiencies During the AD process, brain regions in which acetylcholine, serotonin, and norepinephrine are prominent become altered, affecting widespread areas of the cerebral cortex. Serotonin is known to be important in affective illness (eg, depression and anxiety), and depression is a common comorbidity with AD. The number of serotonin receptors and transporters are altered in AD brains, corresponding to decline in measures of cognition and presence of anxiety.30-32 Also, norepinephrine levels are reduced and norepinephrine neurons are lost in AD.33 Norepinephrine may play an important role in some of the behavioral and psychological symptoms of dementia (aggression, agitation, and psychosis), in addition to memory loss.34 The chronic inflammation hypothesis β-amyloid deposits, NFTs, and damaged neurons may stimulate inflammation as a natural response to cell damage. Microglia (1 of 4 types of brain cells, including neurons, astrocytes, and oligodendrocytes) are involved in immune and inflammatory responses to injury or infection within the brain. During AD pathogenesis, microglia are activated to release potentially cytotoxic molecules, such as proinflammatory cytokines, reactive oxygen species, proteinases, and complement proteins.27 This is a normal response to cellular damage that, in AD, appears to proceed uninhibited, causing more harm than protection. Cytokines stimulate inflammatory processes that may promote apoptosis (programmed cell death) of neurons and oligodendrocytes and induce myelin damage. Inflammation as part of AD pathology has been observed as increased prostaglandins, which are produced by the cyclooxyge- 260 Cholesterol Cholesterol is also now thought to be involved in AD pathogenesis. The brain contains the highest amount of cholesterol of any human organ.35 Elevated cholesterol levels appear to increase Aβ production, whereas reduced cholesterol synthesis (eg, as a result of statin drugs) reduces Aβ levels, thus the risk of AD progression.36 Cholesterol reduction may also reduce the risk or severity of dementia through protection from vascular risk factors; vascular dementia often coexists in patients with AD. In the Honolulu-Asia Aging Study, cholesterol levels of 218 Japanese-American men were measured at mid-life and late-life. At autopsy, there was a strong linear association between mid-life and late-life high-density lipoprotein cholesterol and the number of plaques and NFTs in the cortex.37 SUMMARY Our understanding of AD pathology is now extending beyond the details of pathophysiologic processes to a broader view of the sequence and timing of these events in the development of symptoms and illness progression. Aβ generation is considered to be the first step of an “amyloid cascade,” which continues with oxidation, excitotoxicity, inflammation, and the hyperphosphorylation of tau. Each of Vol. 3, No. 8 n October 2005 REVIEW these processes contributes to neurotransmitter abnormalities and neuronal cell death, which then manifest as cognitive and behavioral abnormalities.5 KEY POINTS • In AD, brain atrophy and neuronal loss occur in a predictable pattern beginning with the entorhinal cortex and hippocampus, ultimately progressing throughout the brain. • AD is characterized by 3 neuropathologic hallmarks: plaques of β-amyloid protein (amyloid plaques), NFTs, and neuronal degeneration, all of which occur during normal aging, but in AD occur in specific locations in the brain. • β-amyloid plaques are thought to play the central role in AD pathogenesis, described as the “amyloid cascade.” • The β-amyloid hypothesis maintains that formation of β-amyloid plaques is the first step in AD pathology, and genetic and histopathologic studies support this hypothesis. NFTs occur after plaque formation. • The cholinergic hypothesis is supported by the drastic and widespread loss of cholinergic neurons in AD, the benefits with acetylcholinesterase inhibitors, and the role of the nicotinic cholinergic receptor. • The glutamate/excitotoxicity hypothesis maintains that slow but steady activation of a glutamate receptor leads to cellular damage. • The oxidative stress hypothesis suggests that βamyloid induces oxidative stress causing permanent damage to some neuronal macromolecules (especially lipids) and creating reactive species, which further propagate neuronal toxicity. • The chronic inflammation observed with AD is thought to be the result of all of these mechanisms causing cell damage and death. In AD, inflammatory cytokines respond to these processes and contribute to neuronal destruction because they appear to act uninhibited. • Serotonin and norepinephrine are also involved in AD pathology. Serotonin is an important factor in depression and anxiety, both of which are common in patients with AD. • Cholesterol also appears to have a role in AD progression, perhaps through a reduction in vascular risk factors, which are common in patients with AD. Advanced Studies in Nursing n TREATMENTS FOR ALZHEIMER’S DISEASE OVERVIEW Pharmacologic treatments for the primary symptoms of AD, namely memory loss and cognitive impairment, have only become available within the past decade. Four of 5 approved therapies (tacrine, donepezil, rivastigmine, and galantamine) act by inhibiting the enzyme acetylcholinesterase, which is responsible for breaking down acetylcholine postsynaptically, thus keeping acetylcholine in the synapse longer. As described earlier in this article, cholinergic neuron loss is the primary type of neurodegeneration in AD. The fifth drug, memantine, acts as a noncompetitive antagonist to the NMDA receptor, curtailing the low-level but steady NMDA receptor activation thought to occur in AD and contributing to excitotoxicity.17 Several other treatments that address not only the symptoms but also the pathophysiologic processes in AD are also under investigation. CHOLINESTERASE INHIBITORS Although there are 4 approved cholinesterase inhibitors, only 3 are commonly used in the United States. The fourth, tacrine, is still available but rarely prescribed because of the potential hepatotoxicity associated with its use; it also has a complicated titration schedule. Tacrine should probably never be recommended as first-line therapy for AD. Although it is still on the market, there is no practical use for tacrine in the treatment of AD. However, nurses may still encounter prescriptions for it. A summary of the recommended dosing and titration schedule, in addition to common adverse events with each drug, are listed in Table 1.38-41 Donepezil, rivastigmine, and galantamine are indicated for mild to moderate AD; memantine is indicated for moderate to severe AD. Donepezil was the first drug to be approved by the US Food and Drug Administration (FDA) for the symptoms of mild to moderate AD. Its efficacy was established in 2 randomized, double-blind, placebocontrolled studies.42,43 Donepezil was followed by rivastigmine, the clinical efficacy of which was shown in 3 randomized, placebo-controlled studies in the United States and internationally.44-46 The efficacy of galantamine was demonstrated in 4 randomized, double-blind, placebo-controlled studies—2 in the United States and 2 in other countries.47-50 The initial safety and efficacy studies were typically shorter than 6 261 REVIEW Table 1. The Currently Available Treatments for AD Symptoms—A Summary* Drug Common Adverse Events† AD Indication Dosing Donepezil Mild to moderate 5 mg or 10 mg; treatment with a 10-mg dose should not be considered until patients have been on a daily dose of 5 mg for 4 to 6 weeks to avoid adverse events Nausea, diarrhea, insomnia, vomiting, muscle cramps, fatigue, and anorexia Rivastigmine Mild to moderate 3–6 mg twice daily; starting dose: 1.5 mg twice daily; increase to 3 mg twice daily after 2 weeks; other dose increases should be separated by at least 2 weeks Nausea, vomiting, loss of appetite, dyspepsia, asthenia, and weight loss Galantamine Mild to moderate 8–12 mg twice daily, preferably with morning and Nausea and vomiting evening meals; 24 mg/d may provide additional benefit for some patients, but it is associated with more adverse events; starting dose: 4 mg twice daily; increase to initial maintenance dose after at least 4 weeks Memantine Moderate to severe Target dose: 20 mg/day; starting dose: 5 mg/day; Confusion, dizziness, headache, and constipation titration: increase in 5-mg increments to 10 mg/d (5 mg twice daily), 15 mg/d (5 mg and 10 mg as separate doses), 20 mg/d (10 mg twice daily); minimum recommended interval between dose increases is 1 week; can be taken with or without food *Tacrine continues to remain on the market, but it is rarely used because of its potential hepatotoxicity and other adverse events. †Based on clinical studies. AD = Alzheimer’s disease. Data from Donepezil US prescribing information38; Galantamine US prescribing information39; Memantine US prescribing information40; Rivastigmine US prescribing information.41 months. Current studies of AD drugs are focusing on longer follow-up, other AD-related indications (eg, mild cognitive impairment [MCI] and more severe stages of AD), nursing home placement, vascular risk factors, and the pathophysiology of AD. Long-term follow-up There has been 1 long-term study of donepezil that extended to 4.9 years, an extension of an original 14week study.42 The results showed evidence of clinical benefit (ie, maintenance of baseline scores for cognition measures) during the first 6 to 9 months of openlabel treatment, with gradual cognitive decline after 9 months. The treatment group was compared to historical controls, which was a serious methodological problem for this study. The rate of cognitive decline throughout the nearly 5-year study was slower for those patients receiving donepezil than the estimates for patients who had not been treated.51 The benefits with rivastigmine have been shown in studies of 1- and 2-years’ duration. In the 1-year studies, differences in cognitive decline as measured by the AD assessment scale-cognitive subscale were -4.45 ± 0.8 (placebo) ver- 262 sus 0.82 ± 0.71 (rivastigmine) and -8.0 (historical placebo) versus -3.8 (rivastigmine).52,53 In the 2-year study, cognitive decline slowed by 35% in those patients receiving rivastigmine compared to a historical placebo group.54 Improvement with rivastigmine was also observed in a subgroup of moderately severe patients.55 The long-term efficacy of galantamine was shown in 3 studies. In an 18.5-month study, patients taking galantamine enjoyed sustained cognitive benefits during the entire study duration.56 In two 3-year studies, galantamine was associated with a roughly 50% slower cognitive decline compared to predicted rates of decline in a clinically similar historical control sample of patients with AD.57,58 Disease severity Donepezil has shown significant benefit on measures of cognition compared to placebo in patients with “early stage” (mild) AD.59 An important observation in this study population is that the placebo group showed virtually no signs of cognitive decline (as measured by the Mini-Mental State Examination [MMSE]) during the study period, whereas in studies of patients with mild to moderate AD, patients receiv- Vol. 3, No. 8 n October 2005 REVIEW ing placebo showed cognitive decline in MMSE scores during the study.59 Therefore, the extent of observed donepezil benefit may depend on the level of AD severity. At the other end of the severity spectrum, donepezil was compared to placebo in patients with moderate to severe AD and showed significant benefit in cognition measures at all time points during the 6month study.60 Two studies have analyzed the effect of rivastigmine based on disease severity, but from a different approach. In a 1-year study, patients were classified as slowly progressive or rapidly progressive, based on the magnitude of response seen in the first 6 months of the study. The final results showed notable and significant differences in response to rivastigmine between these 2 groups of patients, with patients who were rapidly progressive obtaining greater benefit from rivastigmine treatment.61 In a 12-month study of patients with mild AD or MCI, cognitive function was slightly improved or maintained in the patients with mild AD and unchanged or slightly worsened in the patients with MCI (both groups receiving rivastigmine); cognitive function was markedly worsened in untreated patients with AD.62 Functional measures Researchers are now turning to more “clinically relevant” outcomes, such as functional decline (ie, ability to perform activities of daily living [ADLs] or instrumental ADLs [IADLs]), nursing home placement, and effect on caregiver burden. ADLs focus on basic functioning, such as toileting, feeding, dressing, bathing, walking, and grooming. IADLs are more complex activities, which most adults of normal mental capacity can perform, such as operating household appliances, paying bills and managing money, shopping, preparing meals, and participation in hobbies. The effect on ADLs is important for several reasons. ADLs instill and maintain a sense of independence and selfefficiency, which is critical for patients’ and caregivers’ quality of life. In AD, loss of ADLs is enduring and is a significant predictor of institutionalization.63 Therefore, preservation of ADLs is a critical outcome with important and permanent ramifications. A 1-year study of donepezil versus placebo suggested that donepezil use may have effects on delaying loss of ADLs. Patients taking donepezil were 31% less likely to experience functional decline (ie, losing the ability to perform an ADL or IADL) than those taking placebo.64 The authors noted that patients on Advanced Studies in Nursing n donepezil tended to stabilize over time, rather than to improve over baseline, “suggesting that clinicians should aim for stability rather than actual improvement in ADLs.”64 This is an important message to convey to patients and their caregivers as AD progresses and they consider treatment with a cholinesterase inhibitor. Another study showed not only slower decline in ADLs and IADLs with donepezil treatment but also less decline in the components required for completing each ADL (initiation, planning and organization, and effective performance).65 Caregiver burden was also measured as time required with the patient for ADLs/IADLs and stress levels. Caregivers reported spending a mean of 52.4 fewer minutes/day on ADLs and 17.2 fewer minutes/day on IADLs with donepezil-treated patients. Almost all components of the caregiver stress scale favored donepezil. The authors also noted the importance of stabilizing cognitive function because the placebo group did not show a floor effect (ie, patients never reached a point at which further decline was not measurable).65 Rivastigmine has beneficial effects on ADLs, as shown in a retrospective analysis of 3 studies.66 Also, ADL impairment differed across the stages of AD. Table 2 lists the ADLs with a significant change from baseline based on 3 levels of severity.66 A secondary analysis of a 5-month study showed that galantamine treatment resulted in little or no decline from baseline in ADL measures compared to significant decline in the placebo group.48,67 Galantamine treatment resulted in maintenance or improvement in ADL and IADL measures, with significant improvement over placebo in 3 of 6 basic ADLs (toileting, bathing, and grooming) and 6 of 17 IADLs (conversation, managing personal belongings, current events, writing, hobbies, and operating household appliances).67 ADL stabilization was seen throughout the range of AD severity, but the greatest differences were observed in those patients with severe disease.67 Regarding caregiver time, galantamine also has notable effects. Pooled data from two 6-month studies show that caregivers reported spending a mean of 32 fewer minutes per day with galantamine-treated patients than with placebo-treated patients, a savings of approximately 3.5 hours per week. In patients with moderate AD, the benefits were even greater—a mean daily time savings of 53 minutes or more than 6 hours per week. Similarly, galantamine-treated patients could spend 27 more minutes per day unsupervised and, in the 263 REVIEW moderate AD group, the benefit was extended to spending 68 more minutes per day unsupervised.68 The profound consequences of maintaining ADLs is illustrated in a case study from Tariot and Jakimovich, in which donepezil was administered to a patient with severe AD, behavioral problems, and several comorbidities following admission to a long-term care facility.69 The positive effects of donepezil treat- Table 2. ADLs Affected Based on Degree of AD Severity with Rivastigmine or Placebo Treatment GDS ≤3 GDS = 4 PDS Item Mean change Improvement, % Mean change Improvement, % Cannot handle money -0.1 vs -4.1* 49 vs 33* Has a clear concept of time 0.1 vs -3.7 53 vs 40 Discusses politics -0.1 vs -3.3 51 vs 38 Dresses properly -0.5 vs -4.1 50 vs 39 Drives car safely -1.9 vs -5.4 44 vs 33 Forgets things 0.9 vs -3.3* Rearranges objects Stops participation in family finances Cannot tell time 0.5 vs -2.2 52 vs 40 Dials telephone numbers 2.1 vs -2.1 56 vs 44 Increased time doing hobbies/pursuits 2.4 vs -1.0 62 vs 43 Takes normal precautions 1.0 vs -1.7 56 vs 40 Unable to drive alone 1.3 vs -3.5 55 vs 42 GDS ≥5 Mean change Improvement, % -1.6 vs -6.9 45 vs 32 52 vs 32* -1.5 vs -5.3* 40 vs 28* 0.7 vs -2.3 51 vs 38 -1.1 vs -5.8* 45 vs 30* -1.4 vs -4.7 45 vs 32 Cannot use telephone -3.1 vs -7.6* 42 vs 30* Confusion in different settings -2.3 vs -6.5* 42 vs 28* Good eating manners -2.5 vs -6.7* 42 vs 28* Makes mistakes doing hobbies/pursuits -1.1 vs -6.8* 44 vs 27* Does hobbies/pursuits Stops household chores Walks/travels alone Tells time Uses tools properly Cannot discuss family finances Walks safely Cannot accurately care for finances Stops social attendance Drives own car Works at his/her job Meaningfully discusses TV, movies, and similar events with spouse, family, or caregiver This table shows the ADLs as listed in the PDS that were significantly changed from baseline during the study in the observed cases dataset. AD severity was measured by the GDS and divided into 3 groups. As the GDS score increases, the severity of AD increases. *Indicates P <.05 for rivastigmine versus placebo in the intent-to-treat dataset. AD = Alzheimer’s disease; ADL = activity of daily living; GDS = Global Deterioration Scale; PDS = Progressive Deterioration Scale. Reprinted with permission from Potkin et al. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26:713-720.66 264 Vol. 3, No. 8 n October 2005 REVIEW ment included engagement in meaningful conversations about family events and current events seen on television, although he was amnesic for details; coherent periods of (factually correct) reminiscence on his life; and improved ability to perform ADLs, including independent toileting, reduced belligerent and sexually inappropriate behavior, discontinuation of haloperidol, ability to travel to a family event, and restoration of walking ability; none of which were possible when he was admitted to the nursing facility.69 Nursing home placement Nursing home placement is another important milestone in AD progression. The desire and decision to place patients with AD in full-time nursing care varies with each patient (based on severity of disease and neuropsychiatric symptoms) and the caregiver’s circumstances, including financial resources and caregiver ability. In general, families probably prefer to keep the patient at home as long as possible. Conversely, some caregivers would prefer to place a patient under fulltime professional care, but cannot afford to do so. If the patient is a widow/er and the adult children live far away, the preference may be for earlier placement because geographic constraints prohibit at-home care. Studies of cholinesterase inhibitors’ effect on nursing home placement have yielded mixed results, possibly because of these varying influential factors. One study of donepezil versus placebo estimated (conservatively) that proper use of donepezil over 9 to 12 months (ie, therapeutic doses and high compliance rates) resulted in a delay of nursing home placement of 21.4 months for a first-time dementia-related placement and 17.5 months for permanent placement.70 The authors note that “doctors and caregivers need to be educated that, in the same way as the actual benefits of treating hypertension or hyperlipidemia are seen only after years of treatment, treatment of AD with donepezil needs to be maintained to see important long-term benefits.”70 A study in the United Kingdom of donepezil showed no difference in institutionalization after 3 years of follow-up, but the decision to place patients in nursing homes or even to treat with a cholinesterase inhibitor was based on different factors from those in the US healthcare system.71 In clinical practice, a typical drug trial for a cholinesterase inhibitor would be approximately 4 months (for titration up to the therapeutic and best-tolerated dose) to see some stabilization in memory, function, and/or Advanced Studies in Nursing n behavior. If no change is observed, a different drug in this class can be tried. Head-to-head comparisons Direct comparisons of cholinesterase inhibitors are rare in the published literature. A comparison of galantamine to donepezil revealed no significant differences between the 2 treatment groups at study end (52 weeks) in measures of ADLs and neuropsychiatric symptoms.72 However, cognition measures showed a greater benefit with galantamine treatment, maintaining baseline levels with galantamine but worsening with donepezil.72 Cholinesterase inhibitors and anticholinergic drugs Anticholinergic drugs are part of many therapeutic drug classes and are commonly prescribed. They are notorious for producing undesirable cognitive effects, to which patients with AD are especially sensitive. Their concurrent use is likely to negate any of the cognitive benefit with cholinesterase inhibition. A crosssectional study of Iowa Medicaid beneficiaries aged 50 years and older indicated that a surprising 35.4% of these patients received concurrent anticholinergic agents with cholinesterase inhibitors. Roughly 33% of patients received an anticholinergic agent within 90 days (before or after) of starting the cholinesterase inhibitor.73 Nurses should evaluate their patients’ drug profiles at each visit, especially when a cholinesterase inhibitor is prescribed, to avoid this unfortunate situation. Negating the effects of cholinesterase inhibitors incurs significant burden and cost to the patient and the healthcare industry. NMDA ANTAGONISTS Memantine is the only NMDA antagonist approved for the treatment of AD. Its efficacy was demonstrated in 2 randomized, double-blind, placebo-controlled studies in the United States.74,75 In addition to those studies, memantine was compared to placebo in patients already receiving stable doses of donepezil and showed an added benefit when coadministered with this cholinesterase inhibitor, with regard to measures of cognition, ADLs, global outcome, and behavior.75 An oral solution of memantine was recently approved by the FDA, which offers an alternative that may make administration easier for patients who have trouble swallowing tablets or prefer taking medication in liquid form. 265 REVIEW In all of the studies of AD drugs, it is important to remember that the results are a summation of effect on the entire study group. Individual patients respond to a drug to varying degrees, with some patients improving markedly and others showing mild or even no improvement. The only way to know whether a particular patient will respond to any of these drugs is to try. A drug trial is worth the cost because the loss in ADLs and memory and effects on behavior as a result of AD are devastating. VITAMINS E AND C Vitamin E is found in all cell membranes and helps to maintain cell membrane structure. Vitamin E also acts as an antioxidant by neutralizing the effects of oxygen free radicals. Vitamin E is able to donate a hydrogen atom, thus stabilizing the reactive species with the unpaired electron. Vitamin C may be involved in “recycling” the vitamin E from its oxidized form for further use and is also a known antioxidant.76 The recommended daily allowance of vitamin E is 22 IU for adults, which can typically be obtained through the diet.76 As recently reviewed, the few studies evaluating vitamin E and/or C for prevention of AD (through diet or nutritional supplements) do not provide any clear direction, although there is a lot of interest in their use. Some studies show a benefit with 1 or both vitamins, whereas other studies show no effect.76,77 In a recent study in patients with MCI, the effects of 2000 IU vitamin E, 10 mg donepezil, and placebo were compared over 3 years of treatment. There was no significant difference in the rate of progression to AD among the 3 groups, although donepezil showed some benefit during the first 12 months and in apolipoprotein E (APOE)-«4 allele carriers.78 It is difficult to identify the most appropriate role of vitamin E for AD. Variations in study design and source of the vitamins (diet, daily supplement, and multivitamin) make an overall interpretation of vitamin E/C efficacy difficult.76,77 Another confounding factor is whether the role of vitamins E and/or C should be used as treatment with AD diagnosis or as a preventive measure. The recent meta-analysis regarding high-dose vitamin E supplementation and risk of all-cause mortality and the strong response from the medical community underscore the ambiguous role of vitamin E for chronic diseases. The study raised several issues regarding vitamin E that need to be investigated.79,80 Nonetheless, leading medical organizations (as discussed later in this article) endorse consideration 266 of vitamin E for treatment of AD at a recommended dose of 2000 IU, except in patients with vitamin K deficiency (in whom this large dose may exacerbate coagulation defects). ANTI-INFLAMMATORY AGENTS Over the past 5 to 10 years, several studies have suggested that anti-inflammatory drugs (nonsteroidal antiinflammatory drugs [NSAIDs]) are associated with a decreased incidence of AD. A 2003 meta-analysis of the existing literature (using 9 studies) showed that the relative risk of AD among users of NSAIDs was 28% lower than among nonusers of NSAIDs.81 Among short-term users (ie, <1 month), the risk was 5% lower, increasing to 17% reduced risk among intermediate users (<24 months) and further still to 73% lower risk among long-term users (mostly >24 months). Therefore, the benefits with NSAID use may increase with longer use. In studies of aspirin as the only NSAID, the relative risk of AD was reduced 13%.81 A 2004 meta-analysis of 11 studies assessing the benefits of exposure to nonaspirin NSAIDs showed that the risk for development of AD was cut 50% with NSAID exposure.82 Among the prospective studies, the risk was reduced 26% for lifetime NSAID exposure and 58% for use of at least 2 years.82 Therefore, NSAID use may have a preventive benefit, but the appropriate timing of exposure remains to be studied. Studies of prednisone and a comparison of rofecoxib (a COX-2 inhibitor) and naproxen (an NSAID) showed no benefit in cognition measures in patients with AD.83,84 The benefits of NSAIDs vary and do not seem to extend after the onset of dementia. Therefore, NSAIDs are currently not considered to be an appropriate treatment for dementia. STATINS Cholesterol is synthesized only in the liver and brain. One of the enzymes involved in cholesterol synthesis is inhibited by the class of drugs used to treat dyslipidemia—statins. In the brain, cholesterol is synthesized primarily in astrocytes and is transported elsewhere through apolipoproteins, including APOE (a gene in which a type 4 allele is a risk factor for AD). The exact relationship between cholesterol levels and AD risk or progression is unclear. Serum cholesterol levels do not appear to correlate with risk of AD, and statin levels do not affect production of β amyloid in humans, although they do have an effect in vitro and in mice.85 However, Vol. 3, No. 8 n October 2005 REVIEW some recent case-control studies suggest decreased risk of AD with statins, but this is not fully supported by prospective studies.86-88 Statins may offer a neuroprotective or anti-inflammatory effect, rather than prevent accumulation of β-amyloid plaques.85 There are limited clinical studies of statins for AD. Atorvastatin showed some clinical benefit in cognition after 1 year of treatment (compared to placebo), but the difference was not statistically significant.89 It should be noted that this was a pilot study; the final participant numbers at 12 months were low (n = 46).89 Another study of simvastatin (6 months) showed significant reductions in cerebrospinal fluid levels of some but not all AD-related proteins (eg, tau, phosphorylated tau, β amyloid, and other proteins) and slight improvement in cognition.90 Clearly, more studies are needed, but thus far data do not support a role for statins in the treatment of AD. THERAPEUTIC CHOICES The American Psychiatric Association and the American Academy of Neurology (AAN) have published consensus guidelines on the treatment of patients with dementia.91-93 The American Geriatrics Society has endorsed the AAN guidelines, and guidelines for family physicians have also been published.94,95 All of these professional organizations recommend the use of acetylcholinesterase inhibitors for treatment of mild to moderate AD, noting comparable efficacy among the 3 drugs and the importance of clearly conveying expected outcomes to patients and family members/caregivers. All 3 guidelines recommend vitamin E or support consideration of its use to slow or delay disease progression, but they cite insufficient evidence to support the use of antiinflammatory medications in patients with AD.91-93,95 However, these guidelines were established before many of the NSAID or statin study publications. In fact, statins and memantine are not mentioned in any of the current guidelines. CONCLUSIONS The emerging details of AD pathophysiology provide possible therapeutic targets. β-amyloid plaques and NFTs are the long-held hallmarks of AD, but it appears that they (along with the reduced neuronal function and neurotransmitter availability) occur years before clinical symptoms emerge. Future treatment strategies will probably focus on the pathophysiologic changes in AD and address multiple mechanisms. In Advanced Studies in Nursing n the meantime, we have 4 drugs with proven efficacy, albeit modest, in at least some patients with AD. Although some may argue, based on clinical studies, that the effect of cholinesterase inhibitors or memantine is minimal, in reality any preservation of function and delay of nursing home placement in an individual patient has important and permanent consequences. The primary care nurse, in identifying and managing a patient with AD, needs to understand each of the following aspects of AD treatment: the expected outcomes with these drugs and their impact on the patient and caregiver, the importance of reiterating these expectations to the patient and caregiver, the common concurrent prescribing of cholinesterase inhibitors with anticholinergic drugs in older adults, the use of newer agents as possible preventive treatments for AD, and any updates in recommended treatment strategies from leading medical organizations. Because of the profound and sometimes rapid loss of memory and function with AD, the importance of trying at least 1 of these treatments in a patient with AD cannot be overstated. REFERENCES 1. Alzheimer’s Disease Education and Referral Center Web site. Alzheimer’s disease—unraveling the mystery. Available at: http://www.alzheimers.org/unraveling/01.htm. Accessed June 17, 2005. 2. Fox NC, Crum WR, Scahill RI, et al. Imaging of onset and progression of Alzheimer’s disease with voxel-compression mapping of serial magnetic resonance images. Lancet. 2001;358:201-205. 3. Kaye JA, Swihart T, Howieson D, et al. Volume loss of the hippocampus and temporal lobe in healthy elderly persons destined to develop dementia. Neurology. 1997; 48:1297-1304. 4. Forstl H, Zerfass R, Geiger-Kabisch C, et al. Brain atrophy in normal aging and Alzheimer’s disease. Volumetric discrimination and clinical correlations. Br J Psychiatry. 1995;167:739-746. 5. Cummings JL. Alzheimer’s disease. N Engl J Med. 2004;351:56-67. 6. Selkoe DJ. Defining molecular targets to prevent Alzheimer disease. Arch Neurol. 2005;62:192-195. 7. Bertram L, Tanzi RE. Alzheimer’s disease: one disorder, too many genes? Hum Mol Genet. 2004;13:R135-R141. 8. Walsh DM, Selkoe DJ. Deciphering the molecular basis of memory failure in Alzheimer’s disease. Neuron. 2004; 44:181-193. 9. Walker LC, Ibegbu CC, Todd CW, et al. Emerging prospects for the disease-modifying treatment of Alzheimer’s disease. Biochem Pharmacol. 2005;69:1001-1008. 267 REVIEW 10. Gilman S, Koller M, Black RS, et al. Clinical effects of Aβ immunization (AN1792) in patients with AD in an interrupted trial. Neurology. 2005;64:1553-1562. 11. Fox NC, Black RS, Gilman S, et al. Effects of Aβ immunization (AN1792) on MRI measures of cerebral volume in Alzheimer disease. Neurology. 2005;64:1563-1572. 12. Selkoe DJ. Alzheimer’s disease is a synaptic failure. Science. 2002;298:789-791. 13. Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297:353-356. 14. Perry EK, Tomlinson BE, Blessed G, et al. Correlation of cholinergic abnormalities with senile plaques and mental test scores in senile dementia. BMJ. 1978;2:1457-1459. 15. Francis PT. Glutamatergic systems in Alzheimer’s disease. Int J Geriatr Psychiatry. 2003;18(suppl 1):S15-S21. 16. Rogawski MA, Wenk GL. The neuropharmacological basis for the use of memantine in the treatment of Alzheimer’s disease. CNS Drug Rev. 2003;9:275-308. 17. Danysz W, Parsons CG, Möbius HJ, et al. Neuroprotective and symptomological action of memantine relevant for Alzheimer’s disease—a unified glutamatergic hypothesis on the mechanism of action. Neurotox Res. 2000;2:85-97. 18. Parsons CG, Danysz W, Quack G. Glutamate in CNS disorders as a target for drug development: an update. Drug News Perspect. 1998;11:523-569. 19. Abramov AY, Canevari L, Duchen MR. Calcium signals induced by amyloid beta peptide and their consequences in neurons and astrocytes in culture. Biochim Biophys Acta. 2004;1742:81-87. 20. Gordon-Krajcer W, Gajkowska B. Excitotoxicity-induced expression of amyloid precursor protein (beta-APP) in the hippocampus and cortex of rat brain: an electronmicroscopy and biochemical study. Folia Neuropathol. 2001;39:163-173. 21. Harkany T, Abraham I, Timmerman W, et al. β-amyloid neurotoxicity is mediated by a glutamate-triggered excitotoxic cascade in rat nucleus basalis. Eur J Neurosci. 2000;12:2735-2745. 22. Scott HL, Tannenberg AG, Dodd PR. Variant forms of neuronal glutamate transporter sites in Alzheimer disease cerebral cortex. J Neurochem. 1995;64:2193-2202. 23. Scott HL, Pow DV, Tannenberg AE, Dodd PR. Aberrant expression of the glutamate transporter excitatory amino acid transporter 1 (EAAT1) in Alzheimer’s disease. J Neurosci. 2002;22:RC206. 24. Butterfield DA, Griffin S, Munch G, Pasinetti GM. Amyloid beta-peptide and amyloid pathology are central to the oxidative stress and inflammatory cascades under which Alzheimer’s disease brain exists. J Alzheimers Dis. 2002:4:193-201. 25. Zhu X, Raina AK, Smith MA. Cell cycle events in neurons. Proliferation or death? Am J Pathol. 1999;155:327-329. 26. Zhu X, Lee HG, Casadesus G, et al. Oxidative imbalance in Alzheimer’s disease. Mol Neurobiol. 2005;31:205-218. 27. Kim SU, de Vellis J. Microglia in health and disease. J Neurosci Res. 2005;81:302-313. 28. McGeer P, McGeer EG. Inflammation, cytotoxicity, and Alzheimer disease. Neurobiol Aging. 2001;22:799-809. 29. Akiyama H, Barger S, Barnum S, et al. Inflammation and Alzheimer’s disease. Neurobiol Aging. 2000;21:383-421. 268 30. Mossner R, Schmitt A, Syagailo Y, et al. The serotonin transporter in Alzheimer’s and Parkinson’s disease. J Neural Transm Suppl. 2000;60:345-350. 31. Lai MK, Tsang SW, Alder JT, et al. Loss of serotonin 5HT2A receptors in the postmortem temporal cortex correlates with rate of cognitive decline in Alzheimer’s disease. Psychopharmacology. 2005;179:673-677. 32. Tsang SW, Lai MK, Francis PT, et al. Serotonin transporters are preserved in the neocortex of anxious Alzheimer’s disease patients. Neuroreport. 2003;14:1297-1300. 33. Heneka MT, Galea E, Gavriluyk V, et al. Noradrenergic depletion potentiates beta-amyloid-induced cortical inflammation: implications for Alzheimer’s disease. J Neurosci. 2002;22:2434-2442. 34. Herrmann N, Lanctot KL, Khan LR. The role of norepinephrine in the behavioral and psychological symptoms of dementia. J Neuropsychiatry Clin Neurosci. 2004;16:261-276. 35. Dietschy JM, Turley SD. Cholesterol metabolism in the brain. Curr Opin Lipidol. 2001;12:105-112. 36. Reiss AB. Cholesterol and apolipoprotein E in Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2005;20:91-96. 37. Launer LJ, White LR, Petrovitch H, et al. Cholesterol and neuropathologic markers of AD: a population-based autopsy study. Neurology. 2001;57:1447-1452. 38. Donepezil US prescribing information. Available at: http://www.aricept.com/pi/aricept_pi.htm#clinicalpharm. Accessed July 15, 2005. 39. Galantamine US prescribing information. Available at: http://www.us.reminyl.com/active/janus/en_US/assets/ rem/reminyl.pdf. Accessed July 15, 2005. 40. Memantine US prescribing information. Available at: http://www.namenda.com/pdf/namenda_pi.pdf. Accessed July 15, 2005. 41. Rivastigmine US prescribing information. Available at: http://www.pharma.us.novartis.com/product/pi/pdf/ exelon.pdf. Accessed July 21, 2005. 42. Rogers SL, Farlow MR, Doody RS, et al. A 24-week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer’s disease. Donepezil Study Group. Neurology. 1998;50:136-145. 43. Rogers SL, Doody RS, Mohs RC, Friedhoff LT. Donepezil improves cognition and global function in Alzheimer disease: a 15-week, double-blind, placebo-controlled study. Arch Intern Med. 1998;158:1021-1031. 44. Corey-Bloom J, Anand R, Veach J. A randomized trial evaluating the efficacy and safety of ENA 713 (rivastigmine tartrate), a new acetylcholinesterase inhibitor, in patients with mild to moderately severe Alzheimer’s disease. Int J Geriatr Psychopharmacol. 1999;1:55-65. 45. Anand R, Messina J, Hartmann R. Dose-response effect of rivastigmine in the treatment of Alzheimer’s disease. Int J Geriatr Psychopharmacol. 2000;2:68-72. 46. Rosler M, Anand R, Cicin-Sain A, et al. Efficacy and safety of rivastigmine in patients with Alzheimer’s disease: international randomised controlled trial. BMJ. 1999;318:633-638. 47. Raskind MA, Peskind ER, Wessel T, et al. Galantamine in AD: a 6-month randomized, placebo-controlled trial with a 6-month extension. Neurology. 2000;54:2261-2268. 48. Tariot PN, Solomon PR, Morris JC, et al. A 5-month, randomized, placebo-controlled trial of galantamine in AD. Neurology. 2000;54:2269-2276. Vol. 3, No. 8 n October 2005 REVIEW 49. Wilcock GK, Lilienfeld S, Gaens E. Efficacy and safety of galantamine in patients with mild to moderate Alzheimer’s disease: multicenter randomized controlled trial. BMJ. 2000;321:1445-1449. 50. Rockwood K, Mintzer J, Truyen L, et al. Effects of a flexible galantamine dose in Alzheimer’s disease: a randomized, controlled trial. J Neurol Neurosurg Psychiatry. 2000;71:589-595. 51. Rogers SL, Doody RS, Pratt RD, Ieni JR. Long-term efficacy and safety of donepezil in the treatment of Alzheimer’s disease: final analysis of a US multicenter open-label study. Eur Neuropsychopharmacol. 2000;10:195-203. 52. Karaman Y, Erdogan F, Koseoglu E, et al. A 12-month study of the efficacy of rivastigmine in patients with advanced moderate Alzheimer’s disease. Dement Geriatr Cogn Disord. 2005;19:51-56. 53. Farlow M, Anand R, Messina J Jr, et al. A 52-week study of the efficacy of rivastigmine in patients with mild to moderately severe Alzheimer’s disease. Eur Neurol. 2000;44:236-241. 54. Grossberg G, Irwin P, Satlin A, et al. Rivastigmine in Alzheimer disease. Efficacy over two years. Am J Geriatr Psychiatry. 2004;12:420-431. 55. Dorwaiswamy PM, Krishnan KR, Anand R, et al. Long-term effects of rivastigmine in moderately severe Alzheimer’s disease. Does early initiation of therapy offer sustained benefits? Prog Neuropsychopharmacol Biol Psychiatry. 2002;26:705-712. 56. Lyketsos CG, Reichman WE, Kershaw P, Zhu Y. Long-term outcomes of galantamine treatment in patients with Alzheimer disease. Am J Geriatr Psychiatry. 2004;12:473-482. 57. Raskind MA, Pesking ER, Truyen L, et al. The cognitive benefits of galantamine are sustained for at least 36 months: a long-term extension trial. Arch Neurol. 2004;61:252-256. 58. Pirttila T, Wilcock G, Truyen L, Damaraju CV. Long-term efficacy and safety of galantamine in patients with mild to moderate Alzheimer’s disease: multicenter trial. Eur J Neurol. 2004;11:734-741. 59. Seltzer B, Zolnouni P, Nunez M, et al. Efficacy of donepezil in early stage Alzheimer disease: a randomized placebo-controlled study. Arch Neurol. 2004;61:1852-1856. 60. Feldman H, Gauther S, Hecker J, et al. A 24-week, randomized, double-blind study of donepezil in moderate to severe Alzheimer’s disease. Neurology. 2001;57:613-620. 61. Farlow M, Hake A, Messina J, et al. Response of patients with Alzheimer disease to rivastigmine treatment is predicted by the rate of disease progression. Arch Neurol. 2001;58:417-422. 62. Almkvist O, Darreh-Shori T, Stefanova E, et al. Preserved cognitive function after 12 months of treatment with rivastigmine in mild Alzheimer’s disease in comparison with untreated AD and MCI patients. Eur J Neurol. 2004;11:253-261. 63. Hope T, Keene J, Gedling K, et al. Predictors of institutionalization for people with dementia living at home with a carer. Int J Geriatr Psychiatry. 1998;13:682-690. 64. Mohs RC, Doody RS, Morris JC, et al. A 1-year placebocontrolled preservation of function survival study of donepezil in AD patients. Neurology. 2001;57:481-488. 65. Feldman H, Gauther S, Hecker J, et al. Efficacy of donepezil on maintenance of activities of daily living in patients with moderate to severe Alzheimer’s disease and Advanced Studies in Nursing n the effect on caregiver burden. J Am Geriatr Soc. 2003;51:737-744. 66. Potkin SG, Anand R, Hartman R, et al. Impact of Alzheimer’s disease and rivastigmine on activities of daily living over the course of mild to moderately severe disease. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26:713-720. 67. Galasko D, Kershaw PR, Schneider L, et al. Galantamine maintains ability to perform activities of daily living in patients with Alzheimer’s disease. J Am Geriatr Soc. 2004;52:1070-1076. 68. Sano M, Wilcock GK, van Baelen B, Kavanagh S. The effects of galantamine treatment on caregiver time in Alzheimer’s disease. Int J Geriatr Psychiatry. 2003;18:942-950. 69. Tariot PN, Jakimovich L. Donepezil use for advanced Alzheimer’s disease-a case study from a long-term care facility. J Am Med Dir Assoc. 2003;4:216-219. 70. Geldmacher DS, Provenzano G, McRae T, et al. Donepezil is associated with delayed nursing home placement in patients with Alzheimer’s disease. J Am Geriatr Soc. 2003;51:937-944. 71. AD2000 Collaborative Group. Long-term donepezil treatment in 565 patients with Alzheimer’s disease (AD2000): randomized double-blind trial. Lancet. 2004;363:2105-2115. 72. Wilcock G, Howe I, Coles H, et al. A long-term comparison of galantamine and donepezil in the treatment of Alzheimer’s disease. Drugs Aging. 2003;20:777-789. 73. Carnahan RM, Lund BC, Perry PJ, Chrischilles EA. The concurrent use of anticholinergics and cholinesterase inhibitors: rare event or common practice? J Am Geriatr Soc. 2005;52:2082-2087. 74. Reisberg B, Doody R, Stoffler A, et al. Memantine in moderate-to-severe Alzheimer’s disease. N Engl J Med. 2003;348:1333-1341. 75. Tariot PN, Farlow MR, Grossberg GT, et al. Memantine treatment in patients with moderate to severe Alzheimer disease already receiving donepezil. A randomized controlled trial. JAMA. 2004;291:317-324. 76. Berman K, Brodaty H. Tocopherol (vitamin E) in Alzheimer’s disease and other neurodegenerative disorders. CNS Drugs. 2004;18:807-825. 77. Kontush K, Schekatolina S. Vitamin E in neurodegenerative disorders: Alzheimer’s disease. Ann N Y Acad Sci. 2004;1031:249-262. 78. Petersen RC, Thomas RG, Grundman M, et al. Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med. 2005;352:2379-2388. 79. Miller ER III, Pastor-Barriuso R, Dalal D, et al. Meta-analysis: high-dosage vitamin E supplementation may increase allcause mortality. Ann Intern Med. 2005;142:37-46. 80. Letters to the editor. High dosage vitamin E supplementation and all-cause mortality. Ann Intern Med. 2005;143:150-158. 81. Etminan M, Gill S, Samii A. Effect of non-steroidal antiinflammatory drugs on risk of Alzheimer’s disease: systematic review and meta-analysis of observational studies. BMJ. 2003;327:128-132. 82. Szekely CA, Thorne JE, Zandi PP, et al. Nonsteroidal antiinflammatory drugs for the prevention of Alzheimer’s disease: a systematic review. Neuroepidemiology. 2004;23:159-169. 83. Aisen PS, Davis KL, Berg JD, et al. A randomized controlled 269 REVIEW trial of prednisone in Alzheimer’s disease. Alzheimer’s Disease Cooperative Study. Neurology. 2000;54:588-593. 84. Aisen PS, Schafer KA, Grundman M, et al. Effects of rofecoxib or naproxen vs placebo on Alzheimer disease progression: a randomized controlled trial. JAMA. 2003;289:2819-2826. 85. Wolozin B. Cholesterol, statins and dementia. Curr Opin Lipid. 2004;15:667-672. 86. Wolozin B, Kellman W, Ruosseau P, et al. Decreased prevalence of Alzheimer disease associated with 3-hydroxy3-methyglutaryl coenzyme A reductase inhibitors. Arch Neurol. 2000;57:1439-1443. 87. Jick H, Zornberg GL, Jick SS, et al. Statins and the risk of dementia. Lancet. 2000;256:1627-1631. 88. Zandi PP, Sparks DL, Khachaturian AS, et al. Do statins reduce risk of incident dementia and Alzheimer disease? The Cache County Study. Arch Gen Psychiatry. 2005;62:217-224. 89. Sparks DL, Sabbagh MN, Connor DJ, et al. Atorvastatin for the treatment of mild to moderate Alzheimer disease. Arch Neurol. 2005;62:753-757. 90. Sjogren M, Gustafsson K, Syversen S, et al. Treatment with simvastatin in patients with Alzheimer’s disease lowers both alpha- and beta-cleaved amyloid precursor protein. Dement Geriatr Cogn Disord. 2003;16:25-30. 270 91. American Psychiatric Association. Practice guideline for the treatment of patients with Alzheimer’s disease and other dementias of late life. Am J Psychiatry. 1997;154(suppl 5):1-39. 92. Rabins PV. Guideline watch. Practice guideline for the treatment of patients with Alzheimer’s disease and other dementias of late life. American Psychiatric Association Web site. Available at: www.psych.org/psych_pract/treatg/pg/ AlzWatch_081704.pdf. Accessed July 13, 2005. 93. Doody RS, Stevens JC, Beck C, et al. Practice parameter: management of dementia (an evidence-based review). Neurology. 2001;56:1154-1166. 94. American Geriatrics Society Web site. Position statementclinical practice guidelines. Guidelines abstracted from the American Academy of Neurology’s Dementia Guidelines for Early Detection, Diagnosis, and Management of Dementia. Available at: http://www.americangeriatrics.org/products/positionpapers/aan_dementiaPF.shtml. Accessed June 11, 2005. 95. Cummings JL, Frank JC, Cherry D, et al. Guidelines for managing Alzheimer’s disease: Part II. Treatment. Am Fam Physician. 2002;65:2525-2534. Vol. 3, No. 8 n October 2005