* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Role Of The Oncology Registered Nurse
Harm reduction wikipedia , lookup
Nurse anesthetist wikipedia , lookup
Medical ethics wikipedia , lookup
Patient safety wikipedia , lookup
Nurse–client relationship wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Nanomedicine wikipedia , lookup
Electronic prescribing wikipedia , lookup
Licensed practical nurse wikipedia , lookup
The Role of the Oncology Registered Nurse In Outpatient Medical Oncology The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Acknowledgements “The Role of the Oncology Registered Nurse in Outpatient Medical Oncology” would not have been possible without the input and expertise provided by Eric Berger, Bridget Culhane, Cynthia Fisher, Laura Fennimore, Ilisa Halpern, Kris Hartigan, Gail Mallory, Pearl Moore, Julie Painter, Dianne Richardson, Paula Sherwood, Kathleen Shuey, and Karen Stanley. The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Table of Contents Introduction 1 Section One: Pretreatment 3 Section Two: Treatment 18 Section Three: Additional Clinical Responsibilities 28 Section Four: Oral Chemotherapy 34 Section Five: Case Study 36 Definitions 40 References 44 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Introduction A diagnosis of cancer is a frightening and life-changing event. The individual and his/ her family fear the worst as they face the unknown, undergo a variety of treatment options and procedures and experience the side effects of therapy that can alter their quality of life. The impact of cancer on an individual’s life correlates with the degree of change and disruption experienced. In today’s world, patients in the midst of treatment continue to care for families, work, and face life with the resources that are available. The registered nurse’s ability to provide patient and family education across the illness and treatment continuum assists patients to adjust to the realities of the illness, cope more effectively, and reduces anxiety. The registered nurse’s skills in thorough assessment and intervention significantly impact patient outcomes. Research verifies that ongoing nursing communication, assessment, and intervention can reduce readmission rates and assist in the early diagnosis of problems so that patients experience fewer complications. The purpose of this document is to provide information on the unique needs of cancer patients and their families and the responsibility and unique contributions of the registered nurses who care for them. This document has been developed through a collaborative partnership between nurses representing the Oncology Nursing Society and US Oncology. The mission of both organizations is to promote quality patient care. The document explains and details services that may be provided during the care of the patient and family in an outpatient oncology setting/facility. Of note are the numerous interventions (such as delivery of chemotherapy/biotherapy, treatment of a disease by means of chemical substances or drugs, and management of side effects of therapy) requiring the unique contribution of the registered nurse with oncology specific training and competencies. Registered nurses enhance quality care by utilizing state-of-the-art knowledge and the skills of assessment, planning, intervention(s), and evaluation and provide the safest environment for the patient and family. Chemotherapeutic agents used for treating cancer are available in various forms. The form (route of administration) may depend on patient capability to receive the medication in that way or the requirements of a specific chemotherapeutic regimen/ treatment plan. Routes of chemotherapy administration include: topical (rubbed onto the skin), oral (by mouth in pill form), intravenous (administered through a catheter inserted into the patient’s vein in the arm, neck or chest), intrathecal (administered via a catheter inserted into the patient’s cerebrospinal fluid), via ommaya reservoir (administered through a device that allows the medication to enter ventricular spaces in the brain), and intraperitoneal (administered into the peritoneal /abdominal cavity). All routes of chemotherapy require safe and consistent delivery. Many patients will require surgical or radiologic placement of central venous access devices (intravenous devices that are placed into large veins in the upper chest) while other devices such as peripherally inserted central catheters may be placed by a specially trained registered nurse into a large vein in the arm. As these devices provide a direct line of infusion to major blood vessels supplying the heart, they 1 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology require meticulous care to prevent infection, regular dressing changes, and intermittent flushing with solutions that prevent the blood from clotting and keep the line open. This document is divided into key sections or treatment phases. Each phase details specific healthcare provider interventions and essential registered nurse interventions along the continuum of outpatient medical oncology care. ¾ Section One, the Pre-Treatment phase, addresses interventions prior to the actual initiation of chemotherapy. ¾ Section Two, the Treatment Phase, addresses those interventions that occur from the time therapy is initiated until all drug delivery devices (catheters used to deliver therapy into a vein, the cerebrospinal fluid, or ventricular spaces in the brain) are removed from the patient. ¾ Section Three, Additional Clinical Responsibilities, addresses interventions that might occur more frequently and/or intermittently across the treatment continuum − ongoing education, reinforcement of previously given information, symptom/side effect management, management of intravenous devices, and other issues as they arise, as well as those responsibilities focusing on documentation and telephone triage. ¾ Section Four, Oral Chemotherapy, addresses those unique interventions required when patients are self-administering chemotherapy in the home setting. ¾ Section Five includes case scenarios with examples of patient treatment experiences and nursing interventions. 2 3 X X X X X X X X X X X X X X ¾ Current allergies to medication, food, and environmental factors. ¾ Nutritional status. Review and update medication list and check for incompatibilities or drug interactions. Discuss potential interactions with physician and/or pharmacist to determine if changes need to be made. ¾ Currently prescribed medications. ¾ Over-the-counter medications. emphysema). gastrointestinal, genitourinary, musculoskeletal, lymph nodes and related swelling, blood cells, nervous system, and particular body chemistries. Comprehensive physical assessment: ¾ Coexisting health problems (e.g., cardiac history, diabetes, Requires Registered Nurse ¾ History and physical examination (determines current condition). ¾ Review of systems: head and neck, skin, respiratory, cardiovascular, First Visit X X X X X X Each Visit X X X Patient assessment: physical and psychosocial. Section One: Pretreatment The following sections describe the responsibilities of the registered nurse in medical oncology and activities associated with caring for patients receiving chemotherapy or biotherapy. Some of the activities described can be performed by clinical staff other than the registered nurse (e.g., a pharmacist) or by technical staff who are supervised by the registered nurse. Duties that are exclusively the responsibility of the oncology nurse are noted. In addition, the frequency of activity is listed. Activities may occur on the first day of chemotherapy (first visit), at each chemotherapy visit, each time a chemotherapy agent is given by IV push or IV infusion, at each cycle (chemotherapy agents are given for a predetermined time frame [e.g., a group of chemotherapy agents may be given for three days every 21 days and the patient’s response to treatment evaluated at the end of each cycle]), or some other frequency. The Role of the Oncology Registered Nurse In Outpatient Medical Oncology As Needed Each Cycle Each Infusion Each IV Push 4 X X X X Develop or revise the plan of care based on assessment data and consult with other members of the healthcare team as necessary. Based on a comprehensive patient assessment, the physician and/or registered nurse may find it necessary to alter the treatment plan (e.g., adjusting chemotherapy dosages or delay of treatment) or provide pretreatment interventions (e.g., blood transfusion). Comprehensive psychosocial assessment of patient and family: Tumor marker studies (some cancers have markers that indicate the reduction or progression of the cancer); assessment frequency varies based on disease. Renal function studies. Liver function studies. Comprehensive metabolic panel (blood chemistry tests). X X X X X X X X X ¾ ¾ ¾ ¾ X X X X X X X X Each Cycle infection, red cells that carry oxygen to the body and help with fatigue problems, and platelets that assist with clotting. X X X X X As Needed ¾ Complete blood count: white blood cells that fight bacterial and viral X X X X First Visit Examples of laboratory values may include: Requires Registered Nurse X Each Visit Obtain and review laboratory results to determine if they are within an acceptable range as set by the practice. Chemotherapy destroys rapidly dividing cells, both normal (hair follicles, lining of the gastrointestinal tract, reproductive tract, and blood cells) and malignant cells. Assess laboratory values in light of expected side effects (e.g., decreased blood counts) and unanticipated complications of previously administered therapies. Alert the physician regarding laboratory results that may impact the chemotherapy regimen. ¾ Complementary and/or alternative medications or therapies. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Infusion Each IV Push First Visit X X X X X Requires Registered Nurse X X X X X ¾ Psychologic distress that includes sadness, depression, anxiety, anger, and feelings of loss of control. ¾ Disruption of family dynamics (e.g., role changes). Validate patient and family concerns and feelings. Allow adequate time for listening. Make appropriate referrals or consultations in collaboration with the multidisciplinary healthcare team for more comprehensive assessment and intervention as necessary. 5 X X X X X X X X X X X X X X Assess learning needs, and develop and gather appropriate materials. Discuss with patient and family and provide written materials as needed: ¾ Drug and/or dietary interactions that may occur and their management. Importance of maintaining appropriate schedule as prescribed and notification of healthcare team if that is not possible (especially when oral chemotherapy drugs are prescribed). See Section Four. X X Each Cycle Chemotherapy and administration issues: ¾ General medication side effects (for any prescriptions currently taken). ¾ Prevention or detection measures for concerned family members. ¾ Cancer or disease process and impact on the individual. X X Confirm patient identification. X X X X X X X X As Needed Preprocedure education (may be reinforced postprocedure). X X X X Each Visit ¾ Need for outside services. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Infusion Each IV Push 6 X X X X X X ¾ Analgesics for pain control. Information about central venous access device (CVAD) (i.e., an IV device placed into large veins in the upper chest). Symptom identification and management. Side effects of chemotherapy are to be taken seriously. If they are not well managed, patients may be hospitalized, treatment regimens delayed, and lives risked. The registered nurse must interpret X X ¾ Drugs that prevent or control nausea and vomiting during and after chemotherapy. X X X X ¾ Growth factors (drugs which stimulate the body’s bone marrow to make white blood cells or red blood cells). X X X Supportive care medications used to control cancer and treatmentrelated symptoms: ¾ Potential for changes in the regimen or schedule based on laboratory values or other diagnostic tests. X X X X X X ¾ Ongoing plan established by physician and patient. X X X X X X Requires Registered Nurse Treatment schedule (e.g., daily for four days, every Tuesday for four weeks): X X Each Visit X X X Each Cycle X X X As Needed ¾ Vesicant drug issues: Some chemotherapy agents have the potential to cause severe tissue damage if accidentally leaked into tissue around the vein; describe symptoms such as burning or stinging at the site so that the patient may notify the nurse if they occur during administration of the chemotherapy agent. X Each IV Push ¾ IV-related complications (e.g., swelling, redness, discoloration of veins). First Visit X X Each Infusion ¾ Side effects and toxicities. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 7 X X X X X X ¾ Vomiting: Restrict intake of food and fluid leading to malnutrition and severe dehydration, as well as electrolyte imbalance. If ongoing despite prescribed drug therapy, blood tests may be required to assess for dehydration. A different form of nutritional support may be necessary. Call the healthcare team if unable to keep fluids or food down. Report duration of the problem and the number of vomiting episodes. ¾ Diarrhea: Can lead to significant fluid loss leading to severe dehydration. Take antidiarrhea medications as prescribed and drink fluids as prescribed. Monitor frequency of episodes and report problem to healthcare team if nonresponsive to prescribed interventions. May require laboratory assessment and further intervention. ¾ Constipation: Can lead to straining, trauma to rectal tissue, risk of X X Requires Registered Nurse ¾ Nausea: If nausea is present, take antinausea medications as prescribed, and focus on multiple small meals and cold foods without aromas. First Visit X Each Visit X Each IV Push ¾ Chills: Monitor for presence of chills and/or shaking, which may be a sign of infection or neurologic reaction. Notify the healthcare team. Each Infusion X Each Cycle X As Needed ¾ Fever: Monitor the patient’s temperature. Even a slight fever in a patient who has received chemotherapy may indicate an infection that is life threatening. Report a fever immediately to healthcare team. Fever may require further assessment (e.g., blood or other tissue cultures, antibiotics). Instruct patient and family members or caregivers and provide written materials as needed regarding: information from patients and families who report unmanaged symptoms and ensure that proper care is provided. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology First Visit Requires Registered Nurse 8 X X X X X X ¾ Shortness of breath: May indicate respiratory distress resulting from respiratory infection, blood clots in the lung, cardiac complications, bleeding, severe fatigue, or severe pain. Call the healthcare team if shortness of breath has a sudden or unexpected onset. ¾ Anorexia: A loss of desire to eat can result in malnutrition. Notify the healthcare team if this occurs. Monitor weight loss. Alternate sources of nutrition may be prescribed. Small, frequent meals may help. ¾ Neurotoxicity: This is a change in sensation and/or feeling in the extremities. If the hands are numb or sensation is changing, avoid holding hot or very cold items and typical household tasks such as washing dishes or putting items in a hot oven. Notify the healthcare team regarding symptoms. X Each Visit X Each IV Push ¾ Bleeding or bruising: May be a sign of low platelet count (i.e., cells that help to clot the blood). Avoid sharp instruments and rigorous physical activity, and call the healthcare team if significant injury occurs or bleeding cannot be stopped. Aspirin and other medications that interfere with blood clotting should not be taken unless the physician has indicated they can be taken. Notify the healthcare team if bleeding is frequent or cannot be stopped. Each Infusion X Each Cycle X As Needed ¾ Mouth ulcers: Watch for mouth ulcers or inflammation of the oral tissue. Use medications to control discomfort as prescribed. Cold foods and icy nutritional drinks may be easier to tolerate. Call the healthcare team if food and fluid intake is restricted, pain does not respond to prescribed medications, or fever develops. infection in the traumatized tissues, and fecal impaction (i.e., intestines blocked with stool). Take constipation medications (e.g., stool softeners, laxatives) as prescribed, drink plenty of fluids, carefully monitor bowel movements, and notify the healthcare team if constipation is not responsive to interventions. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology X X Reinforce patient education from previous visits and ensure family members understand the information. Check to ensure that written materials have been provided to all who will need them. Emphasize the need to notify the healthcare team if problems arise between visits. 9 ¾ IV catheter. ¾ Appropriate occlusive dressing that covers the IV site. ¾ Tape. For a peripheral IV start, assemble supplies: Gather and prepare IV supplies. Determine the type of IV access. (CVAD versus an IV line placed into veins of the hand or lower arm known as a peripheral IV). X X X X X X X X X X X X X X X functional.) ¾ Program the pump. ¾ Test the alarm. ¾ Evaluate the electrical safety. X X X X Each IV Push X Each Cycle ¾ Equipment maintenance. (Verify that equipment is clean and X Each Infusion Prepare the pump (i.e., a mechanical device used to regulate the rate of infusion of chemotherapy drugs) for use. X Each Visit Gather and prepare equipment (e.g., IV pole, table). Prepare the room after confirming patient identification. X X Requires Registered Nurse Provide a list of healthcare team members (e.g., physicians, registered nurses, pharmacists) and their phone numbers to contact for problems. Reinforce the importance of reporting symptoms as previously described. Therapy may be interrupted if timely intervention is not provided. As Needed X First Visit Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 10 X X X X X X X X X Assemble catheter flush supplies: X X X X X X X X X X Requires Registered Nurse ¾ Topical anesthetic applied prior to accessing device with port needle. ¾ Appropriate needle for implanted pump. First Visit X Heparin flush or solution and tubing to maintain patency. Heparin cap. Alcohol wipes. Antiseptic wipes. Mask. Gloves. Tape. Appropriate occlusive dressing that covers the site. X X Each IV Push Additional supplies and equipment for implanted pump (i.e., device implanted during a surgical procedure to deliver continuous chemotherapy to a specific tumor site such as the liver via the hepatic artery). ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ For CVAD, assemble supplies: /no clots or sluggish flow and easily infuses with good blood return). ¾ Heparin flush or solution and tubing to maintain IV patency (IV is open Heparin cap (placed on the end of a peripheral or central line to maintain a closed, sterile system). Alcohol wipes. Antiseptic wipes. Each Infusion X X X X Each Cycle X X X X Each Visit Gloves. As Needed ¾ ¾ ¾ ¾ Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology First Visit 11 X X X X X Preparation of chemotherapy requires extensive knowledge on the part of the registered nurse or oncology-specialized pharmacist to safely interpret chemotherapy orders and correctly perform the verification of: ¾ Drug dosages (chemotherapy drugs have varying doses based on the ¾ Administration route for each chemotherapy drug. (Administering chemotherapy via the incorrect route can be harmful and even result in death.) actual therapy or protocol). X X Obtain, verify, and re-verify patient consent as needed. X X X X Each Cycle Verify insurance coverage (does not require a registered nurse or pharmacist to verify directly with the insurance company). However, before preparing expensive chemotherapy, the registered nurse or pharmacist must be certain the verification was made. Prepare chemotherapy. Chemotherapy hazardous waste container. Goggles (as needed to prevent exposure). Mask (as needed to prevent exposure). Chemotherapy gown. X X X X X X X X X X X Special chemotherapy-protective gloves. ¾ ¾ ¾ ¾ ¾ Requires Registered Nurse X Each IV Push X Each Infusion Gather and use personal protective equipment to protect clinical staff (e.g., registered nurse, pharmacist) from exposure to chemotherapy. X Each Visit X X X X X X As Needed ¾ Flush solution (heparin or saline). ¾ Syringe. ¾ Needleless connector. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 12 ¾ ¾ ¾ ¾ Tubing: Certain chemotherapy agents require special IV tubing and/ Chemotherapy agents (in vials from manufacturer). Antiemetic agents (in vials from manufacturer). IV fluids. Assemble supplies for drug preparation: maximum dosage that can be given. This should be calculated and monitored to ensure that the dosage is not exceeded regardless of the patient’s BSA. For example, doxorubicin is used for many tumors and has a maximum dosage set to reduce the potential for cardiac damage.) ¾ Maximum dose of drug. (Particular chemotherapy drugs have a patient’s body surface area [BSA], which is a formula based on height and weight that is used in determining appropriate chemotherapy drug doses.) ¾ Calculated dose. (Most chemotherapy drugs are dosed according to written document that includes specific details of a research project, including drug information, how to administer the drug, patient eligibility, etc.). ¾ Physician orders per community standard or research protocol (i.e., a of several-hour infusion could result in serious harm and even death to the patient.) ¾ Infusion time. (Inappropriate infusion times such as IV push instead X X X X X X X X X X X X X X X X X X X X X X X First Visit X Requires Registered Nurse awareness of U.S. Food and Drug Administration-approved indications as well as approved “off-label” use). Each Visit X X Each IV Push X X Each Infusion ¾ Drug compatibility and/or interactions. ¾ Drugs ordered (must be approved for the diagnosis, which requires Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology As Needed Each Cycle First Visit 13 X X X X ¾ Operating the hood continuously (i.e., 24 hours per day). ¾ Inspecting and certifying the cabinet every six months. when the hood is serviced or moved. and at the end of each workday. ¾ Decontaminating the cabinet weekly, whenever a spill occurs, or Each Cycle X As Needed ¾ Cleaning the cabinet each day prior to use, whenever a spill occurs, X X X Document expiration dates of chemotherapy drugs. X X X Document the lot number of chemotherapy drugs. This allows for tracking of each drug that is administered. Use the Certified Biological Safety Cabinet (needed to safely prepare drugs and prevent exposure of pharmacy or nursing staff to aerosolization of chemotherapy agents). Preparation and maintenance include: X X X X X Assess drug stability. The registered nurse or pharmacist needs to know how long drugs are stable in solution so that they are prepared in the correct time frame, stored in the correct environment to maintain drug potency and stability, and delivered in a safe and timely fashion. X X Prepare the label for all IV fluids (for injection or infusion). X Requires Registered Nurse X X Each Visit Assess the patient and drug for proper solution. In many instances, the volume and type of IV fluid that a chemotherapy agent is diluted in may be determined by the individual patient’s need for IV fluids. For example, patients with diabetes need to receive chemotherapy drugs diluted in normal saline (rather than dextrose) if the specific drug and fluid are compatible. X Each IV Push and placing in either a syringe for injection or IV fluid for infusion. Each Infusion ¾ Syringes, alcohol preps, and needles for removing solution from vials or the use of an in-line IV filter to eliminate undiluted particles. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 14 X X X X X X ¾ Don chemotherapy gown and gloves, as well as a mask and goggles if ¾ Place a plastic-backed paper drape on the counter surface of the ¾ Verify that the glass shield on the biologic safety cabinet is only open biologic safety cabinet. appropriate. X X Mix chemotherapy agents in biologic safety cabinet. A registered nurse, pharmacist, or pharmacy technician under the supervision of a pharmacist must mix the chemotherapy. Some states do not allow pharmacy technicians to prepare chemotherapy. Chemotherapy drugs are carcinogenic (i.e., can cause cancer) and need to be prepared under circumstances that minimize exposure to the person preparing the chemotherapy and to the environment. X X X X X X X X X X X X X X chemotherapy-induced diarrhea or severe nausea and vomiting in an effort to avoid hospitalization. This also reduces the risk of bleeding (hemorrhage) in the bladder. ¾ IV fluids: Patients may need to receive IV hydration because of patients who have infections in an effort to avoid hospitalization. cancer therapies can destroy bone mass, causing elevated serum calcium. This can lead to confusion, seizures, and/or death. Confer with the physician if laboratory data indicate the need for increased red or white blood cells that can be managed with growth factors. ¾ Antiemetic agents for the prevention of nausea and/or vomiting. ¾ Growth factors for low red blood cell or white blood cell counts: Prepare supportive care agents. X Requires Registered Nurse X First Visit ¾ Antibiotics: Oncology practices often administer IV antibiotics to Each Visit X Each IV Push X Each Infusion ¾ Bisphosphonates to lower blood calcium levels: Some tumors and/or Each Cycle X X X As Needed X X X Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology X X X X X X X ¾ Clear all liquid from needle or hub prior to removing the needle from ¾ Withdraw the needle or syringe from the vial without spilling contents Requires Registered Nurse X X X First Visit ¾ Attach the needle (or needleless system) to the syringe. ¾ Insert the needle correctly into the vial to prevent coring. ¾ Using aseptic technique, withdraw medication from the vial taking Each Visit X 15 X X X X X X X X X X X X ¾ For infusion, inject the chemotherapy dose into the solution. ¾ Clean the additive port on the solution container prior to and after ¾ Properly mix contents and perform a final inspection. ¾ Place a tamper-proof seal on additive port. ¾ Place a cap on the end of the tubing to maintain sterility, maintain ¾ Wipe the bag with an alcohol prep to remove any possible chemotherapy contamination. stability of product, and prevent leakage. injecting chemotherapy. vial). X X X X X X ¾ If reconstituting a powder, draw up correct amount of diluent. ¾ Inject diluent into vial. ¾ Mix contents of vial, diluent, and powder (with needle remaining in in the Biological Safety Cabinet. the closed vial. care not to touch any internal part of the plunger when pulling back. X X X X X X X X X Each IV Push X X X X X X X X X X X X X X X X Each Infusion rubber diaphragm. X X X X X X X X X X X X X X X Each Cycle ¾ If withdrawing from a vial, remove the dust cover and clean the 8" to prevent exposure to chemotherapy agents. Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology As Needed X Prepare syringes with normal saline to flush IV line between administration of each agent. 16 X X X X Obtain vital signs. (Findings may signal body system abnormalities necessitating postponement of treatment.) ¾ Blood pressure. Obtain vital signs. X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X As Needed ¾ Reorder drugs. ¾ Restock drugs. (Must wear personal protective equipment). Inventory management: X X X X Prepare IV chemotherapy. Fill IV tubing with a nonchemotherapy IV fluid (such as normal saline). X X X X X X X X ¾ Amount of drug to be instilled into solution for infusion. ¾ Dose calculations. X X X prescribed dose to reduce waste and decrease cost.) ¾ Vial sizes. (Use a combination of vial sizes that comes closest to the is being admixed.) ¾ Original chemotherapy order. ¾ Drug being prepared. (Look at the original vial to verify correct drug Double check: drug-disposal container per federal regulations. X X X X X ¾ Print and apply the drug label to the mixture. ¾ Dispose of contaminated equipment in an appropriate hazardous X Each Infusion X X X X X Each IV Push sterility, maintain stability of product, and prevent leakage. Each Cycle X X X First Visit ¾ For an IV push, place the cap on the end of the syringe to maintain Requires Registered Nurse Each Visit Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology X X Obtain height. Obtain weight. X X X X X X ¾ BSA (formula using height and weight) OR ¾ Area under the curve (AUC). ¾ Verify BSA or AUC with orders and dose recommendations. Inaccurate calculations of BSA have resulted in 18% of the serious preventable adverse drug events when practitioners have insufficient information about the patient. X X Each IV Push Calculate the appropriate chemotherapy dosage. An inaccurate chemotherapy or biotherapy dosage could result in over- or underdosing of agents. Verify dosing based on: Each Infusion X X X X Each Cycle X X X X X X As Needed X X X First Visit ¾ Pulse and respiratory rate. ¾ Temperature. Requires Registered Nurse Each Visit Section One: Pretreatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 17 Each Cycle Each Infusion Each IV Push Each Visit First Visit Requires Registered Nurse As Needed 18 Arterial access device: This implanted device resembles a port but have a mechanism that delivers chemotherapy into the hepatic (liver) artery. The device allows for the delivery of chemotherapy into a specific region of the body thus providing a higher concentration of chemotherapy at the tumor site. ¾ Implanted pumps: (CVAD). Chemotherapy can be very caustic to the veins, and repeated exposure to chemotherapy can sclerose (harden) veins or cause them to be very fragile, thus making a peripheral IV difficult to insert. Fragile veins can easily be punctured during insertion of the peripheral IV, thus necessitating multiple attempts at placing the IV. In these instances, an implanted device called a port can be surgically placed under the patient’s skin. A small tube that is connected to the port is threaded into the large vein in the chest cavity. The port has a reservoir made of titanium with a self-sealing access portion that allows a needle to be placed through the port to remove blood for sampling or deliver a variety of medications (including chemotherapy) and fluids into the patient’s bloodstream. External catheters also can be placed in the large vein in the chest cavity. These catheters are partially external and generally held in place with stitches in the skin. ¾ Central venous access methods: Central venous access requires that an IV device is placed into a large vein in the upper chest IV push: A primary bag of IV fluids is hung and slowly drips into the patient’s vein. The registered nurse slowly pushes the chemotherapy agent into a side port of the primary bag’s IV tubing. Chemotherapy agents known as vesicants must be administered in this manner. Because the vesicant drug has the potential to cause severe damage, including tissue death, if any of the medication is allowed to leak into the tissues around the vein, the registered nurse must constantly monitor the rate of delivery and the condition of the site where the IV is placed. IV piggyback: A primary (main) bag of IV fluids, usually saline solution, is hung and the chemotherapy solution is connected (piggybacked) into a side port of the tubing of the primary fluid. This technique further dilutes the medication as it enters the patient’s venous system. ¾ Peripheral IV methods: Chemotherapy and supportive care medications are administered in a variety of ways. Methods of administration include the following. Definitions. Administration of chemotherapy. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology As Needed Each Cycle Each Infusion Each IV Push Each Visit First Visit Requires Registered Nurse 19 X X X ¾ Using appropriate reference, check to ensure that the dosage falls Check for contraindications (e.g., abnormal laboratory results, serious side effects from previous treatments) before administration. X X X X The registered nurse must be knowledgeable regarding indications for therapy, side effects and potential adverse reactions, and appropriate X X X Complications of venous access are prevented or reduced with appropriate care. Chemotherapy and therapeutic agents are administered safely. within the prescribed safe range. dosage of the drug (e.g., milligrams ordered multiplied by the patient’s BSA). X X X ¾ Verify calculations performed by the physician, such as the drug X X X ¾ Check the physician order for the current date, days of administration for the therapy, patient allergies, and physician signature. X X Double-check the dose calculation for each chemotherapy agent prior to administering. Chemotherapy treatment plans or orders are clearly and concisely written and verified before administration. Many patients are sent home with chemotherapy delivered by a device that pumps drugs into their bodies 24 hours a day. The registered nurse in the office is on call for these patients in the event of pump problems, including dislodging a needle from the port, an alarm warning of occlusion (possibly related to blood that has congealed and formed a clot in the catheter), the accidental cutting of the tubing, or a dead battery. Problems can lead to rapid or inadequate infusion of the chemotherapy, infection, and/or the formation of a clot in the catheter or a blood vessel because of inadequate fluid flow. Epidural and intrathecal access devices: These catheters are inserted into the epidural space (between the bony prominences of the spinal column) and allow for the delivery of chemotherapy, opioids, and anesthetic medication for chronic intractable pain. Intraventricular (ommaya) access device: This is a dome-shaped, self-sealing silicone reservoir attached to a catheter. The device is implanted under the scalp above the frontal lobe and allows for delivery of chemotherapy into the cerebral spinal fluid to treat cancer cells present in that fluid. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology X X X X X X X X X X X X X X X X X X X X X X X X X X Hang primary IV fluids. This keeps the vein open, dilutes chemotherapy agents, and maintains IV access for therapeutic and potential emergency situations. Verify that the IV is functioning correctly: 20 Ensure the “five rights” of medication administration prior to administering any medication to prevent errors: ¾ Right patient. ¾ Right time. ¾ Right drug. ¾ Check for blood return. Some chemotherapy agents can damage the tissue surrounding the vein if leaks occur. Blood return is verified to confirm the IV line remains in a stable position in the vein. X X X X X X X X X X X Each Infusion ¾ Check the site for any signs of leakage into the skin. ¾ Prevent leakage of chemotherapy from the port septum. ¾ Use a noncoring needle for ports to minimize damage to the septum. Initiate CVAD access: ¾ Subsequent sites should be initiated above the previous IV site. X X X ¾ Routinely begin IV access in areas below the elbow. ¾ Assess for appropriate vein selection. Review prior sites of access and look for damage to previously used veins. Initiate peripheral IV access: X Requires Registered Nurse X First Visit ¾ Thoroughly cleanse skin at access site to reduce the potential for infection. X X Each Visit X X Each IV Push X X interventions. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology As Needed Each Cycle X X X X X X X X X X X X X X X X X X X X X X Begin the IV infusion: ¾ Compare the drug in IV bag with the physician order. ¾ Secure another registered nurse to double-check the dosage to be 21 ¾ ¾ ¾ ¾ order. ¾ Compare the drug in the syringe, bag, or bottle with the physician permeability fabric, chemotherapy gloves, a nonporous pad to place under IV, and goggles if the potential for eye contamination exists). ¾ Gather and use protective equipment (i.e., a gown made of low- Administer IV push agents: Infuse the bag of chemotherapy and adjust the rate of delivery as appropriate. Review the action of the drug and side effects with the patient. Explain the entire procedure to patient. Check the IV site to ensure that it is working correctly. delivered against physician order. permeability fabric, chemotherapy gloves, and goggles if the potential for eye contamination exists). ¾ Gather and use protective equipment (i.e., a gown made of low- X X X Double-check the patient’s identity. (Ask the patient to state his or her name, date of birth, address, or other identifier to prevent accidental delivery of medication to wrong patient.) X X X X X X X X X X X X X X X X X X X X X As Needed X X X First Visit X Each Visit Administer premedications (e.g., antiemetics and/or steroids to prevent nausea and vomiting). Requires Registered Nurse X X Each IV Push X X Each Infusion ¾ Right dose. ¾ Right route of administration. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Cycle First Visit X X X X X X Requires Registered Nurse X X X X X X X ¾ Secure another registered nurse to double-check the dosage to be ¾ ¾ ¾ ¾ ¾ Push the medication through a free-flowing IV while continuously When administering a vesicant agent, maintain specific precautions. 22 ¾ Check for blood return upon completion of infusion. ¾ Check patency of the CVAD per institution protocol. For CVAD access: X X X X X X ¾ Monitor the insertion site for signs of leakage or swelling (i.e., a small bump at the site). ¾ Check frequently for blood return or patency during IV push or continuous infusion without causing damage to fragile veins. Check every five minutes or 2–3 cc. ¾ Avoid use of an IV pump for peripheral infusions. X X X X X X ¾ Place a new peripheral IV (one stick) for vesicant agents. X X Each Infusion X X X X X X Each Cycle ¾ Evaluate risk factors for a peripheral extravasation (i.e., thin, fragile veins; sclerosed, hardened veins secondary to prior chemotherapy exposure). X X X X X X As Needed For peripheral IV access: monitoring the IV site for any signs of leakage. Place a nonporous pad under the IV site where the drug is being pushed to prevent exposure of chemotherapy to the patient. Review the action of the drug and side effects with the patient. Explain the entire procedure to the patient. Check the IV site to ensure that it is working correctly. Each Visit X Each IV Push delivered with the physician order. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 23 X X X X ¾ Flow of IV fluids. ¾ Vital signs (if indicated, dependent on drug administered). leakage. X X X X ¾ Patient response or tolerance to treatment. ¾ Condition of IV site and patency (redness, tenderness, pain, signs of X X X X X X X Individualize assessments based on patient history and condition and medication being administered. Periodic assessments include: X X X X Flush the peripheral IV catheter or CVAD between chemotherapy agents. This prevents chemical reactions or precipitate formation that might occlude the catheter. X X X Control the rate that the IV push agent is administered to avoid damage to organ systems. X X X X X X X X X Send patient for x-ray or dye study to confirm proper placement of device. Declot the access device with the prescribed medication per protocol. Reposition the patient. Flush the catheter with saline. ¾ If blood return is not evident prior to or during the infusion of a vesicant, Regulate and monitor the rate of infusion to ensure patient safety. The cancer and preexisting or comorbid conditions can be affected by the rate of delivery of fluids or chemotherapy (e.g., patients with preexisting kidney disease who receive large fluid volumes may retain rather than excrete the fluid). Requires Registered Nurse X First Visit X Each Visit Ask the patient to immediately report any stinging or burning at the site or internal discomfort (for CVAD infusions). Each IV Push X X X X Each Infusion X X X X Each Cycle X As Needed X Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology First Visit X X X X X X X X X X X Requires Registered Nurse X X X X X X X X X X X Manage implanted pumps or access devices (CVAD, arterial access device, intraventricular access device or ommaya reservoir, epidural and intrathecal access devices). This requires a registered nurse with advanced training in the care and management of these specialized treatment options. ¾ Monitor skin reactions around the pump site: signs of vesicant ¾ Check frequently for catheter blockage. ¾ Check and recheck the dosage of the drug in the reservoir to avoid ¾ Assess the stability of the pump’s placement (e.g., turning over in the Manage ambulatory pumps, if used. Flush IV access, both peripheral and central, at the end of the infusion, using sterile technique: ¾ When the infusion of chemotherapy is complete, flush the peripheral 24 ¾ Flush CVADS with heparin and normal saline to ensure and maintain ¾ Using sterile technique, disconnect the tubing and place a sterile cap ¾ Remove the peripheral IV catheter, apply pressure until bleeding is stopped, and apply sterile pressure dressing at the site. Assess for complications (e.g., continued bleeding after catheter removal). on end of CVAD. patency and function between intermittent administration. catheter needle before removal to wash out any chemotherapy that might remain. Chemotherapy agents should not be allowed to enter the tissue of the hand or arm when the needle is removed. pump pocket under the skin that would prohibit device access). over- or underdosing. Each Visit X X X X X X X X X X X X X X X X X X X X As Needed extravasation, drug crystallization, and skin death over pump site. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Cycle Each Infusion Each IV Push X X X X X X X X X X X X X X X X X X X X Potential or suspected extravasation: ¾ Assess continuously for vesicant or irritant extravasation. ¾ If appropriate, have antidote therapy (i.e., drugs given to counteract ¾ Assess the site to determine management of follow-up care (e.g., 25 ¾ Evaluate and manage potential long-term complications, including loss ¾ If extravasation is suspected, stop the infusion, administer the ¾ Stop the infusion. ¾ Disconnect the IV site. If extravasation occurs: antidote if one is available and appropriate, and apply ice or heat as appropriate (based on chemotherapy drug involved). of limb or loss of function. choice of future sites for IV infusion or placement of CVAD). potential tissue damage) readily available. administered at a later date, consider premedication. physician or protocol orders. treatment. Flare reaction (redness and itching at IV site): X X Requires Registered Nurse ¾ Once flare reaction has resolved, slowly resume infusion of the drug. ¾ Anticipation and/or prevention of future reactions: If the drug is to be First Visit X Each Visit X Each IV Push ¾ If reaction resolves, assess patient status and resume treatment per Each Infusion ¾ Assess for flare reaction. ¾ Implement appropriate management measures, including stopping Each Cycle X X X As Needed X X X Manage any reactions that occur during therapy. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 26 patient instructions, and any follow-up. Educate the patient and family on management of the extravasation site. Monitor the site at 24 hours, one week, two weeks, and as necessary. Initiate appropriate nursing interventions. Apply the antidote if available (not all drugs have antidotes). Apply hot or cold packs depending on the drug. Attempt to aspirate any residual chemotherapy agent. If using implanted port, verify needle placement. X X X X X X X X ¾ Consider medication desensitization. Actual reactions: ¾ Stop the infusion and initiate appropriate measures based on the ¾ Provide support to family. Perform a scratch test, intradermal skin test, or test dose before administering initial dose of drug. Instruct the patient on symptoms to report. Ensure availability of emergency equipment and medications. Obtain baseline vital signs. Identify drugs at risk for causing hypersensitivity reaction. X X X X X ¾ ¾ ¾ ¾ ¾ X X X X X Potential reactions: ¾ ¾ ¾ ¾ ¾ ¾ ¾ X Requires Registered Nurse X First Visit Hypersensitivity reaction (i.e., a reaction to a drug that can range from rash and itching to anaphylaxis, which is life-threatening shock). Each Visit X Each IV Push X Each Infusion ¾ Initiate a tracking form to document the condition of the IV site, Each Cycle X X X X X X X As Needed X X X X X X X Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 27 First Visit X X X X X X Reassess the infusion site for signs of extravasation. Monitor for bleeding post-infusion. X X X X Each Visit X X X X Each IV Push Monitor for adverse reactions and delayed and / or life-threatening anaphylactic shock. Monitor the patient after completion of chemotherapy. ¾ Administer appropriate medications based on physician order or protocol. ¾ Call 911 for emergency assistance. ¾ Start CPR. ¾ Administer oxygen. Initiate appropriate emergency measures and management of anaphylaxis. If anaphylaxis occurs, stop the infusion or administration of drug. Assess for anaphylactic reaction. Administer premedications. Obtain baseline vital signs. Identify drugs at risk for causing an anaphylactic reaction. Requires Registered Nurse ¾ ¾ ¾ ¾ ¾ ¾ Each Infusion X X X X X X X Each Cycle X X X X X X X As Needed Anaphylaxis (life-threatening shock): physician order or protocol. Section Two: Treatment The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 28 X X X ¾ Drug. X X X X Each IV Push X Tumor markers. Kidney (renal) function test. Liver function test. Complete blood count. X X Each Infusion Record on infusion flow sheets all updated information indicated below. This documents the actual treatment, method of administration, and date and time of administration. It serves as a historic and legal document of the patient’s treatment regimen. ¾ ¾ ¾ ¾ X X X X X X X X X X X X X X Each Cycle All laboratory values must be verified, evaluated, and trended so that changes can be monitored over the treatment continuum. X As Needed On laboratory flow sheets, document all updated laboratory results. Current laboratory results may determine a patient’s response to treatment. Variations in laboratory results could result in the delay of treatment, adjustments in drug dosages, or additional supportive care drugs to correct changes in laboratory values. Complete documentation on medical forms. X X X X X X X agents (e.g., sharps, biohazard waste bins). Occupational Safety and Health Administration compliance: ¾ Change linen. ¾ Remove reusable equipment after cleaning. ¾ Wipe down (clean) chairs, table, and other room supplies. X Requires Registered Nurse ¾ Dispose of all supplies used for the administration of chemotherapy First Visit X X Each Visit X X Clean treatment area and/or equipment. Section Three: Additional Clinical Responsibilities The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 29 BSA and/or AUC. Weight. Height. Pulse and respiratory rate. Temperature. Blood pressure. Document all oral and written instructions given to patients and family members; including how to manage side effects at home following treatment, how to monitor for delayed hypersensitivity reactions, and how to manage pain. The registered nurse must assess and document the patient’s and family members’ level of understanding of the instructions. ¾ ¾ ¾ ¾ ¾ ¾ Assess and document vital signs to determine baseline readings and to monitor changes in vital signs during and after treatment. Accurate height and weight measurements are essential for determining the patient’s BSA and must be documented. The dosages of the medications given to the patient are determined by the patient’s BSA, which the registered nurse must calculate and document based on height and weight. X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X Vesicant precautions (if appropriate). Patency of IV. Route of administration. X X X X X X X Start and stop times for each drug. X X ¾ ¾ ¾ ¾ X X X Each Visit irreversible side effects). Each IV Push X X Each Infusion X X X X Requires Registered Nurse X X X Each Cycle ¾ Dose. ¾ Solution or volumes. ¾ Cumulative dose (cannot be exceeded with risk of severe and As Needed First Visit Section Three: Additional Clinical Responsibilities The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Visit X X X X X X X X X X X Document all prescriptions given to the patient and the reason for prescriptions. This provides a record of all medications provided to the patient and is an important reference when following up with the patient by phone or on subsequent office visits. ¾ Nausea. ¾ Pain medication. ¾ Refills. Document notes of phone calls with the patient or family members, indicating what was discussed and which instructions or prescriptions were given. This provides a running record of all interactions with the patient and family members between office visits. ¾ Patient concern. X X X X X X X X X X X X X First Visit ¾ Tolerance to chemotherapy. ¾ Reactions. ¾ Side effects (e.g., nausea during treatment). X Each IV Push X Each Infusion X Each Cycle Assess and document the patient’s response to treatment, including tolerance of the treatment and any reaction or side effects experienced. This documentation is important historic information to have for subsequent treatments with the same therapy. Level of understanding. Pain management. Management of side effects of treatment. X X X X Requires Registered Nurse Delayed hypersensitivity. As Needed ¾ ¾ ¾ ¾ This documentation provides a running record of what the patient and family members have been taught. Section Three: Additional Clinical Responsibilities The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 30 Palliative and end-of-life care. Referrals and consultations as appropriate. Reporting of laboratory and test results. Symptom management. Cancer treatment options. 31 Implement nursing interventions. For example, when a patient has constipation from pain medication, the registered nurse offers suggestions to relieve symptoms such as drink a warm liquid, increase fluid intake, avoid constipating foods, etc. Recognize early complications of treatment. Educate the patient and family. Assess patient condition. ¾ ¾ ¾ ¾ ¾ Family questions and concerns. Medication changes. Change in patient health. Order verification. Interpretation of patient data. Potential problems that may be managed by phone: ¾ ¾ ¾ ¾ Phone calls: ¾ ¾ ¾ ¾ ¾ Provide or reinforce information about: Phone triage (patient- and family-initiated phone calls). Requires Registered Nurse X X X X X X X X First Visit X X X X X X Each Visit X X X X X Each IV Push X X X X X Each Infusion X X X X X X Each Cycle X X X X X X X X As Needed ¾ Physician instructions. ¾ Prescriptions. Section Three: Additional Clinical Responsibilities The Role of the Oncology Registered Nurse In Outpatient Medical Oncology 32 Other clinical responsibilities. ¾ Contact the pharmacy. ¾ Set up home care or hospice. ¾ Answer general questions from the patient and / or family. Shortness of breath. Constipation. Diarrhea. Bleeding and/or bruising. Fatigue. Vomiting. Mouth ulcers. Nausea. Chills. Fever. X X X X X X X X X X X X X X Requires Registered Nurse ¾ Prescription refill. ¾ New prescriptions. ¾ Symptom management (assess, educate, and intervene as necessary): Scheduling of chemotherapy appointments, physician visits, or tests (e.g., laboratory, x-ray). Laboratory results to patients. Laboratory results to other physicians. Insurance questions and concerns. X X X X X X X X X X X X X X X X X X X X As Needed ¾ ¾ ¾ ¾ Section Three: Additional Clinical Responsibilities The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Cycle Each Infusion Each IV Push Each Visit First Visit 33 X X X Monitor and assess patient status between clinic visits for signs and symptoms of infection. Manage sample drug inventory in compliance with state and federal regulations. X X Flush IV lines and venous access devices between therapy sessions (i.e. monthly port flush). X X X Provide CVAD dressing change. Manage indigent drug inventory in compliance with state/federal regulations, as appropriate. (Patients with financial problems may be eligible for pharmaceutical company-administered free drug programs.) X X X Assist with procedures (e.g., bone marrow aspiration; paracentesis, which is the removal of abnormal accumulation of fluid in the abdomen for evaluation of presence of cancer cells; thoracentesis, which is the removal of abnormal accumulation of fluid in the lung for evaluation of presence of cancer cells; lumbar puncture, which is the insertion of a needle into the spinal fluid for the purpose of removing fluid for testing or administration of chemotherapy). X X X Educate patients and families regarding clinical trials. Monitor patients receiving conscious sedation (administered during select procedures). X X Requires Registered Nurse Facilitate the submission process for clinical trials or research protocols. First Visit X Each Visit X Each IV Push Collaborate with the physician in screening patients for inclusion in available clinical trials or research protocols. Each Infusion X Each Cycle X As Needed Administer growth factors as prescribed. Section Three: Additional Clinical Responsibilities The Role of the Oncology Registered Nurse In Outpatient Medical Oncology First Visit Requires Registered Nurse 34 X X X X X X X X X ¾ Keep medication in original containers. Do not crush tablets or open ¾ Entire household needs to be instructed on how to handle bodily fluids capsules. room temperature, away from excess heat and moisture) to maintain the medication’s efficacy and prevent accidental ingestion (children or pets in the home). Also provide instructions regarding what to do or who to call if someone else accidentally takes the chemotherapy. ¾ Instruct patients in the proper storage of chemotherapy (refrigerator, to understand the importance of early recognition of and prompt intervention for potentially serious side effects.) Safety issues: X X X X ¾ Side effects and self-help measures to manage side effects. ¾ How and when to contact the clinic or oncology office (Patients need medication to make up for a missed dose, and the absolute importance of truth-telling when reporting the degree of accuracy in taking the chemotherapy as prescribed (Physicians make clinical judgments based on response to treatment. Dose adjustments may be made based on patients accurately reporting taking oral chemotherapy as prescribed.) laboratory tests and medical visits. Provide verbal and written instructions that include: X Each Visit X Each IV Push ¾ Special instructions, such as “take with food,” do not double up on Each Infusion ¾ Name of the medication (both generic and brand). ¾ Dose (may be taking different dose-sized tablets). ¾ Schedule of specific days the drug is to be taken as well as follow-up X Each Cycle X X X X As Needed X X X X Patient and family education. Section Four: Oral Chemotherapy The Role of the Oncology Registered Nurse In Outpatient Medical Oncology unexplained reasons or a history of self-adjusting doses of other medications. Implement necessary steps to assist the patient in achieving compliance. ¾ Assess the patient for a prior history of missed clinic visits for X X X X First Visit treatment. Older patients are more vulnerable to compliance problems because of visual and cognitive impairments, memory deficits, physical limitations, unpleasant side effects, and lack of social or family support. X X Each Visit ¾ Assess the patient for the ability to comply with this type of X Each Cycle Adherence and compliance: Requires Registered Nurse X X As Needed ¾ Proper disposal of unused oral chemotherapy. of person taking chemotherapy. Section Four: Oral Chemotherapy The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Each Infusion Each IV Push 35 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Section Five: Case Study The following case studies are presented to illustrate the actions of a competent registered nurse (RN) in addressing common situations that may arise. Extravasation of Adriamycin The RN is knowledgeable about the dangers associated with an extravasation. Extravasation of a vesicant can cause sloughing of skin, damage to tendons and/or ligaments requiring plastic surgery and possible extended therapy and reduced quality of life. Prompt intervention for actual or suspected extravasation can reduce or prevent skin damage. Even with all safety guidelines carefully in place and followed, chemotherapy emergencies can occur and it is imperative that a RN be present to provide appropriate oncology care. A 35-year-old Caucasian female received her third of four cycles of chemotherapy for a diagnosis of breast cancer. An IV was started in her hand and IV fluid initiated. The RN administered anti-nausea medications and prepared a bag of IV fluids to be used for the infusion. The RN assessed the IV site for patency by observing for swelling, pain, and blood return. The RN carefully and slowly administered Doxorubicin, a vesicant chemotherapy drug, using IV push technique. The vesicant was pushed by the RN 2-3ml at a time while a main IV line of normal saline solution ran continuously to dilute the drug and facilitate infusion. During the course of administering the drug, the RN continuously assessed the IV site for patency, checked for blood return, monitored for pain, burning, stinging, redness, or swelling. The patient reported no discomfort at IV site, no swelling was observed, and a blood return was noted while pushing the vesicant as described above. After 20 ml were delivered, the patient began to complain of some discomfort. Slight swelling at the IV site and no blood return were observed. The RN immediately stopped the infusion and attempted to aspirate drug from the IV catheter. The IV was removed. The physician was notified for further orders. The hand was elevated and an ice pack applied. The patient was given strict directions to follow while at home to reduce adverse side effects. In addition, the patient was instructed to call the physician or go to the emergency room if pain, swelling, redness increased or drainage occurred at the site. Due to the serious nature of the event, the RN would initiate a tracking tool which would allow her to track the site and mobility of the involved extremity/area. She would initiate a patient education form, which clearly defines when to call the physician and/or nurse. Finally, a medication variance report would be initiated to accurately reflect the event. This is an internal document which allows staff to review the chemotherapy process to prevent a possible re-occurrence. 36 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Oral Chemotherapy Mr. B. is a 72-year-old widower with a brain tumor. His treating physician has prescribed Temozolomide, an oral chemotherapy drug − a new therapy for his treatment. Mr. B. came to the office alone today, not expecting that a new treatment would be prescribed for him by his physician. Due to Mr. B.’s somewhat compromised thinking and memory ability as a result of his brain tumor, the RN set up an appointment for Mr. B. to return with his adult daughter for a chemotherapy teaching session before the Temozolomide was actually administered. Mr. B. and his daughter returned to the office two days later for the chemotherapy teaching session. The RN first assessed Mr. B. regarding his ability to comply with the very complicated schedule Temozolomide requires. The RN explained that multiple size tablets would be prescribed and that patients can become confused and harmed by taking the medication incorrectly. The RN requested that the daughter purchase a pillbox organizer. The daughter was taught the administration schedule (take the drug with water, on an empty stomach, at bedtime) and the specific scheduled days for taking the oral chemotherapy. The RN offered to assist the daughter in setting up the first round to assure accuracy. The RN provided written instructions regarding Mr. B.’s schedule, a written calendar that showed the specific days the medication was to be taken as well as the follow-up blood tests and physician visit. The RN provided education and written information on the drug Temozolomide that explained how to take the drug, how to store the drug, what food and other medications cannot be taken at the same time, what to do if a dose is missed, the possible side effects, self-help measures to cope with side effects and which side effects required an immediate call to the oncology physician’s office. The RN explained to the patient and daughter the absolute importance of reporting back to the physician/RN any missed doses or missed days, explaining that this is important information for the physician in order to make accurate judgments of how effective the drug is against the cancer and/or deciding on dose adjustments because of side effects. Lastly, the RN confirmed with the patient and daughter their understanding of the information provided, of who and when to call if there were problems or questions and explained that only one cycle of the Temozolomide will be prescribed at a time to lessen the chance of over dosage and to avoid missed follow-up appointments. The initial chemotherapy teaching session took approximately 60 minutes. 37 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Chemotherapy Administration Mrs. S is a 66-year-old white female diagnosed with lung cancer in December of 2004. A CT scan revealed that the tumor had invaded her pulmonary artery. Because of the tumor’s location on this critical vessel, surgery was not a viable treatment option. The surgeon explained that she could bleed to death on the operating room table if the artery could not be repaired following the removal of the tumor. Her physician has told her he would try to shrink the tumor with Cis-Platinum and VP16, two chemotherapy agents used frequently in the treatment of lung cancer. He also explained that he hoped to improve her ability to breathe if the burden (size) of the tumor was decreased. Today is the first day of her treatment cycle − chemotherapy agents are given for a predetermined time frame (i.e. a group of chemotherapy agents may be given for three days every 21 days). The patient’s response to treatment will be evaluated at the end of each cycle. Mrs. S and her daughter attended a chemotherapy teaching session yesterday that reviewed basic information related to chemotherapy drug administration. Upon arrival in the clinic, a peripheral IV is started. The RN explains to Mrs. S specific side effects related to the chemotherapy agents she is to receive. Cis-Platinum has the potential to damage the kidneys. To prevent damage to the kidneys, a liter of IV fluid is administered prior to the Cis-Platinum. Additionally, a diuretic (medication that will decrease fluid retention by increasing urinary output) is administered. The IV fluids and a diuretic are administered to prevent severe effects of the drug on the kidneys. After flushing the peripheral IV line with normal saline, an antiemetic agent and steroid are administered by IV push to prevent the severe nausea and vomiting associated with Cis-Platinum. The RN then puts on personal protective equipment to protect her/himself from contact with the chemotherapy agent. Personal protective equipment is worn during mixing of the chemotherapy agents in the pharmacy area, for starting and stopping the chemotherapy agent, and to manage any chemotherapy exposure. The Cis-Platinum is connected to the peripheral IV and administered. During the Cis-Platinum administration, Mrs. B becomes nauseated and starts vomiting. The RN nurse contacts the physician and obtains orders for an additional antiemetic agent and administers the treatment (this requires stopping the CisPlatinum infusion, flushing the IV with saline, administering the antiemetic, flushing again with saline, and restarting the Cis-Platinum). Upon completion of the CisPlatinum, a second liter of hydration fluid is given. This fluid is also given to prevent damage to the kidneys. Next, VP16 is administered. Mrs. S. is instructed that her blood pressure and pulse will be taken frequently during administration of the VP16 as this agent has the potential to cause hypotension (low blood pressure – which can result in cardiac complications). Mrs. S did not experience any changes in her blood pressure during the VP16 infusion. Upon completion of therapy, the peripheral IV is discontinued. 38 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Prior to leaving the clinic, the RN provides additional instructions to Mrs. S and her daughter. The information includes what to expect in the next few hours, side effects to report and who to call, and next treatment visit/appointment. This information is verbally reviewed and written instructions are provided. 39 The The Role Role of of the the Oncology Oncology Registered Registered Nurse Nurse In In Outpatient Outpatient Medical Medical Oncology Oncology Definitions Antiemetics: medications usually given with steroids and used to prevent the severe nausea and vomiting associated with many chemotherapy agents. Area under the curve (AUC): a formula used to calculate the dosage of a drug called Carboplatin. It is based on a complex formula utilizing a patient’s age, sex, weight, and the ability of the kidney to excrete waste product. Arterial access devices: implanted devices, resembling a port, but with a mechanism that delivers chemotherapy into the hepatic (liver) artery. Allows for the delivery of chemotherapy into a specific region of the body thus having a higher concentration of chemotherapy at the tumor site. Bisphosphonates: some tumors and / or cancer therapy can destroy bone mass causing serum calcium to be elevated. Elevated serum calcium can lead to confusion, seizures, and / or death. This group of drugs lowers blood calcium levels. Body surface area (BSA): a formula based on height and weight that is used in determining appropriate chemotherapy drug doses. Carcinogenic: the ability to cause cancer. Central venous access device (CVAD): intravenous device that is placed into large veins in the upper chest. Chemotherapy is very caustic to the veins. Repeated exposure to chemotherapy can sclerose (harden) veins making a peripheral IV difficult to insert. Veins also can become fragile from repeated exposure to chemotherapy. Fragile veins can easily be punctured in multiple places during insertion of the peripheral IV necessitating multiple attempts at placing a peripheral IV. A surgeon will place an implanted device (port) under the patient’s skin. A small tube that is threaded into the large vein in the chest cavity is then inserted. This device allows for the removal of blood for sampling or for the delivery of chemotherapy and other medications. Also, there are external catheters that are placed in the large vein in the chest cavity. These catheters are not fully implanted and are taped/held in place with a couple of stitches to the skin on the chest. Certified Biological Safety Cabinet: used to aseptically prepare drugs and prevent exposure of pharmacy/nursing staff to aerosolization of chemotherapy agents. Chemotherapy: treatment of a disease by means of chemical/biological substances or drugs. These agents work in a variety of ways including destroying rapidly dividing cells and affecting the biologic response of cells. In addition to cancer cells, chemotherapy may destroy many of the body’s other rapidly dividing cells. These include hair follicles, mucous membranes that line the gastrointestinal tract, sperm and female eggs, and blood components such as white blood cells, platelets and red blood cells. Co-morbidity: co-existing health problems such as cardiac history, history of heart attack, diabetes, emphysema, etc. 40 The The Role Role of of the the Oncology Oncology Registered Registered Nurse Nurse In In Outpatient Outpatient Medical Medical Oncology Oncology Cycle: chemotherapy agents are given for a predetermined time frame, for example, a group of chemotherapy agents may be given for three days every 21 days. The patient’s response to treatment is evaluated at the end of each cycle. Diuretic: medications that decrease fluid retention by increasing urinary output. Drug delivery device: catheter used to deliver therapy into a vein, an artery, the cerebrospinal fluid, or ventricular spaces in the brain. Epidural access devices: catheters that are inserted into the epidural space (spaces between the bony prominences of the spinal column), which allow for the delivery of opioids, anesthetic medication for chronic intractable pain, and chemotherapeutic agents. Extravasation: leakage of vesicant IV fluid into the skin. Fecal impaction: intestines blocked with stool. Flare reaction: redness and itching at IV site. Growth factors: drugs which stimulate the body’s bone marrow to make white blood cells that fight infection, red blood cells that prevent anemia, or platelets that assist in clotting. Hematologic: related to the blood. Implanted port: central venous access device that is totally implanted under the skin. A surgeon will place an implanted device (port – reservoir made of titanium with a self sealing material septum/top part of port) under the patient’s skin. A small tube that is threaded into the large vein in the chest cavity is then inserted. The port is accessed with a special needle which is attached to IV fluids that are then administered through the port/catheter into the vein Implanted pump: device implanted during a surgical procedure to deliver chemotherapy to a specific area, such as the liver via the hepatic artery. Chemotherapy is delivered over a period of weeks directly to the location of the cancer. Intraperitoneal administration: administration of chemotherapy or fluids into the peritoneal (abdominal) cavity. Intrathecal administration: administered via a catheter inserted into the patient’s cerebrospinal fluid. Intrathecal access devices: catheters that are inserted into the epidural space of the spinal column, which allow for the delivery of opioids, anesthetic medication for chronic intractable pain, and chemotherapy. Intravenous administration: administered through a catheter inserted into the patient’s vein. Intravenous piggy-back (IVPB): this technique involves hanging a bag of IV fluid, usually saline solution, and attaching (piggy-backing) the medication to be delivered into a side port of the tubing of the primary bag of fluid. This technique allows the 41 The The Role Role of of the the Oncology Oncology Registered Registered Nurse Nurse In In Outpatient Outpatient Medical Medical Oncology Oncology medication being administered to be further diluted as it is allowed to drip into the patient’s vein. Intravenous push (IV push, IVP): this technique is accomplished as the RN sits at the patient bedside and slowing pushes the medication into a side port of the primary bag’s IV tubing. The primary bag of fluid is allowed to drip while the nurse slowly pushes the syringe’s contents into the patient. Many drugs known as vesicants are required to be administered by this technique. Because the vesicant drug has the potential to cause severe damage, including tissue death, if any of the medication is allowed to leak into the tissues around the vein, the RN must constantly monitor the rate over which the drug is delivered and the site around the catheter placed in the patient’s vein to deliver the drugs. Intraventricular access device: device that is a dome shaped, self-sealing, silicone reservoir attached to a catheter that allows medication to enter ventricular spaces in the brain. It is implanted under the scalp above the frontal lobe. Allows for delivery of chemotherapy into the cerebral spinal fluid to treat cancer cells present in the fluid. See ommaya reservoir. Irritant: any agent that causes a local inflammatory reaction but does not cause tissue necrosis. Lumbar puncture: lumbar puncture, which is the insertion of a needle into the spinal fluid for the purpose of removing fluid for testing or administration of chemotherapy. Necrosis: tissue or muscle death that can lead to loss of use of an extremity or amputation of the extremity. Neurologic: issues related to the nervous system. Ommaya reservoir: device that is dome shaped, self-sealing, silicone reservoir attached to a catheter that allows medication to enter ventricular spaces in the brain. It is implanted under the scalp above the frontal lobe. Allows for delivery of chemotherapy into the cerebral spinal fluid to treat cancer cells present in the fluid. See intraventricular access device. Oral administration: by mouth in pill form. Paracentesis: removal of abnormal accumulation of fluid in the abdomen for evaluation of presence of cancer cells. Patency: IV is open, no clots or sluggish blood flow, easily infuses with good blood return. Peripheral venous access device (peripheral IV): intravenous device that is usually placed into veins of the hand or lower arm. Personal protective equipment: equipment (gloves, gowns, goggles – if indicated, mask – if indicated) worn by clinical staff to protect from exposure to chemotherapy. Platelet: type of blood cell that assists with clotting. 42 The The Role Role of of the the Oncology Oncology Registered Registered Nurse Nurse In In Outpatient Outpatient Medical Medical Oncology Oncology Premedicate: administering medications for control of symptoms/side effects prior to administration of chemotherapy agents. Pump: mechanical device used to regulate the rate of infusion of chemotherapy drugs. Red blood cells: carry hemoglobin, which in turn carries oxygen throughout the body. A lack of red blood cells results in a condition known as anemia. Research protocol: written document that includes specific details of a research project, including drug information, how to administer the drug, patient eligibility, etc. Steroids: given with antiemetics and used to prevent the severe nausea and vomiting associated with many chemotherapy agents. Supportive care medications: include antiemetics and steroids, growth factors, bisphosphonates, and pain medicines. See specific medication group for more information. Thoracentesis: removal of abnormal accumulation of fluid in the lung for evaluation of presence of cancer cells and reduce shortness of breath associated with presence of fluid. Topical administration: rubbed onto the skin. Tumor markers: some cancers have markers that indicate the reduction or progression of the cancer. Venous access device: see central venous access device and peripheral venous access device. Vesicant: some chemotherapy drugs have the potential to cause severe damage to tissue, tendons, or ligaments if it leaks into the area surrounding a vein. Damage may be so severe that it may require plastic surgery or amputation. White blood cells (neutrophils): these cells fight bacteria that can cause serious infections. A lack of sufficient neutrophils can result in impaired ability to fight off a serious infection which could lead to patient death. 43 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology References Aiken L, Clarke S, Sloan D. Hospital staffing, organization, and quality of care: cross national findings. Nursing Outlook, 50 (5), 187-194. 2002. American Nurses Association. American Nurses Association Nursing report for Acute Care Settings. Washington, DC: American Nurses Association. 1995. American Nurses Association. ANA Government Affairs Newsletter, 1, (1-4). 2001. American Nurse Association. Nursing-Sensitive Quality Indicators for CommunityBased Non-Acute Care Settings and ANA’s Safety & Quality Initiative. Washington, DC: American Nurses Association. 2002. Blegen M, Vaghan T. A multisite study of nurse staffing and patient outcomes. Nursing Economics, 16 (4), 196-203. 1998. Brant JM, Wickham RS (eds). ONS Statement on the Scope and Standards of Oncology Nursing Practice. Pittsburgh, PA: Oncology Nursing Press. 2004. Brown KA, Esper P, Kelleher LO, Brace O’Neill JE, Polovich M, White JM (eds). Chemotherapy and Biotherapy Guidelines and Recommendations for Practice. Pittsburgh, PA: Oncology Nursing Society. 2001. Buschell PC, Yarbro CH (eds). Oncology Nursing in the Ambulatory Setting. Boston, MA: Jones and Bartlett. 2005. Camp-Sorrell D (ed): Access Device Guidelines: Recommendations for Nursing Practice and Education (2nd ed). Pittsburgh, PA: Oncology Nursing Society. 2004. Carroll TL, Fay VP. Measuring the impact of advanced practice nursing on achieving cost-quality outcomes: Issues and challenges. Nursing Administration Quarterly, 2 (14), 32-40. 1997. Daly JM, Maas ML, Johnson M. Nursing outcomes classification. An essential element in data set for nursing and health care effectiveness. Computer Nursing, 15 (2 Suppl), S82-6. 1997. Devine EC. Meta-analysis of the effect of psycho-educational interventions on pain in adults with cancer. Oncology Nursing Forum, 30 (1), 75-89. 2003. Devine EC, Westlake SK. The effects of psycho-educational care provided to adults with cancer: Meta-analysis of 116 studies. Oncology Nursing Forum, 22 (9), 1369-81. 1995. 44 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Donabedian A. The Definition of Quality and Approaches to Its Assessment. Chicago, IL: Health Administration Press. 1980. Doran D. State of the Science. Sudbury, MA: Jones and Bartlett. 2003. Elwood P. Shattuck lecture: Outcomes management – A technology of patient experience. New England Journal of Medicine, 318 (23), 1549-56. 1988. Epstein AM. The outcomes movement-will it get us where we want to go? New England Journal of Medicine, 323 (4), 266-70. 1990. Gullatte MM. Clinical Guide to Antineoplastic Therapy: A Chemotherapy Handbook. Pittsburgh, PA: Oncology Nursing Press. 2001. Hickey M, Newton S (eds). Telephone Triage for Oncology Nurses. Pittsburgh, PA: Oncology Nursing Society. 2005. Institute of Medicine. Medicare: A strategy for quality assurance sources and methods. Washington, DC: National Academy Press. 1990. Institute of Medicine and National Research Council. Enhancing quality cancer care (National Cancer Policy Board), M. Hewitt and J Simone (eds). Washington, DC: National Academy Press. 1999a. Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press. 1999b. Institute of Medicine. To err is human: building a safer health care system. Washington, DC: National Academy Press. 1999c. Institute of Medicine. Health professions education: a bridge to quality. Washington, DC: National Academy Press. 2003. Intravenous Nursing Society. Infusion Nursing Standards of Practice. Journal of Intravenous Nursing, 23(65). November/December 2000. Irvine D, Sidani S, Hall L. Finding value in nursing care: a framework for quality improvement and clinical evaluation. Nursing Economics, 16 (3), 110-116. 1998. Jennings B. Outcomes: Two directions-research and management. AACN Clinical Issues, 6 (1), 79-88. 1995 Jennings B, Staggers N, Brosch L. A classification scheme for outcome indicators. Image: Journal of Nursing Scholarship, 31 (4), 381-388. 1999. 45 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Johnson M, Maas M. Implementing the Nursing Outcomes Classification in a practice setting. Outcomes Management for Nursing Practice, 2 (3): 99-104. 1998. Johnson M, Maas M, Moorhead S. Nursing Outcome Classification (2nd ed). St. Louis, MO: Mosby. 2000. Kovner C, Jones C, Zhan C, Gergen PJ, Basu J. Nurse staffing and postsurgical adverse events: An analysis of administrative data from a sample of U.S. hospitals, 1990-1996. Health Services Research, 37 (3), 611-29. 2002. Lang N, Marek K. The classification of patient outcomes. Journal of Professional Nursing, 6, 158-163. 1990. Lipscomb J, Donaldson M. Outcomes research at the NCI: Measuring, understanding, and improving the outcomes of cancer care. Clinical Therapeutics, 25 (2), 699-712. 2003. Lipscomb J, Donaldson M, Arora N, et al. Cancer outcomes research and the arenas of application. JNCI Monographs, 33, 178-197. 2004. Maas M, Delaney C. Nursing process outcome linkage research: Issues, current status, and health policy implications. Medical Care, 42 (2), 40-48. 2004. Maas M, Johnson M. Moorehead S. Classifying nurse sensitive patient outcomes. Image Journal Nursing Sch, 28 (4), 295-301. 1996. Maas M, Reed D, Park M, Specht J, Schutte D, et al. Outcomes of family involvement in care intervention for caregivers of individuals with dementia. Nursing Research, 53 (2), 76-86. 2004. Mitchell P, Lang N. Framing the problem of measuring and improving healthcare quality. Medical Care, 42 (2), II-4-II-11. 2004. National Quality Forum. Safe Practices for Better Healthcare. 2003. National Quality Forum: NFQ Steering Committee meeting. Standardizing Quality Measures for Cancer Care Summary Report: Final Summary. September 4-5, 2000. Naylor M, McCauley K. The effects of a discharge planning and home follow-up intervention on elders. Journal of Cardiovascular Nursing, 14 (1), 44-54. 1999. Naylor M, Brooten D, Campbell R, Maislin G, McCauley K, Schwartz J. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatric Society, 52 (5), 675-684. 2004. 46 The Role of the Oncology Registered Nurse In Outpatient Medical Oncology Occupational Safety and Health Administration (OSHA): OSHA Technical Manual. http://www.osha.gov/dts/osta/otm/otm_toc.htm. Oncology Nursing Society. Oral Chemotherapy Considerations for Oncology Nursing Practice. Clinical Journal of Oncology Nursing, 7 (6, Suppl). 2003. Oncology Nursing Society. Sentinel Events Toolkit. 2002. Patrick DL, Chiang Y. Measurement of health outcomes in treatment effectiveness evaluations: Conceptual and methodological challenges. Medical Care, 38(9), II-14-II25. 2000. Urden L. Outcome evaluation: An essential component for CNS practice. Clinical Specialist, 13 (1), 39-46. 1999 47




















































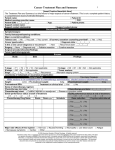

![[Insert Practice Name/Info Here]](http://s1.studyres.com/store/data/003627257_1-f993e13f3647f1666582d75e79d0541e-150x150.png)