* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Valsartan + Captopril - Duke Clinical Research Institute
Survey
Document related concepts
Transcript
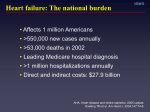
VALsartan In Acute myocardial iNfarcTion Marc A. Pfeffer, MD, PhD (Chair), John J.V. McMurray, MD (Co-Chair), Eric J. Velazquez, MD, Jean-Lucien Rouleau, MD, Lars Køber, MD, Aldo P. Maggioni, MD, Scott D. Solomon, MD, Karl Swedberg, MD, PhD, Frans Van de Werf, MD, PhD, Harvey D. White, DSc, Jeffrey D. Leimberger, PhD, Marc Henis, MD, Susan Edwards, MS, Steven Zelenkofske, DO, Mary Ann Sellers, MSN, and Robert M. Califf, MD, for the VALIANT Investigators Other Steering Committee Members: P. Armstrong, P. Aylward, S. Barvik, Y. Belenkov, A. Dalby, R. Diaz, H. Drexler, G. Ertl, G. Francis, J. Hampton, A. Harsanyi, J. Kvasnicka, V. Mareev, J. Marin-Neto, J. Murin, M. Myers, R. Nordlander, G. Opolski, J. Soler-Soler, J. Spac, T. Stefenelli, D. Sugrue, W. Van Gilst, S. Varshavsky, D. Weaver, F. Zannad. Dr. Pfeffer is named as a coinventor on a patent awarded to the Brigham and Women’s Hospital regarding the use of inhibitors of the renin-angiotensin system in selected survivors of myocardial infarction; there is a licensing agreement between Novartis Pharmaceuticals and the Brigham and Women’s Hospital, which is not linked to sales. Supported by a grant from Novartis Pharmaceuticals Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Aims VALIANT was designed as a mortality trial in high-risk MI patients who derived particular benefits from an ACE inhibitor (SAVE, AIRE, TRACE). To determine whether: u the ARB valsartan was superior to captopril in improving survival and with equal statistical power u the addition of the ARB valsartan to captopril was superior to the proven dose of captopril in improving survival u If valsartan was not superior to captopril, a non-inferiority analysis was prespecified to determine whether valsartan could be considered “as effective as” captopril Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Acute MI (0.5–10 days)—SAVE, AIRE or TRACE eligible (either clinical/radiologic signs of HF or LV systolic dysfunction) Major Exclusion Criteria: — BP < 100 mm Hg — Serum creatinine > 2.5 mg/dL — Prior intolerance of an ARB or ACE-I — Nonconsent double-blind active-controlled Captopril 50 mg tid (n = 4909) Valsartan 160 mg bid (n = 4909) Captopril 50 mg tid + Valsartan 80 mg bid (n = 4885) median duration: 24.7 months event-driven Primary Endpoint: All-Cause Mortality Secondary Endpoints: CV Death, MI, or HF Other Endpoints: Safety and Tolerability Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Enrollment and Follow-up 14,808 Patients Randomized Informed consent not ensured: 105 patients 14,703 Patients Captopril Valsartan Combination 4909 4909 4885 Vital status unknown: 38 (0.8%) 4871 (99.2%) Vital status unknown: 53 (1.1%) 4856 (98.9%) Vital status unknown: 48 (1.0%) 4837 (99.0%) Median follow-up: 24.7 months Vital status ascertained in 14,564 patients (99.05%) Vital status not ascertained in 139 patients (0.95%) (lost to follow-up at 1 year: 0.4%; 2 years: 0.7%) Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Baseline Characteristics Mean age (years) 64.8 Thrombolytic therapy (%) 35.2 Women (%) 31.1 Primary PCI (%) 14.8 Other PCI after MI, before randomization (%) 19.8 Qualifying MI site (%) Anterior Inferior 59.4 34.4 Qualifying MI type (%) Q wave Non Q wave 66.6 31.9 Mean BP (mm Hg) Killip class (%) Mean LVEF* (%) Creatinine Days to randomization 123/72 I II III IV 28.0 48.3 17.3 6.4 35.3 1.1 mg/dL 98 µmol/L 4.9 *data on LVEF were available for 11,338 patients Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Baseline Characteristics Medical History (%): Baseline Medications (%): Diabetes mellitus 23.1 ACE inhibitor* Hypertension 55.2 ARB* Smoking 31.7 Beta-blocker 70.4 Aspirin 91.3 Other antiplatelet 24.8 Potassium-sparing diuretic 9.0 Prior: Myocardial infarction 27.9 Heart failure 14.8 Stroke 6.1 CABG 7.0 PCI 7.3 39.6 1.2 Other diuretic 50.3 Statin 34.1 *stopped before randomization Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Study Drug Dose Titration Step I Step II Step III Step IV Cap 50 mg (tid) Cap 25 mg CAPTOPRIL (tid) Cap 6.25 mg Cap 12.5 mg Val 160 mg (bid) Val 80 mg Val 40 mg VALSARTAN (bid) Val 20 mg COMBINATION Cap 12.5 mg Cap 6.25 mg Val 20 mg Val 20 mg Cap 25 mg Val 40 mg Cap 50 mg (tid) Val 80 mg (bid) GOAL by 3 months Am Heart J. 2000;140:727–734 Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Mortality by Treatment 0.3 Captopril Valsartan Probability of Event 0.25 Valsartan + Captopril 0.2 0.15 0.1 0.05 Valsartan vs. Captopril: HR = 1.00; P = 0.982 Valsartan + Captopril vs. Captopril: HR = 0.98; P = 0.726 0 Months 0 Captopril 4909 Valsartan 4909 Valsartan + Cap 4885 6 12 18 24 30 36 4428 4464 4414 4241 4272 4265 4018 4007 3994 2635 2648 2648 1432 1437 1435 364 357 382 N Engl J Med 2003;349:1893-1905 Copyright © 2003 Duke Clinical Research Institute. All rights reserved. All-Cause Mortality: Noninferiority Analyses Hazard Ratio (97.5% CI) P-value noninferiority margin (noninferiority) Intention-to-Treat Patient Population (n = 14,703) 0.004 Per Protocol Patient Population (n = 14,285) 0.002 Noninferiority not Demonstrated Noninferiority Val Superior to Cap 0.8 Cap Superior to Val 1 1.13 1.2 Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Mortality in SAVE, TRACE, AIRE, and VALIANT Hazard Ratio for Mortality SAVE TRACE Valsartan preserves 99.6% of mortality benefit of captopril AIRE Combined VALIANT (imputed placebo) 0.5 Favors Active Drug 1 Favors Placebo 2 Pfeffer, McMurray, Velazquez, et al. NInstitute. Engl J Med 2003;349 N Engl J Med 2003;349:1893-1905 Copyright © 2003 Duke Clinical Research All rights reserved. CV Death, MI, or HF by Treatment 0.4 Captopril Valsartan Probability of Event Valsartan + Captopril 0.3 0.2 0.1 Valsartan vs. Captopril: HR = 0.96; P = 0.198 Valsartan + Captopril vs. Captopril: HR = 0.97; P = 0.369 0 Months 0 6 12 18 24 30 36 Pfeffer, McMurray, Velazquez, et al. NInstitute. Engl J Med 2003;349 N Engl J Med 2003;349:1893-1905 Copyright © 2003 Duke Clinical Research All rights reserved. Cardiovascular Mortality and Morbidity Hazard Ratio (97.5% CI) P-value noninferiority margin (noninferiority) CV Death 0.001 (1657 events) CV Death or MI 0.00001 (2234 events) 0.0001 CV Death or HF (2661 events) CV Death, MI, or HF 0.000001 (3096 events) Noninferiority not Demonstrated Noninferiority Val Superior to Cap 0.8 Cap Superior to Val 1 1.13 1.2 Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Adverse Experience Leading to Dose Reduction Captopril 20 % of Patients 15 Valsartan † Valsartan + Captopril * P < 0.05 Valsartan vs. Captopril †P * < 0.05 Valsartan + Captopril vs. Captopril 10 * 5 † * 0 n= * Hypotension Renal Causes Hyperkalemia Cough Skin Rash 2205 619 162 555 146 * Taste AngioDisturbance edema 82 56 Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Adverse Experience Leading to Study Drug Discontinuation Captopril 3.5 Valsartan Valsartan + Captopril * P < 0.05 Valsartan vs. Captopril % of Patients 3 †P < 0.05 Valsartan + Captopril vs. Captopril 2.5 † 2 1.5 * † 1 * * 0.5 * 0 n= Hypotension 201 Renal Causes 154 Hyperkalemia 23 Cough 253 Skin Rash 90 Taste AngioDisturbance edema 46 34 Copyright © 2003 Duke Clinical Research Institute. All rights reserved. Conclusion In patients with MI complicated by heart failure, left ventricular dysfunction or both: u Valsartan is as effective as a proven dose of captopril in reducing the risk of: —Death —CV death or nonfatal MI or heart failure admission u Combining valsartan with a proven dose of captopril produced no further reduction in mortality—and more adverse drug events. Implications: In these patients, valsartan is a clinically effective alternative to an ACE inhibitor. Copyright © 2003 Duke Clinical Research Institute. All rights reserved.