* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Joint Commission Questions and Answers
Survey
Document related concepts
Transcript
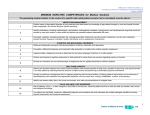
Joint Commission 2013 Questions and Answers A pocket guide to making quality, safety and preparedness a permanent part of your job &A Index Important Phone Numbers...................................................................3 About This Guidebook......................................................................... 4 You and the Survey Process.................................................................5 The AAMC Mission Statement.............................................................. 9 National Patient Safety Goals............................................................. 11 Ethics, Rights and Responsibilities.....................................................16 Provision of Care, Treatment and Services.......................................... 24 Assessment (nutrition, pain, abuse/neglect)—POCT—Restraints —Learning Assessment—Patient Education—Handoff/SBAR— Continuum of Care—Blood Administration—Falls— Code Blue/Rapid Response—Code Carts 1 Medication Management...................................................................53 Surgical Services...............................................................................59 Surveillance, Prevention, and Control of Infection...............................67 Improving Organizational Performance...............................................78 Management of the Environment of Care............................................85 Radiation Safety................................................................................92 Emergency Management....................................................................93 Leadership........................................................................................95 Information Management...................................................................97 Human Resources............................................................................. 99 2 Important Phone Numbers • The hospital emergency number to contact security officers (i.e. fire) is x6911 • In the Sajak Pavilion, Wayson Pavilion, or Health Sciences Pavilion, dial 9-1-1 for police or fire emergency • Patient Safety/Incident Report Hotline x4787 (“4PTS”). • Compliance Officer, Shirley Knelly, x1328/ Compliance Hotline x1338 • Privacy Officer, Robin Smith, x4130 • Patient Safety Officer, Shirley Knelly, x1332 • Environment of Care Safety Officer, Tony Kuzawinski, x4798 • Emergency Repair Hotline at x4777 3 About This Guidebook While this guidebook is meant to prepare you for a Joint Commission survey, its larger purpose is to make that level of preparation a permanent presence in the way you go about your job–every day, every time. You are responsible for being familiar with the information in the guidebook, which means you share in the responsibility for making sure that quality, safety and preparedness are not the exception but the constant rule. Check with your director/manager about your specific responsibilities in preparing for the survey, and about what specific information will assist you in responding to surveyors’ questions during the survey process. 4 You and the Survey Process 1.What is the Joint Commission? The Joint Commission is an accrediting organization that evaluates a health care organization’s performance in areas that most affect patient health and safety. These areas are defined in The Joint Commission Standards. By achieving accreditation, a health care organization has demonstrated its commitment to provide safe, quality care to its patients. 2.What is your role during the survey? All employees should know that a surveyor must first be identified by administration as a bona fide surveyor before any hospital business is discussed. If you are the first contact a surveyor has made, smile, introduce yourself, including your title, and accompany the surveyor to your area manager to contact the Vice President of Quality and Patient Safety. 5 3.What is Tracer Methodology? Tracer methodology is an evaluation method in which a surveyor selects a patient and uses that individual’s record as a roadmap to assess and evaluate an organization’s compliance with selected standards and the organization’s system for providing care and services. 4.What is the role of the staff in the survey/during a tracer? As surveyors move around the hospital, they will ask to speak with the staff members who have been involved in the tracer patient’s care, treatment and services. Assume they will want to talk with you, so have confidence in yourself–you provide awesome care, so let them see it! Remember that you are prepared to answer their questions. 6 Consider the following recommendations: > Answer their questions directly (keep your answers short and sweet) and ask the surveyor to repeat or rephrase the question if you don’t understand it. > Be polite and smile–do not let the questions make you feel defensive or angry. > Be honest–if you do not know the answer, do not make one up. If you don’t know, state your resources. > Be specific, provide examples for an answer and refer to policies or procedures whenever possible. > Be enthusiastic about what you do. 7 Examples of what will be asked: >Your role in patient safety (i.e., NPSGs) >What makes you competent in your role and how you were oriented in that role (i.e., licensure, yearly competencies) > How care is coordinated and communicated with other disciplines (i.e. care planning) >What you would do in an emergency (i.e. fire) > How do you support patient rights >What are your Performance Improvement Projects on your unit >What is a Sentinel Event/Near Miss 8 The Anne Arundel Medical Center Mission Statement It is important that all employees know, understand and can speak about the mission of the hospital. The mission of Anne Arundel Medical Center is to enhance the health of the people we serve. AAMC enhances the health of the people we serve by recognizing its responsibilities for following the highest standards of care, treatment and services in meeting the needs of individual patients, affiliated physicians, third party payers, subcontractors, independent contractors, vendors, consultants, our community, and one another. 9 1. How do you support the mission of AAMC? Anne Arundel Medical Center staff provides patient care in a manner consistent with the mission statement. 2. Do you know what is meant by one level of care? Yes. The care we provide is the same for all patients throughout the hospital who have similar needs. We assure that all patients receive the same level of care when we use common policies/procedures and collaborate with other departments in the provision of care. Outcomes then can be assessed and measured through performance improvement activities. 10 National Patient Safety Goals Each year the Joint Commission identifies National Patient Safety Goals and surveys organizations’ efforts to achieve these goals, as appropriate to their settings and services. Each employee is expected to know how these safety goals are being applied in their particular area of service. Please refer to the National Patient Safety Goals flipcharts and/or posters in your departments for details. The current National Patient Safety Goals are on the following pages: 11 GOAL 1:Improve the accuracy of patient identification > Double identification of patient: >> Name and contact serial number (CSN) > Two person verification process for the administration of blood and blood products GOAL 2: Improve the effectiveness of communication among caregivers Critical value results reporting process GOAL 3: Improve medication safety 12 > Labeling of meds > Management of anticoagulation therapy > Accurately and completely reconcile medications across the continuum of care GOAL 7: Reduce the risk of healthcare associated infections > Comply with CDC or WHO hand hygiene guidelines and compliance monitoring > Implementation of evidence based practices to prevent: >>Health care associated infections due to multi-drug resistant organisms (MDRO) and Cdiff flagging and isolation, patient and health care worker education. >>Central Line Associated Bloodstream Infections (CLABSI): central line insertion checklist, patient education prior to insertion. >>Surgical Site Infections (SSI): proper antibiotic prophylaxis, patient education prior to surgery. >>Catheter Associated Urinary Tract Infections (CAUTI): limit Foley use, leg securement. 13 GOAL 15:Identify safety risks inherent in its patient population > Identify patients at risk for suicide >Provide suicide information (i.e., crisis hotline) to the patient and family members Universal Protocol to prevent wrong site, wrong procedure 14 > Pre-procedure verification process > Mark procedure site > Perform a time-out just prior to the procedure What are the responsibilities of the Patient Safety committee? >>Integration and coordination of all components of the Patient Safety Program. >>Oversight and implementation and monitoring of the National Patient Safety Goals. >>Reviewing and recommending actions related to patterns/trends identified in occurrences reports. >>Promoting a non-punitive culture of safety. 15 Ethics, Rights and Responsibilities The hospital has an ethical responsibility to the patients and community it serves. To fulfill this responsibility, ethical care, treatment, services and business practices must go hand-in-hand. The hospital’s system of ethics supports honest and appropriate interactions with patients. The system of ethics also includes patients whenever possible in decisions about their care, treatment, and services, including ethical issues. Refer to policy ERR3.1.03 1. What is an ethics consult and how do you initiate it? A patient, family member, physician, caregiver, other party or an employee may request an Ethics Consult. An ethic consult can be initiated through a clinical consultation in Epic or can be initiated through the hospital operator. This consult accesses an ethics representative who is on call 24 hours a day, seven days a week. The on-call person will ensure all supports 16 are in place to facilitate the decision making at hand, this may include ensuring family conferences have taken place to convening a patient care advisory committee to provide clarification or assistance in facilitating care decisions as needed. A Patient Care Advisory Committee must include an administrator, a physician, a social worker and a nurse that are uninvolved in the care of the patient or issue in order to give an objective view and facilitation. Refer to policies ERR3.1.10/ERR3.1.09 2. How are patients informed of their rights? Patients are given an Advance Directive pamphlet, Patient Guide and brochures during the admitting process. Information is also located in patient rooms. Volunteers visit with new patients and provide additional information if needed. Interpreters are available to assist when needed. Refer to policy ERR3.1.03 17 3. What is an Advanced Directive? An Advance Directive is either a living will or a durable power of attorney for health care. It allows patients to indicate their wish for health care in case they become involved in an end of life situation or are unable to speak for themselves. Refer to policy ERR3.1.02 4. What is the hospital policy on ‘Do Not Resuscitate’ orders? It is the policy of AAMC to honor the wishes of patients and their families who express a desire to withhold or withdraw life-sustaining treatment when specific criteria can be met. Refer to policy ERR3.1.08 5. How does a patient, family member or visitor initiate a complaint? Any patient, family member, visitor, or nurse/caregiver can initiate a complaint to any hospital employee. Hospital employees should do as much 18 as they can for the patient at the time. Access Patient Advocacy at x4820. During off shifts, the administrative coordinator or clatanoff pavilion administrative coordinator would handle such issues. Refer to policy ERR3.1.04 6. How do you ensure patient privacy? >Only access a patient’s medical record when you have a “need to know,” for example, you are involved in the direct treatment, payment, or other healthcare operations related to that specific patient. >Never discuss patients in public areas (i.e. elevators, cafeteria). >Maintain confidentiality of patient information when talking on the telephone or at the computer. >Sign off the computer when finished. 19 patient privacy cont. >Maintain security of the patient’s physical medical record >Knock before entering the patient’s room >Be sure a patient’s body is adequately covered Refer to policy ERR3.1.05 7. How would you address the care and learning needs of patients with religious, cultural or language barriers? 20 >Consult with Patient Advocacy, Social Services and Spiritual Care >Involve hospital in-person Spanish interpreters for all language barriers, including hearing and sight impairments, and they will facilitate support and interpretation for you through the Martti units or Pacific Interpretation audio interpretation services. >For hearing and/or sight impaired patients, refer to policy ERR3.1.01 >A patient’s learning needs are assessed with each hospitalization by all professionals who interact with the patient, the information is documented in patient education tab assessment. 8. Why must we document a patient’s primary language and where do we document this information? Language barriers can have a significant impact on safe patient care and patient care outcomes. As the diversity of our region continues to grow, Anne Arundel Medical Center is encountering more patients with language barriers. To communicate effectively with our patients, we must provide patient care that is linguistically appropriate to all patients. The first step in providing this care is to identify and to document the patient’s primary language. 21 >The following are the steps to document on the Adult Profile Flow Sheet: >>Language Assistance–Answer ‘Yes’ or ‘No’ >>Language Needed–Open pull down menu and select language >>Order an interpreter consult (x3801) 9. What are the components of an Informed Consent? The goal of the informed consent process is to establish a mutual understanding and agreement between the patient or surrogate and the individual who provides the care or procedure that the patient received. The process allows each patient or surrogate to fully participate in decisions about his/her care, treatment and services. Obtaining consent to treatment ensures that any patient receiving surgery or medical procedures will be fully informed by the “individual performing the procedure” as to all the material risk, benefits and alternatives prior to giving consent. 22 The consent form, Record of Consent for Procedure is required for all surgical procedures and certain categories of invasive and a several types of noninvasive procedures, such as radiological procedures, administration of blood/ blood products, refusal of blood transfusions, radiation therapy. A properly executed informed consent contains documentation by the individual performing the procedure of the patient’s understanding of the information pertaining to the nature of the proposed care, treatment, services, medications, interventions or procedures, material risks, benefits and side effects of the proposed care, therapy or procedures. It also contains documentation of the likelihood of achieving care goals, the reasonable alternatives to the proposed care or procedure, the material risk, benefits and side effects related to alternatives, including the possible results of not receiving care, treatment and services, and whether other healthcare professionals will be performing tasks related to the proposed care or procedures. 23 Provision of Care, Treatment and Services The provision of care, treatment, and services to patients is composed of four core processes or elements: • Assessing patient needs. • Planning care, treatment, and services. • Providing the care, treatment, and services the patient needs. • Coordinating care, treatment, and services. 1. Who can make a referral to Nutrition Services? Any direct caregiver for the patient may request a nutrition consult. Nutritional needs are initially assessed within the first 24 hours as part of the admission screening. 24 2. When and how often is pain assessment done? Pain assessments are done by a professional nurse on admission, after each intervention and as-needed, at least once per shift. Interventions are made based on the reassessment and in evaluation of the pain management. Patients are assessed for their risk of pain upon entering AAMC by a professional nurse. Factors that increase a patient’s “risk for pain” include being developmentally or medically non-verbal, English is not the patient’s primary language, extremes of age, cultural and religious beliefs. If pain is present upon entering AAMC, a comprehensive pain assessment is completed. See NAP12.1.18 for components of a comprehensive pain assessment. Pain is subsequently assessed every shift, each report of pain, within one hour of administering a PRN opioid, any new or changed pain; prior to and following a procedure, per PCA policy and at discharge. 25 3. How is pain assessed and managed for our patients? Pain management goals are set with the patient and family. All professionals who interact with the patient assess pain. Interventions are initiated as appropriate through an interdisciplinary process. Pain is assessed using developmental/age and cognitively appropriate pain assessment tools. ** Know which pain assessment tools available in Alec are appropriate for your patient ** Pain management is included in the patient’s individualized plan of care and supported by Clinical Practice Guidelines (CPG’s) that address both acute and chronic pain. AAMC provides multi-modal and interdisciplinary pain management. 26 4. Who would you notify if you suspect abuse and/or neglect of a patient? Notify the supervisor/designee and the social worker. There is also a domestic violence coordinator at x1209 who can assist. A consult can also be entered into Alec based on the admission screenings. 5. What are some specific reportable criteria for suspected abuse of a patient? • Physical signs: cigarette burns, scalding burns, certain types of fractures or internal injuries • Personality: overly shy or aggressive, cries easily • Coping skills: inappropriate low tolerance, expresses desire to die • Personal appearance: unkempt, poor hygiene, malnourished 27 6. What is Point of Care Testing (POCT)? Point of Care tests are laboratory tests done outside of the lab by non-lab personnel. Because an accredited laboratory has many quality controls built into its processes, as well as highly trained lab personnel, any lab tests done outside the walls of the lab must be done with the same level of quality control. 7. What POCT is performed in your patient care area? 28 Each patient care area at AAMC has defined POCT. In order to know what POCT is authorized (permitted) in your area, refer to the POCT grid under Lab Administration on the intranet. All POCT performed at AAMC is for screening purposes and should not be used as a sole source of patient diagnosis. 8. What is the organization’s policy on restraints? AAMC’s philosophy is to strive toward a restraint free-environment by continuously improving our practice to protect patients and respect their right and dignity. 9. How do you monitor use of restraints? AAMC is committed to preserving a patient’s rights and dignity. AAMC utilizes retrospective chart review to monitor use of restraints to identify opportunities to introduce preventive strategies, alternative use, and process improvements that reduce the risk associated with use of restraints on an ongoing basis. 29 10. What are the two types of restraints that are used at AAMC? Medical-Surgical: Used to promote medical-surgical healing. These restraints are used for patients climbing out of bed or pulling at tubes or lines. Behavioral Restraints: Used in an emergency to protect the patient against injury to self or others because of violent or abhorrent behavior. 11. What procedures are required for each type of restraint? The revised Restraint Policy and the Physician Order Sets list all the requirements for each type of restraint. 30 Key Medical/Surgical Restraint Requirements: >A physician order within 12 hours of application. >When a verbal order is given to restrain, the physician must evaluate the patient within 24 hours. >Physician must renew the order, based on reevaluation, at least every calendar day >Care and assessment every two hours Key Behavioral Restraint Requirements: >A physician order and face-to-face assessment within one hour of application >The care and assessment is done every 15 minutes >A time-limited order based upon age (four hours for adults, two hours for ages 9 to 17, one hour for under age nine). 31 12. Do you utilize seclusion (the involuntary confinement of a person in a locked room) at AAMC? No, we do not use seclusion at AAMC. 13. How do we determine the educational needs of patients, families and significant others? Patient, family and significant others’ learning needs are assessed on admission and then reassessed on an ongoing basis. This information is documented in the patient education tab. The answers to the learning assessment questions can be viewed in the SBAR handoff report. 32 14. What are considerations in a learning assessment? >Literacy, educational level and language >Emotional barriers and motivations >Physical and cognitive limitations >Learning needs preferences and readiness to learn >The specific questions to be answered in Alec regarding learning assessment are the following: 1. Does the patient/guardian have any barriers to learning? 2. What is the primary language of the patient/guardian? 3. How does the patient/guardian prefer to learn new content? 33 15. Based on the needs identified in the learning assessment, patients/families should receive education on: >Disease processes and treatment plan >Safe and effective use of medication and medical equipment >Potential drug-food interaction >Nutrition and dietary needs >Rehabilitative techniques >Community resources >When and how to obtain further treatment These items are teaching points on the General Teaching Title in Patient Education. 34 16. Where do you find the hospital’s guidelines on patient education? The policy for patient education is EDU 17.1.01 and handouts are available in Alec via Clinical References, we use software from ExitCare. 17. What are you required to document regarding patient education? >Preferred language, barriers to learning, preferred learning style(s) >The reassessment of learning needs and challenges >Ongoing teaching, including informal sessions and structured classes >Patient/caregiver responses 35 18.How do you involve patients in education and how do you know they have learned what you have taught? Encouraging questions and involving patients and families in decisions about their care promotes an interactive approach to patient education. Asking patients questions such as “What would you do if your catheter falls out after you go home?” is a good way to evaluate teaching effectiveness. Having patients perform demonstrations of a self-care measure is another method of evaluation. Your evaluation of the patient’s learning must be documented in the medical record. 19. How do you make patient education collaborative andinterdisciplinary when more than one discipline is involved in teaching? When more than one discipline is involved in the care of the patient, those same disciplines participate in the various aspects of patient and family 36 teaching. Each discipline has access to all documentation in the patient medical record. 20.What is meant by continuum of care? One of our goals in providing patient care is to maximize the coordination of services among health care providers across a variety of settings. Continuum of care refers to our process for coordinating care and services to: >Meet the ongoing needs of individuals before, during and after hospitalization >Assess that appropriate information is provided, not only to the patient and family, but to subsequent caregivers as well. 37 Examples of services provided within the acute care setting include pharmacy, dietary, physical medicine and rehabilitation, care management, social services and pastoral care. Examples of services which extend beyond the hospital include sub-acute care, extended nursing facility care, home care, hospice and other community based healthcare services (i.e., a clinic, community education). 21. How do we ensure that patients who come to AAMC have access to care? Our goal is to ensure access to appropriate care. Admission to each patient care unit is guided by criteria. Prior to, during, and after admission, we assess the patient’s status to determine if we can provide the needed care. If not, we facilitate transfer to a more appropriate unit or to another health care facility. When patients are admitted, referred, transferred or discharged, we make sure the appropriate patient care information is communicated to subsequent health care providers. 38 22. What do we do to ensure that the patient and/or family receive information concerning the care to be given during the patient’s hospitalization? Dissemination of information regarding procedures and/or treatment options are initiated by the physician and reinforced by all disciplines involved in the patient’s care. 23. Describe some of the ways you communicate information to other healthcare professionals? We communicate with each other by written forms, telephone, fax, computerized documentation and/or in person to be certain information is relayed from one health care provider to the next. We document assessments, plans and interventions on the medical record for review by all team members. 39 24. What standardized tool does AAMC use in communicating hand off patient care? SBAR 25. What does SBAR stand for? S–Situation: What is happening at the present time? B–Background: What are the circumstances leading up to this situation? A–Assessment: What do I think the problem is? R–Recommendation: What should we do to correct the problem? 26. Why do we use SBAR? 40 To help our healthcare team communicate in ways that improve patient safety, increase clarity, and provide a concise reporting method. This in turn, will lead to a reduction in harm, increased satisfaction for all providers and overall better outcomes for patients and their families. 27. How do we make referrals to the Care Management department? Care Managers and Social Workers are easily accessible on the unit, collaborating with other members of the healthcare team to facilitate meeting patient needs. In addition, anyone can make a referral to the Care Management department by telephone at x4180, fax at x4184, or by entering a clinical consult into Alec. 41 28. When does discharge planning begin? Upon admission. It is a multidisciplinary process. 29. How are the needs of patients met after discharge if home care or hospice is necessary? Family/patient in coordination with the care coordinator or social worker would assist in making decisions for discharge. 30. How is the Interdisciplinary Plan of Care developed? The patient’s Plan of Care is determined and developed through collaboration with all disciplines involved in the patient’s care. Each patient’s plan of care in individualized based on the patient’s needs. Goals are identified and mutually agreed upon between the patient and the interdisciplinary team. This information is communicated and documented using the computerized interactive Plan of Care. 42 31. How is the Plan of Care individualized for your patient? >Individualization of a patient’s Plan of Care can be done at several levels: >It starts on assessment when you assess your patient with the fall and skin risk tools, if the patient scores an appropriate level, the care plan topic will be recommended for you via Best Practice Alert (BPA). >Next when you are creating your care plan by applying a template, select specific topics based on what your patient needs. For example, if your patient has had hip surgery then you select that template. >Within the template, select the interventions that apply to your patient. >Finally, write a patient specific goal that you anticipate the patient will reach during the hospital stay. 43 32. What are the Blood Product Administration Key Points? 44 >Obtain pre-transfusion vital signs >Verification of blood product and patient must be made by two nurses before initiation >Blood must be initiated within 30 minutes of Blood Bank release to nurse >Monitor patient during the first 10 to 15 minutes of the transfusion and observe for reaction >Vital signs must be taken 15 minutes after the transfusion was initiated >Continue to monitor vital signs every hour until transfusion is complete >PRBC must be completed within four hours >Vital signs must be taken one hour after the transfusion completed >Once blood product transfusion has completed, stop the blood in the EMR and complete the section 33. What are some fall prevention measures that you can take? >Communicate. Notify the transporter if a patient is at risk for falling. Notify the receiving department if there is a high risk for falls. >Include the fall risk in the handoff report and charge nurse reports. >Assess for risk of falling on admission (within 24 hours), every shift, when transferred to another unit, or after a significant condition change. > Maintain a safe unit environment by conducting an environmental assessment of patient’s environment at the time of admission and at least every shift. >> Remove clutter and tripping hazards from patient’s room. 45 >> Place the call light and frequently used objects within reach. >On admission, discuss patient/staff partnership in preventing falls while hospitalized and provide patient and family with copy of patient education on preventing falls while hospitalized. >Basic fall prevention interventions for all patients include: >> Orient patient to surroundings including bathroom location, use of bed, location of call light. >> Use properly fitting nonskid footwear >> Keep bed in lowest position during use >> Unless specifically indicated, avoid the use of four side rails. Patients can crawl over side rails and fall to floor. 46 > In addition to basic fall prevention interventions, interventions for moderate fall risk patients include: >> Place yellow wrist band on patients. >> Post yellow falling star outside patient’s room. >> Assist patient to the bathroom/commode every two hours, as required by service line. Stay with patient while toileting. >> Supervise and/or assist with bedside sitting, as appropriate. >> Use bedside commode, as appropriate. >> Monitor and assist patient in daily activities. >> Reorient confused patients as necessary. 47 > Evaluate need for: >> PT and/or OT consult >> Activation of bed/chair alarms >> Hip Protectors In addition to basic and moderate fall prevention interventions, the following interventions for high fall risk patients include: > Post red falling star outside of patient’s room > Remain with patient while toileting and performing personal hygiene at sink > Activate bed and chair alarm > When necessary, transport throughout the hospital with assistance of staff. Notify receiving area of high fall risk patients. 48 > For patients who are high fall risk due to neurological deficits: >> Use two person lift until physical therapy has evaluate for specific transfer recommendations >> Following orientation to call light, have patient demonstrate use of call light >> Assist patient with edge of bed sitting > Conduct post-fall assessment on all patients that have fallen and provide either low risk or high risk monitoring. >> Low Risk monitoring – no apparent injury from witnessed fall >> High Risk Monitoring – all unwitnessed falls, falls with actual or potential head/neck injuries, bleeding disorders, and use of anticoagulant and/or antiplatelet agent. 49 34.How do you activate Emergency Response Teams – Code Blue and Rapid Response? Code Blue: Push Code Blue button in patient’s room and/or call x1111 Rapid Response: Call x1111 Who can call Rapid Response? Anyone–Staff (nurse, PCT, dietary, etc.), family members, patients, volunteers, etc. Why would you call Rapid Response? > You are worried about your patient–Call even if you are unsure!! > Acute change in heart rate <40 or >130 beats/minute > Acute change in systolic BP <90 mmHg > Acute change in RR <8 or >28 breaths/minute > Acute change in saturation <90% despite O2 > Acute change in LOC 50 35. What areas call 9-1-1 for medical emergencies? Wayson, Donner, Health Sciences, and Sajak Pavilions including all outpatient regulated space and campus parking areas Exception: Donner Pavilion–inpatient and outpatients in radiation oncology and outpatient infusion center (Code Blue for outpatients; Code Blue and Rapid Response Team for inpatients) 36. How often do you check your emergency code carts? The carts are checked once daily using the code cart checklist to verify that the lock identification number matches the number on the checklist, locks are intact, expiration date is valid, and appropriate items are on top of cart with valid expiration dates. 51 37. How long must an area keep the code cart logs? The current month’s log is kept with the crash cart. A department must keep prior month’s logs in a separate location on the unit for one year. 38.Who controls code carts? Distribution stocks the supplies. The cart is sent to the Pharmacy for drug replacement, a final check and locked. The carts are kept in Distribution for redeployment to patient care areas. 52 Medication Management 1. What does AAMC’s high alert acronym PPINNCH stand for? Pitocin Potassium concentrated IV Insulin Narcotics Neuromuscular blockers Chemotherapy Heparin and other anticoagulants 53 2. What are several ways medications are secured in your work area? Most medications are secured in Pyxis. Individual patient medications are stored in locked drawers outside patient’s rooms, and in med rooms. The code carts contain medications but are secured with a tamper evident lock and checked. 3. What must you do when opening a multi-dose vial? Check the expiration date to ensure it is not out of date. Multi-dose vials must be dated with a 28 day expiration date after opening or shorter as per manufacturer’s recommendations. Vials may be used until the expiration date as long as there is no evidence of contamination. Undated vials must be discarded. 54 4. What is important to remember about labeling medications in OR/Procedural areas? All medications that are removed from the original manufacturer’s container for use in a procedure are to be labeled with the medication name, concentration/strength, quantity/amount, diluents and volume of diluents (if not apparent from the container), and expiration date (24 hours or less). See SNP15.4.12 - Medication labeling and administration in the operating room/procedural areas for more detail. 5. When are Pyxis overrides permitted? Pyxis overrides are permitted during urgent patient care situations when patient harm could result from delay in administration of a medication. When a medication is removed via override, it becomes the responsibility of the person removing and administering the medication to perform the same 55 safety review that a pharmacist would perform before administration to the patient. The override order in the eMAR is then “linked” to a physician’s order by the administering nurse once the original order has been verified by the pharmacist. 6. What is the hospital definition of adverse drug reactions (ADR)? A response to a drug that is unintended and/or unexpected and occurs at doses used for prophylaxis, diagnosis, and treatment. 7. Why is the Medications Reconciliation process important? Patients are at high risk for harm from adverse drug events when communication about medications is not clear. The chance for communication errors increases whenever individuals involved in a patient’s care change. 56 8. When should medication be reconciled? At admission, transfer, and discharge. 9. Who is responsible for ensuring reconciliation occurs? Physicians, nurses, and pharmacists. 57 Medication Reconciliation Tips for Success: 58 • Ensure the medication list is accurate on admission: Enter nurse up-dates to PTA medications via a “note” attached directly to the medication on the admission navigator “Review PTA Meds.” • Ensure all medications have been reconciled at transfer from one unit or service to another. • Ensure all medications have been reconciled at discharge: View “Med Rec Status” on the discharge navigator. • View the “Order Reconciliation History” on the “Patient Summary” as a quick look to see if all medications have been reconciled on admission, at transfer, and discharge. Surgical Services How do you label medications on and off the sterile field? 1. Medication containers include syringes, medicine cups and basins. 2. Label medications and solutions that are not immediately administered. This applies even if there is only one medication being used. Note: An immediately administered medication is one that an authorized staff member prepares or obtains, takes directly to a patient, and administers to that patient without any break in the process. 3. Labeling occurs when any medication or solution is transferred from the original packaging to another container. 4. Labels include the following: Medication name, strength, quantity, diluent and volume (if not apparent from the container), expiration time 59 when expiration occurs in less than 24 hours (for example, Propofol). Note: The date and time are not necessary for surgical and interventional procedures when medications are discarded at the end of the procedure or the end of the day. 60 5. Label each medication or solution as soon as it is prepared, unless it is immediately administered. 6. Label the container after the medication is prepared. 7. Verify all medication or solution labels both verbally and visually whenever the person preparing the medication or solution is not the person who will be administering it. Verification is done by two individuals qualified to participate in the procedure. 8. All medications and solutions both on and off the sterile field and their labels are reviewed by entering and exiting staff responsible for the management of medications. 9. Immediately discard any medication or solution found unlabeled. 10.Remove all labeled containers on the sterile field and discard their contents at the conclusion of the procedure. 11. An expiration date is required when all multi-dose vials are opened and not used within 24 hours. When and how do you conduct a Pre-procedure verification (Universal Protocol)? 1. Pre-procedure verification begins when the patient is scheduled for a procedure. 61 62 2. Key elements to verify include the patient’s name, procedure to be performed and laterality (correct side/site). 3. A pre-anesthesia time out must be done before sedation is given to the patient so that the patient can participate in the time out and confirm the key elements. This timeout is led by the physician providing the sedation. 4. In cases of laterality, the incision site must be marked with the surgeon’s or proceduralist’s initials. 5. Only the indelible ink marker provided by the hospital is to be used the mark the site. 6. If site marking is not possible, the alternative site marking process must be used. In the alternative site marking process the nurse places a white alternative site marking band on the patient during the pre-procedure verification and writes the correct side and site with an approved surgical marking pen. The physician or practitioner performing the procedure must initial the band itself prior to moving the patient to the operating or procedure room to confirm the side or site. Documentation of placement will follow the same documentation for all site markings. The band will not be removed until after the procedure is completed. Note: In NICU, the babies are marked with a betadine swab. 7. The site marking must be visible after the site has been cleansed and draped for the procedure 8. A surgeon/proceduralist-led time-out must occur immediately before the start of the procedure (initial incision or insertion of instrumentation). 9. During the time out, all other activities and conversations are suspended, to the extent possible without compromising patient 63 safety, so that all relevant team members are focused on the active confirmation of the correct patient, procedural site and other critical elements of the procedure. If laterality is indicated, all team members must confirm that the site marking is visible. 64 10.Time-outs must also be conducted before anesthetic blocks (scalene, local, etc.) are done. This time out is led by the physician providing the anesthetic. 11. If a central line must be inserted before the procedure starts, the physician inserting the central line must perform a time-out with members of the procedural team. The central line checklist is to be completed by that physician. 12.All time-outs are to be documented in the patient’s medical record. What is proper surgical attire? 1. Scrubs: Only scrub tops and pants provided by this hospital are worn. Scrubs used in restricted areas are not brought or worn in from home. Personnel are to change into street clothes prior to leaving the hospital. 2. Scrub jackets: Either disposable or non-disposable, only scrub jackets provided by the hospital are to be worn. 3. Clean, fresh, personal scrub hats may be worn in restricted areas only if covered with a fresh, disposable scrub hat/bonnet prior to entry into the operating rooms/sterile procedure areas. 4. Dedicated shoes for restricted areas are recommended. Shoes not dedicated to the restricted areas should be worn with shoe covers while in the restricted areas. 5. Remove shoe covers and masks when leaving the operating room suite. 65 6. Undergarments (e.g., undershirts, turtlenecks) are not permitted to extend beyond the necklines or sleeves of the scrubs. 7. Any jewelry (earrings, necklaces, watches, and bracelets, etc.) that cannot be confined within the surgical attire is not permitted. 8. Fingernail jewelry is not permitted (see policy IC5.1.04 Hand Hygiene). Fingernail polish is not permitted for scrubbed personnel. 9. Remove all personal protective equipment (gloves, masks, booties, etc.) prior to exiting the OR/CSP. Personal protective equipment (PPE) is not permitted beyond the area in which it was used. Disposable surgical bonnets are allowed outside of the restricted areas only if not visibly soiled or wet, and must be replaced upon re-entry into restricted areas. 10. Fanny packs, backpacks, and briefcases should not be taken into the restricted area. 66 Surveillance, Prevention, and Control of Infection 1. What are some measures used to prevent transmission of infectious diseases to staff and to patients? Isolation precautions may be instituted by the nursing staff without a physician’s order. AAMC’s mandatory immunization program protects both staff and patients. Environmental cleaning has become increasingly important in the fight against transmission, particularly with antibiotic-resistant organisms. Hand hygiene remains the single most important factor in preventing the spread of infectious diseases. 2. When should hand hygiene be performed? Hand hygiene (washing hands or use of alcohol-based handrub) should be performed before and after touching a patient or any equipment that touches a patient. Wash your hands with soap and water when hands are 67 visibly soiled/contaminated, before eating, after using the restroom, and whenever caring for a patient with Clostridium difficile (Cdiff). AAMC follows Centers for Disease Control and Prevention (CDC) guidelines. 3. How is hand hygiene monitored and promoted at AAMC? Hand hygiene is monitored through audits conducted by “secret shoppers” on every patient unit and the Emergency Department. Compliance is compared housewide, per patient unit, and per type of healthcare worker role. AAMC is a member of the Maryland Hand Hygiene Collaborative in order to foster improved hand hygiene by healthcare workers, patients, and visitors. Alcohol-based handrub, hand wipes on food trays, hand hygiene education in the patient handbook, and housewide signage are only some of the examples of how hand hygiene is promoted at AAMC. Be prepared to discuss the most current data on hand hygiene compliance for the hospital and your area, as well as how your area is promoting hand hygiene. 68 Fingernails are to be short (less than ¼ inch in length); if nail polish is used, it should be clear and intact. Persons involved in patient care or handling linen, patient supplies, food, etc. are not allowed to wear artificial nails. 4. What are the steps to placing a patient in isolation? >Identify the appropriate isolation and hang an isolation sign on entry to the patient room. >Order isolation in the computer (physician’s order is not required). >Gather the correct personal protective equipment (PPE) and place at entry to patient room. >Educate patient/family members on need for isolation and expectations of them to maintain isolation. Use handouts located on intranet to assist with education. 69 >Perform hand hygiene and put on PPE prior to entry. Dispose of PPE in room upon exit and perform hand hygiene. >With patient transfer or discharge, leave the isolation sign posted for environmental services (EVS) to remove following cleaning of room. 5. What infection control and prevention education is important to provide to your patient/patient’s family? Any time a patient is diagnosed with an infectious disease or is about to undergo a procedure there is an opportunity for infection prevention education. Upon admission and throughout a patient stay, hand hygiene is emphasized. The Joint Commission emphasizes the need for education of patients and family members, and looks for documentation of education for the following conditions/situations: 70 >Identification of multidrug-resistant organisms (MDROs), such as MRSA, VRE, etc., and Clostridium difficile (Cdiff) >Placement in isolation > Prior to insertion of a central line (central line-associated bloodstream infection (BSI) prevention) > Prior to surgery (surgical site infection (SSI) prevention) 6. What infection prevention strategies are used during the insertion of a central line (central venous catheter)? Remember the central line insertion checklist (make sure to document): > Have proper hand hygiene > Use a sterile drape to cover patient (maximum barrier precautions) 71 > PPE: sterile gloves, cap, gown, mask, eye protection for inserter/assistant; mask with eye shield for everyone else in the room >Chlorhexidine skin prep or alternative if allergic >Avoid femoral vein unless there are no other options. 7. How long does a disinfectant wipe or solution need to make contact in order to kill bacteria and other microorganisms? Germicidal wipes or bleach-impregnated wipes are used to wipe down equipment, including IV pumps, stethoscopes and keyboards between patient use. Sometimes staff will also use germicidal solution (for example, Virex), used mostly by environmental service (EVS) staff for cleaning rooms, for bigger items, such as stretchers. Whatever used, you are expected to know how long the equipment needs to stay wet (contact/kill time) in minutes to be effective. 72 Remember: Germicidal PDI AF3 (grey top) Wipes = 3 minutes Bleach Wipes (for example, Dispatch) = 5 minutes Virex Spray Solution = 10 minutes 8. How are employees exposed to bloodborne pathogens reported? Exposures are reported by the exposed employee to their supervisor. Employees exposed to bloodborne pathogens must be evaluated in Employee Health Monday to Friday 7:30am to 4pm and in the Emergency Department at all other times. This evaluation must occur immediately as the window for giving antiviral medications, if needed, is two hours. 9. How are communicable diseases reported at AAMC? The Infection Control Department has the responsibility for reporting communicable diseases to the local and state health departments. 73 Physicians may also report as needed. The laboratory also reports any test results regarding communicable diseases. 10. How are infection control concerns reported? Infection control concerns may be reported to Infection Control at x6446 or the 4PTS hotline at x4787. Immediate concerns can also be addressed by paging the hospital epidemiologist and/or director of Infection Control. 11. Where does staff receive education on infection control? All staff receive infection control education in orientation and annually on Healthstream. Also, infection control practices are integrated into competencies. Infection control programs are also offered in specific departments as issues and concerns are identified. Infection Control personnel may be contacted for questions or consultation. Resources are also found on the hospital Infection Control intranet site. 74 12. What are some of the monitors in AAMC’s Infection Control program? The Infection Control program does surveillance of surgical site infections in high risk, high volume surgeries, central line-associated bloodstream infections, ventilator-associated pneumonias, urinary catheter-associated urinary tract infections, blood culture contamination rates and other high risk indicators. Surveillance also includes incidence of hospital-acquired multidrug-resistant organisms (MDROs) and Clostridium difficile (Cdiff) and other organisms. Environmental testing, such as water testing for Legionella, is coordinated through engineering and monitored by Infection Control. Infection Control Risk Assessments (ICRAs) are conducted prior to construction projects. 75 13. How is selection of surveillance/monitoring determined by Infection Control? Selection of what surveillance/monitors are conducted is dependent on the level of risk associated with patients, staff, and visitors. Periodic and as needed risk assessments are performed in order to prioritize needs for surveillance/monitoring. Annually, the risk assessments are used to determine priorities; goals for the coming year are determined based on the risk assessment and listed in the Infection Control Plan, available for review on the Infection Control section of the hospital intranet. 76 14. How are data from the Infection Control activities reported? All reports are presented at the monthly Infection Control Committee; data for specific patient populations are reported at service line and nursing quality councils, critical care committee, and shared at staff meetings. Nursing Quality indicators (NDNQI) include unit-based infections data. Be aware of the infections data which relates to your area of service. 77 Improving Organizational Performance 1. What are Core Measures? 78 They are measures identified by the Joint Commission that allow for a robust assessment of care provided in focused areas. The following are Core Measure areas which are collected and monitored: • Acute Myocardial Infarction (AMI) • Heart Failure (HF) • Pneumonia (PN) • Surgical Care Improvement Project (SCIP) • Children Asthma Care (CAC) • Venous Thromboembolism (VTE ) For more information on metrics, contact Carole Clarke at x1327. 2. How do I know what is important in terms of performance? The Board of Trustees determines strategic aims that are important to AAMC. The following are the strategic aims for FY14: > Preventable death > Harm reduction > Patient satisfaction > Hospital acquired infections > Re-admissions > Medication reconciliation > Core measures 79 These are based on organizational priorities, considered important, high volume, high-risk, and sometimes, new services. This information is communicated through our Quality unit and services line councils. 3. How can I improve performance on my unit? Work with your unit leadership and/or participate in unit quality councils and performance improvement projects. 4. How do I know what performance improvement projects are occurring on my unit? Information is posted in staff areas regarding projects. Frequently, the data is displayed graphically so you can visually see how successful we are. Please ensure you know your department’s performance Improvement projects, how you are doing and what actions are being taken to improve the measure. 80 5. What if the data shows we are not doing as well as we hoped? We closely analyze the data to determine what the issues and obstacles (opportunities for improvement) are. Once issues are identified we can make corrections. 6. What is the specific methodology used at AAMC for performance improvement activities? PDCA (Plan-Do-Check-Act) is our problem solving framework: Plan: Plan the improvement Do: Do the improvement and data collection Check: Check the results of the implementation Act: Act to maintain the gain and continue improving. 81 7. What is the definition of a Sentinel Event? A Sentinel Event is an unexpected occurrence involving death or serious physical or psychological injury, or the inherent risk thereof, including any process variation for which a recurrence would carry a significant chance of serious adverse outcome. (See Sentinel Event policy QI6.1.09 for criteria). 8. What is a Near Miss? A Near Miss is an event that does not meet the definition of a Sentinel Event, but involves a process variation for which a recurrence would carry a significant chance of a serious outcome. 9. How are incidents reported at AAMC? Incidents can be reported directly to Department Managers and in turn are reported to Administration. You may also use the 4PTS Patient Safety Hotline (443-481-4787). 82 10. What is the process of Failure Modes Effects Analysis (FMEA)? This is a process that is used for systematic, proactive approach for identifying the ways that a process or design may fail, and how it can be safer. The focus is on preventing errors before they occur, enhancing patient safety and increasing customer satisfaction. 11. What is a Root Cause Analysis (RCA)? A Root Cause Analysis is systematic process that uses information gathered during an investigation to determine the fundamental system deficiencies that led to the incident. The goal is to analyze incidents to identify root causes and fix underlying system problems to prevent recurrence of a similar event. AAMC conducts root cause analyses for identifying the base or contributing casual factors that underlie variations in performance associated with adverse events or near-misses (See Sentinel Event QI6.1.09 policy for details). 83 12. What are the terms Lean and RIE? Lean: The core idea is to maximize customer value while minimizing waste. RIE: A rapid improvement event is a part of the Lean toolkit and provides a mechanism for making radical changes to current processes and activities within a very short time scale. What are some examples of Lean RIEs implemented: > Linen management > Perioperative scheduling > Care management > Pharmacy > Revenue cycle > Supply chain 84 Management of the Environment of Care 1. What is the smoking policy of the hospital? AAMC has a smoke-free hospital campus. 2. What are the codes to signal an emergency? The codes are: > Code Red Mr. Firestone: Fire > Code Pink: Infant/Child Abduction > Code Blue: Cardiac Arrest > Code Gold: Bomb Threat > Code Orange: Hazardous Material Spill > Code Yellow: Emergency or Disaster > Code Silver: Active Weapon Threat 85 3. What should you remember in the event of a fire? The employee should be aware of the location of the pull stations (near the exit) and the fire extinguishers in their work area. Areas to respond to the fire should be the floor of origin, one floor below and two floors above the fire’s origin. One strip of tape should be placed on empty patient rooms to indicate the room is empty. The acronym used is R.A.C.E., which stands for: Remove the patient from danger Announce (pull the alarm) Contain the fire (shut doors) Extinguish the fire or evacuate 86 4. How frequently are fire drills conducted? Fire drills are conducted once per shift per quarter in each area, except during periods of construction when frequencies are two per shift per quarter. 5. In what ways does the hospital support a secure work environment? The hospital provides four security officers on duty per shift. These officers do hazard surveillance rounds internally and externally. 6. What should an employee do if they see a suspicious person or activity on campus or need help restraining a violent person? They should ask the person if they need assistance, and should keep the person in view and call Security immediately at x6911. 87 7. What body within the hospital is charged with evaluating the institution in terms of general safety, utilities management, equipment management, emergency management, security interim life safety and hazardous materials/waste? The Environment of Care Committee leads these efforts. 8. How do you identify emergency powered electrical outlets? These outlets are red or labeled. 9. How are you notified of expected utility interruptions? Advanced notice is given to all staff via email, or the PA system is used for immediate notification. 88 10. Are extension cords prohibited for hospital use? The use of extension cords is limited to certain situations and must be approved by Maintenance or Biomedical Engineering for medical equipment. 11. What should you do if the hospital lost access to water? The loss should be report to the Engineering department. They will provide alternatives (i.e., bottled water for drinking). 12. Who is authorized to shut off an area’s medical gas? In an emergency situation the charge nurse shuts off oxygen as authorized by the fire marshall. When the emergency situation is identified, notify the hospital operator and the administrative coordinator. Take the necessary actions to handle the situation according to hospital policy and communicate the shut down of the gases to the appropriate people i.e., Respiratory Therapy. 89 13.What should you do if there is a chemical spill? 90 > Remove everyone from the immediate area > Consult the Material Safety Data Sheets (MSDS). To obtain the necessary information, call the 3E Company at 1-800-451-8346. They will respond immediately by fax or email. > Please follow the Spill Response-Action by Category Chart (Code Orange in the Emergency Procedure Quick Reference Guide). > If it is mercury, the spill kits are available from the Environmental Services Department. > Notify your manager/supervisor. > Complete a Patient Safety Report (formerly known as an Incident Report). 14. How can you protect yourself, patients and the environment from exposure to hazardous chemicals? • Read and follow directions from the Material Safety Data Sheets (MSDS) • Proper storage, handling and disposal of waste. Report any unsafe conditions to your supervisor or Security at x6911. 91 Radiation Safety If you are identified as a worker in a radiation area, how do you protect yourself from radiation exposure at work? After using your lead apron, hang it up. Protective aprons have a sheet of soft lead impregnated rubber on the inside. If it is folded or creased it can fracture. When this happens, the protective nature of the apron is lost. Don’t forget to hang up your lead apron properly every time you take it off. Wear your radiation badge, store it appropriately, and turn it in every month, on time. That is the best way to know if you have been exposed to radiation. 92 Emergency Management 1. How does the hospital prepare staff for a disaster which might involve a large number of patients admitted to the hospital? The Incident Commander conducts two disaster drills per year. 2. What are the six critical functions of hospitals in relation to Emergency Management? 1) Communications 2) Resources and assets 3) Safety and security 4) Staff roles and responsibilities 5) Utilities management 6) Patient clinical and support activities 93 3. What are staff responsibilities during any type of a disaster? Know and follow the guidance in the EOC 4.4.01 Emergency Operations Plan. The main aspects for staff to follow are: 1. To protect the lives of your patients and families to the best of your ability 2. To conserve property, such as knowing what to do in a fire (RACE) 3. To continue to provide and manage patient care to the best of abilities during a disaster. 4. How do you maintain patient safety when utilities fail? Some of the ways these situations are managed is by using portable oxygen, flashlights, cell phones, bottled water, and manual respiratory equipment. 94 Leadership The Leadership at AAMC is responsible for: >The safety and quality of care, treatment, and services >A culture that fosters safety as a priority for everyone who works in the hospital >The planning and provision of services that meet the needs of patients >The availability of resources—human, financial and physical—for providing care, treatment and services >The existence of competent staff and other care providers >Ongoing evaluation of and improvement in performance 95 How do we ensure that our clinical contracted services are performing high quality and safe care to our patients? Each service line quality council is responsible to select the measures for the clinical contracted services in their area and monitor those measures on a quarterly basis to ensure that high quality and safety care are provided through the contractual agreement. 96 Information Management 1. Do you have the necessary computer access to do your job? Yes. My computer access is based on my role as caregiver. If my role changes, my new role will require different access. Access changes are requested by my supervisor. 2. How often is the computer system unavailable? Every third Wednesday of the month at 2am the system is potentially unavailable for two hours maximum for routine maintenance and upgrades. Longer downtimes are coordinated and communicated differently. 97 3. What guidelines do you follow if the computer system is down? I follow the Integrated Computer Downtime Management policy. IS9.1.03. Depending on the scope of the downtime I may have access to > SRO (Shadow Read Only): The network is still available which will allow read only access to the patient record or > BCA (Business Continuity Access) printers: These allow you to print a patient summary, which is used when there is no network connectivity. 98 Human Resources 1. Do you function according to your job description? Yes. All employees sign off on their job descriptions through Performance Manager at time of hire, or transfer into new job/department. All job descriptions are available to any employee through the Job Descriptions tab in Performance Manager. 2. What skills are you required to maintain for competency in your department? There are department- and job-specific competencies that are required in addition to the hospital-wide competencies. These are documented and kept on file with your job description, annual performance evaluation and other educational records. 99 3. What education programs are you required to attend? All employees are required to attend AAMC’s new hire orientation. All employees are expected to complete annual hospital-wide educational programs (for example, fire safety, electrical safety, infection control, hazardous materials, right to know, personal safety, TB, bloodborne pathogens [for those at risk for exposure] and cultural awareness). Nurses attend the Nursing Service Orientation during the first week on the job. Employees that use Alec are required to take Alec computer training courses appropriate for their duties. Any job-specific educational offering to address particular patient populations and unit specialty topics, or any applicable new rules or regulations may also be required. From time to time, there is a house-wide competency, such as Disruptive Behavior training. 100 4. Why are specific competencies chosen? Specific competencies are determined by your position responsibilities and are based on risk; volume; whether it’s a new procedure, equipment or technology; and changes in policy or procedures. 5. Are you provided with education to maintain population-specific competency? Yes. Training is related to the population (age, bariatric, developmental challenges, etc.) served and competencies are updated and defined annually. 6. What educational programs have you attended recently? Think about what educational program you have completed recently and write them down in the following space (for example, pain management, ethics seminars, hospital grand rounds, weekly cancer conferences, etc.). 101 Notes: 102 Notes: 103 Notes: 104 105 2001 Medical Parkway Annapolis, MD 21401 443-481-1000 TDD: 443-481-1235 www.aahs.org