* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Heidelberg Retina Tomograph und Papille
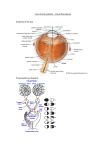
Photoreceptor cell wikipedia , lookup
Retinal waves wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Fundus photography wikipedia , lookup
Macular degeneration wikipedia , lookup
Optical coherence tomography wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Diabetic retinopathy wikipedia , lookup
Heidelberg Retina Tomograph und Papille Medline Abstracts November 1996 bis August 2001 Invest Ophthalmol Vis Sci 2001 Aug;42(9):1993-2003 Detecting early glaucoma by assessment of retinal nerve fiber layer thickness and visual function. Bowd C, Zangwill LM, Berry CC, Blumenthal EZ, Vasile C, Sanchez-Galeana C, Bosworth CF, Sample PA, Weinreb RN. Glaucoma Center, Department of Ophthalmology, University of California San Diego, La Jolla 92093-0946, USA. PURPOSE: To compare the abilities of scanning laser polarimetry (SLP), optical coherence tomography (OCT), short-wavelength automated perimetry (SWAP), and frequency-doubling technology (FDT) perimetry to discriminate between healthy eyes and those with early glaucoma, classified based on standard automated perimetry (SAP) and optic disc appearance. To determine the agreement among instruments for classifying eyes as glaucomatous. METHODS: One eye of each of 94 subjects was included. Healthy eyes (n = 38) had both normal-appearing optic discs and normal SAP results. Glaucoma by SAP (n = 42) required a repeatable abnormal result (glaucoma hemifield test [GHT] or corrected pattern standard deviation [CPSD] outside normal limits). Glaucoma by disc appearance (n = 51) was based on masked stereoscopic photograph evaluation. Receiver operating characteristic (ROC) curve areas, sensitivities, and specificities were calculated for each instrument separately for each diagnosis. RESULTS: The largest area under the ROC curve was found for OCT inferior quadrant thickness (0.91 for diagnosis based on SAP, 0.89 for diagnosis based on disc appearance), followed by the FDT number of total deviation plot points of < or =5% (0.88 and 0.87, respectively), SLP linear discriminant function (0.79 and 0.81, respectively), and SWAP PSD (0.78 and 0.76, respectively). For diagnosis based on SAP, the ROC curve area was significantly larger for OCT than for SLP and SWAP. For diagnosis based on disc appearance, the ROC curve area was significantly larger for OCT than for SWAP. For both diagnostic criteria, at specificities of > or =90% and > or =70%, the most sensitive OCT parameter was more sensitive than the most sensitive SWAP and SLP parameters. For diagnosis based on SAP, the most sensitive FDT parameter was more sensitive than the most sensitive SLP parameter at specificities of > or =90% and > or =70% and was more sensitive than the most sensitive SWAP parameter at specificity of > or =70%. For diagnosis based on disc appearance at specificity of > or =90%, the most sensitive FDT parameter was more sensitive than the most sensitive SWAP and SLP parameters. At specificity > or = 90%, agreement among instruments for classifying eyes as glaucomatous was poor. CONCLUSIONS: In general, areas under the ROC curve were largest (although not always significantly so) for OCT parameters, followed by FDT, SLP, and SWAP, regardless of the definition of glaucoma used. The most sensitive OCT and FDT parameters tended to be more sensitive than the most sensitive SWAP and SLP parameters at the specificities investigated, regardless of diagnostic criteria. Arch Ophthalmol. 2001 Jul;119(7):1069-70 Discriminating between normal and glaucomatous eyes using the Heidelberg Retina Tomograph, GDx Nerve Fiber Analyzer, and Optical Coherence Tomograph. Zangwill LM, Bowd C, Berry CC, Williams J, Blumenthal EZ, Sanchez-Galeana CA, Vasile C, Weinreb RN. Glaucoma Center, Department of Ophthalmology, University of California-San Diego, La Jolla, CA 92093-0946, USA. 1 OBJECTIVE: To compare the ability of 3 instruments, the Heidelberg Retina Tomograph (HRT), the GDx Nerve Fiber Analyzer (GDx), and the Optical Coherence Tomograph (OCT), to discriminate between healthy eyes and eyes with early to moderate glaucomatous visual field loss. SUBJECTS AND METHODS: Forty-one patients with early to moderate glaucomatous visual field loss and 50 healthy subjects were included in the study. The HRT, GDx, and OCT imaging and visual field testing were completed on 1 eye from each subject within a 6-month interval. Statistical differences in sensitivity at fixed specificities of 85%, 90%, and 95% were evaluated. In addition, areas under the receiver operating characteristic (ROC) curve were compared. RESULTS: No significant differences were found between the area under the ROC curve and the best parameter from each instrument: OCT thickness at the 5-o'clock inferior temporal position (mean +/- SE, 0.87 +/- 0.04), HRT mean height contour in the nasal inferior region (mean +/- SE, 0.86 +/- 0.04), and GDx linear discriminant function (mean +/- SE, 0.84 +/- 0.04). Twelve HRT, 2 GDx, and 9 OCT parameters had an area under the ROC curve of at least 0.81. At a fixed specificity of 90%, significant differences were found between the sensitivity of OCT thickness at the 5-o'clock inferior temporal position (71%) and parameters with sensitivities less than 52%. Qualitative assessment of stereophotographs resulted in a sensitivity of 80%. CONCLUSION: Although the area under the ROC curves was similar among the best parameters from each instrument, qualitative assessment of stereophotographs and measurements from the OCT and HRT generally had higher sensitivities than measurements from the GDx. Am J Ophthalmol 2001 Jul;132(1):57-62 Interobserver variability of optic disk variables measured by confocal scanning laser tomography. Iester M, Mikelberg FS, Courtright P, Burk RO, Caprioli J, Jonas JB, Weinreb RN, Zangwill L. Department of Ophthalmology, University of British Columbia, Vancouver, Canada. PURPOSE: To assess the interobserver variation of confocal laser scanning tomographic measurements of the optic nerve head and to address the question of whether the addition of clinical optic disk photographs is helpful in outlining the optic disk margin and in reducing the observerrelated variation of the measurements. PATIENTS AND METHODS: Optic disk variables for 16 eyes of 16 patients with glaucoma, generated by confocal laser scanning laser tomography (Heidelberg Retina Tomograph), were independently evaluated by four experienced glaucoma specialists, and the interobserver variability was calculated. A second separate review by the same observers included the use of clinical stereoscopic color optic nerve head photographs to aid definition of the optic disk margin. RESULTS: Optic disk parameters with the smallest interobserver variation were cup shape measure, maximum cup depth, height variation contour, and mean height contour. The intraobserver variation of these parameters did not increase when clinical optic disk slides were additionally available. Parameters with the highest interobserver variation were volume below surface, volume below reference, volume above surface, and volume above reference. The observer variation of these optic disk parameters increased significantly for two of the four examiners when clinical optic disk slides were additionally available for outlining the optic disk margin. CONCLUSION: Confocal laser scanning tomography of the optic nerve head can be improved significantly if clinical optic disk photographs are additionally available to help in outlining the optic disk margin. Because interobserver variation in the tomographic optic disk measurements can be significant, even if experienced observer are involved, tomographic optic disk measurements may be centralized in reading centers in the case of multicenter studies. Am J Ophthalmol 2001 Jun;131(6):716-721 The effects of astigmatism and working distance on optic nerve head images using a Heidelberg Retina Tomograph scanning laser ophthalmoscope. 2 Sheen NJ, Aldridge C, Drasdo N, North RV, Morgan JE. Department of Optometry and Vision Sciences, Cardiff University, Cardiff, United Kingdom. PURPOSE: To determine effects of astigmatism and working distance on optic nerve head images in normal patients using the Heidelberg Retina Tomograph. METHODS: The optic disks of 51 normal healthy subjects, aged 19 to 44 years, were imaged through dilated pupils. Subjects with 0.75 DC or less of astigmatism were imaged without correction at a working distance of 15 mm. They were then re-imaged with a cylindrical correction of +3.00 DC at 90 degrees axis (n = 20). Naturally astigmatic subjects with more than 1.00 DC were imaged without correction and then reimaged once this was neutralized with their appropriate spectacle prescription (n = 15). The effects of working distance were studied using subjects with 0.75 DC or less (n = 16). Two working distances were used, 15 and 25 mm. At each session the means of three topographic images were taken from which standard deviations and parameters were recorded. Parameters analyzed included cup shape measure, rim area, and inferior temporal rim volume. Z-profile full width at half maximum was calculated from one image per subject for each condition. RESULTS: No significant difference was found in the measured parameters of the optic disk for any astigmatic condition or changes in working distance (P >.05), (paired t test). Both the standard deviation of the mean topographic images and the Z-profile half-maximum width of the axial intensity profile were significantly greater with induced astigmatism of +3.00 DC (P values 0.3 and.00, respectively). CONCLUSIONS: Optic disk parameters are not significantly affected by uncorrected astigmatism (up to 2.50 DC) or working distance. The algorithm used by the Heidelberg Retina Tomograph to generate topographic maps is sufficiently robust that astigmatism up to 2.50 DC does not require correction. Optom Vis Sci 2001 Jun;78(6):431-435 Age-related topographical changes in the normal human optic nerve head measured by scanning laser tomography. Kergoat H, Kergoat MJ, Justino L, Lovasik JV. School of Optometry, University of Montreal, Quebec, Canada. [email protected] PURPOSE: This study was designed to investigate the effects of advanced aging on the optic nerve head (ONH) structure and retinal nerve fiber layer (RNFL) thickness in the eldest segment of our population. METHODS: Twenty-seven healthy elderly subjects between 75 and 88 years of age (average, 80.1 +/- 0.83 years) and 30 healthy younger subjects between 20 and 32 years of age (average, 23.1 +/- 0.50 years) were recruited for a cross-sectional comparison between ONH morphology and RNFL thickness as measured by scanning laser tomography. The ONH disc, cup, and rim areas; cup-to-disc ratio; and the mean thickness of the RNFL were quantified. RESULTS: The cup and disc areas as well as the cup-to-disc area ratio increased with age, whereas the RNFL thickness decreased during the course of normal senescence. CONCLUSIONS: Any diagnoses of ocular pathology in the elderly must differentiate the effects of normal aging on the ONH topography and RNFL thickness. To that effect, the present study provides a clinical profile of ocular structures that extend into the oldest geriatric age group. Ophthalmic Physiol Opt 2001 May;21(3):173-181 The influence of contour line size and location on the reproducibility of topographic measurement with the Heidelberg Retina Tomograph. Roff EJ, Hosking SL, Barnes DA. Neurosciences Research Institute, School of Life and Health Sciences, Aston University, Aston Triangle, Birmingham B4 7ET, UK. 3 BACKGROUND: The recommended contour line (CL) location with the Heidelberg Retina Tomograph (HRT) is on the inner edge of Elschnig's scleral ring. This study investigated HRT parameter reproducibility when: (i) the CL size is altered relative to Elschnig's ring; (ii) the CL is either redrawn or imported between images. METHODS: Using the HRT, seven 10 degrees images were acquired for 10 normal volunteers and 10 primary open angle glaucoma (POAG) subjects. A CL was drawn on one image for each subject using Elschnig's scleral ring for reference and imported into subsequent images. The CL diameter was then (a) increased by 50 microns; (b) increased by 100 microns; and (c) decreased by 50 microns. To investigate the effect of the method of contour line transfer between images a CL was: (1) defined for one image and imported to 6 subsequent images; (2) drawn separately for each image. RESULTS: Parameter variability improved as the size of the CL increased for the normal group relative to Elschnig's ring but was unchanged in the POAG group. The export/import function (method 1) resulted in better parameter reproducibility than the redrawing method for both groups. CONCLUSIONS: The exporting and importing function resulted in better parameter variability for both subject groups and should be used for transferring CLs across images for the same subject. Increasing the overall CL size relative to Elschnig's scleral ring improved the reproducibility of the measured parameters in the normal group. No significant difference in parameter variability was observed for the POAG group. This suggests that the reproducibility of HRT images are affected more by the variation in topography between images than change in CL definition. Surv Ophthalmol 2001 May;45 e :S297-S303 Clinical detection of optic nerve damage: measuring changes in cup steepness with use of a new image alignment algorithm. Burk RO, Rendon R. Department of Ophthalmology, University of Heidelberg, Heidelberg, Germany.burk,[email protected] The purpose of this study was to study the effect of a subpixel image alignment algorithm on the standard deviation (SD) of mean topography images obtained by laser scanning tomography and to evaluate changes of the cup shape measure parameter (CSM) over time based upon the individual parameter variability using the new algorithm. Triple measurements from optic nerve heads of 132 eyes of 132 subjects were obtained using the Heidelberg Retina Tomograph HRT. To calculate a mean topography image from three single topography images, alignment of the raw optical section image data was performed with the standard software and again with a new subpixel-based image alignment algorithm. The effect on the averaged (SD) of the mean topography images was evaluated. CSM was evaluated in 15 eyes of 15 normal subjects (N) and 28 eyes of 14 glaucoma patients (G) over a period of 28.6 +/- 4.6 months (N) and 28.56 +/- 5.2 months (G) respectively. A change in the CSM value over time was considered significant if CSM measurements exceeded two standard deviations of this variable determined for the individual eye. Mean-topography image SD was 22.86 +/- 8.2 microns (min. 9.5 microm; max. 47.8 microm) with the standard alignment procedure and 15.46 +/- 6.8 microm (min. 6.8 microm; max. 42.8 microm) with the new algorithm. The average SD improvement was 7.46 +/- 3.9 microns (min. -8.1 microm; max. 28.7 microm). The coefficient of correlation of both methods was R(2) = 0.77 (p < 0.0001). No control group eye demonstrated significant changes of CSM in the follow-up period. The CSM indicated an increase in cup steepness in 4 eyes of 4 glaucoma patients. In one of these four eyes, a deterioration of the visual field was identified by white on white perimetry. The new image alignment algorithm significantly reduces the SD of mean topography images calculated from identical raw data. If topometric variables are evaluated over time, the individual variability of data should be taken into account. 4 Curr Opin Ophthalmol 2001 Apr;12(2):100-104 The diagnostic value of optic nerve imaging in early glaucoma. Mardin CY, Junemann AG. Department of Ophthalmology, Friedrich-Alexander Universitat Erlangen-Nurnberg, Erlangen, Germany. [email protected] In the last decade, new imaging techniques have been added to conventional fundus photography and have been evaluated for use in early glaucoma. They all measure the loss of neuroretinal rim or retinal nerve fiber layer as a correlate to glaucomatous ganglion cell and axon loss. The value of optic disc photography, planimetry, laser scanning tomography, laser scanning polarimetry, and optical coherence tomography for the diagnosis of glaucomatous eyes in a preperimetric or early perimetric stage is analyzed on the basis of sensitivity, specificity, and receiver operating characteristics (ROC) curves. It becomes clear that all these techniques allow a more or less semiautomated evaluation of the optic disc and retinal nerve fiber layer but still have their limitations in the diagnosis of a very early, preperimetric stage of the glaucoma disease. J Glaucoma 2001 Apr;10(2):95-101 Ability of peripapillary atrophy parameters to differentiate normal-tension glaucoma from glaucomalike disk. Park KH, Park SJ, Lee YJ, Kim JY, Caprioli J. Department of Ophthalmology, Seoul National University College of Medicine, Korea. PURPOSE: To investigate the ability of peripapillary atrophy (PPA) parameters to differentiate normal-tension glaucoma (NTG) from glaucomalike disk (GLD). METHODS: Thirty-three eyes of 33 patients with GLD that had no evidence of visual field defect and retinal nerve fiber layer defect and 33 eyes of 33 patients with NTG, matched with age and intraocular pressure, were enrolled. The participants were selected from the database of patients referred from a routine health checkup because of high cup-to-disk ratio (>0.5). Topographic measurements for the optic disk were performed using the Heidelberg Retina Tomograph (HRT). The extent of PPA (zone beta) was measured with Atrophy Zone Analysis software of HRT. Receiver operating characteristic (ROC) curves (GraphROC version 2.0) were used to compare the new formula including PPA parameters with that of the HRT discriminant analysis formula in differentiating NTG from GLD. RESULTS: The area of zone beta, atrophy-to-disk area ratio, and angular and radial extent of zone beta were significantly larger in NTG (P < 0.01). Multiple logistic regression analysis showed that rim area and corrected radial extent of zone beta are variables that show significant difference between NTG and GLD (P < 0.05). The area under the ROC curve for the new formula including rim area and corrected radial extent of zone beta (0.8655) was significantly larger than that for the HRT discriminant analysis formula (0.7351) (P = 0.0128). CONCLUSION: The PPA measurement obtained by HRT can be a useful additional tool to differentiate NTG from GLD after the first screening by disk photograph in a routine health checkup. Ophthalmic Physiol Opt 2001 Mar;21(2):139-150 How large is the optic disc? Systematic errors in fundus cameras and topographers. Meyer T, Howland HC. Department of Neurobiology and Behavior, W-201 Mudd Hall, Cornell University, Ithaca, NY 14853, USA. PURPOSE: To determine whether or not there are systematic differences in the areas of optic discs as measured by different machines using different measurement algorithms and whether racial or gender differences exist in optic disc area measurements. METHODS: We examined the results of 5 twenty-three published studies on the size of normal optic discs of various patient populations. Studies differed in the type of instrument and method used to measure optic disc area, and the number, age, race and gender of subjects examined. Noticing that different machines exhibited statistically significant systematic differences in optic disc sizes of comparable populations, we computed a "normalization" factor for each machine based on these mean differences. Applying this normalization factor to the results, we then re-examined the differences between racial and gender groups. RESULTS: By comparing the results of mean optic disc areas of different racial groups made with different machines, and normalizing results according to those of the Zeiss fundus camera, we found the normalization factors for the following machines to be, Zeiss fundus camera: 1 (by definition), Rodenstock Optic Disc Analyzer (RODA): 1.51, Topcon fundus camera: 1.04, Heidelberg Retina Tomograph (HRT): 1.15 and TopSS scanning laser ophthalmoscope: 1.29. That is, to bring the results of area measurements made with a RODA machine in line with those made with a Zeiss fundus camera, one should multiply the former by the factor 1.51. Using the normalized results, we confirmed the findings of previous authors that the optic disc areas of black subjects were statistically significantly larger than those of white subjects (n-weighted mean effect = 0.556 +/- 0.142 S.E., n = 5). Further, the meta-analysis of various racial populations from five studies shows that males have significantly larger discs than females (n-weighted mean effect = 0.151 +/- .055 S.E., n = 9). CONCLUSION: Different machines and techniques give different results when populations of similar racial composition are measured. We recommend applying the above normalizing factors when comparing studies that employ different instruments. Br J Ophthalmol 2001 Mar;85(3):297-303 Scanning laser ophthalmoscopy of the optic nerve head in exfoliation glaucoma and ocular hypertension with exfoliation syndrome. Harju M, Vesti E. Helsinki University Eye Hospital, PO Box 220, FIN-00029 HYKS, Finland. [email protected] AIMS: To study the relation between optic nerve head topography (Heidelberg retina tomograph, HRT) and disc area, visual field index mean defect (MD), and intraocular pressure (IOP), and to see whether change in HRT parameters is associated with change in MD in a prospective follow up. METHODS: 80 consecutive patients (69 patients with exfoliation glaucoma and 11 with ocular hypertension combined with exfoliation syndrome) were examined before IOP reducing intervention and prospectively followed every 6 months for 2 years. RESULTS: At the entry point, multiple regression analysis showed significant linear association between MD and all HRT parameters, when controlling for disc area. Disc area showed significant association with cup area, cup/disc area ratio, rim area, cup volume, and mean RNFL thickness. Six months after intervention IOP had decreased significantly. Reversible changes in cup area, cup/disc area ratio, rim area, cup volume, rim volume, mean cup depth, and maximum cup depth were associated with decrease in IOP. During the follow up period from 6 month to 2 years, IOP did not change significantly, and MD was used as a measure of progression of glaucoma. During this period, only cup shape measure among HRT parameters showed significant association with subsequent change in MD. CONCLUSION: Disc area should be taken into account when using HRT to compare patients. Any effect of change in IOP should be also taken into account when using HRT in follow up. Cup shape measure is a promising indicator of progression of glaucomatous damage. Br J Ophthalmol 2001 Mar;85(3):297-303 Scanning laser ophthalmoscopy of the optic nerve head in exfoliation glaucoma and ocular hypertension with exfoliation syndrome. Harju M, Vesti E. Helsinki University Eye Hospital, PO Box 220, FIN-00029 HYKS, Finland. [email protected] 6 AIMS: To study the relation between optic nerve head topography (Heidelberg retina tomograph, HRT) and disc area, visual field index mean defect (MD), and intraocular pressure (IOP), and to see whether change in HRT parameters is associated with change in MD in a prospective follow up. METHODS: 80 consecutive patients (69 patients with exfoliation glaucoma and 11 with ocular hypertension combined with exfoliation syndrome) were examined before IOP reducing intervention and prospectively followed every 6 months for 2 years. RESULTS: At the entry point, multiple regression analysis showed significant linear association between MD and all HRT parameters, when controlling for disc area. Disc area showed significant association with cup area, cup/disc area ratio, rim area, cup volume, and mean RNFL thickness. Six months after intervention IOP had decreased significantly. Reversible changes in cup area, cup/disc area ratio, rim area, cup volume, rim volume, mean cup depth, and maximum cup depth were associated with decrease in IOP. During the follow up period from 6 month to 2 years, IOP did not change significantly, and MD was used as a measure of progression of glaucoma. During this period, only cup shape measure among HRT parameters showed significant association with subsequent change in MD. CONCLUSION: Disc area should be taken into account when using HRT to compare patients. Any effect of change in IOP should be also taken into account when using HRT in follow up. Cup shape measure is a promising indicator of progression of glaucomatous damage. Am J Ophthalmol 2001 Feb;131(2):216-222 Retinal nerve fiber layer evaluation in human immunodeficiency virus-positive patients. Plummer DJ, Bartsch DU, Azen SP, Max S, Sadun AA, Freeman WR. Shiley Eye Center, Department of Ophthalmology, School of Medicine, University of CaliforniaSan Diego, La Jolla, CA 92093-0946, USA. [email protected] PURPOSE: To determine the effect of human immunodeficiency virus (HIV) infection on topographic measures of the optic disk and the retinal nerve fiber layer. METHODS: A crosssectional study at the Acquired Immunodeficiency Syndrome (AIDS) Ocular Research Unit at the University of California, San Diego. Retinal nerve fiber layer thickness at the optic nerve head was evaluated using the Heidelberg Retinal Tomograph, a confocal scanning laser tomograph in 38 HIV-positive and 24 age-matched HIV-negative subjects. RESULTS: HIV-positive patients without CMV retinitis showed significant differences from HIV-negative normal controls in a number of measures of the retinal nerve fiber layer. This indicated a loss of retinal ganglion cells in HIVpositive patients without retinitis. HIV-positive patients with CMV retinitis were worse in most measurements than both HIV-negative controls and HIV-positive patients without CMV. CONCLUSIONS: Significant thinning of the retinal nerve fiber layer occurs in HIV-positive patients without infectious retinopathy, and there are further changes in the optic disk associated with CMV retinitis. Confocal scanning laser tomography may be of use in the diagnosis of early HIV-associated visual function loss. Ophthalmology 2000 Dec;107(12):2272-2277 Identifying early glaucomatous changes. Comparison between expert clinical assessment of optic disc photographs and confocal scanning ophthalmoscopy. Wollstein G, Garway-Heath DF, Fontana L, Hitchings RA. Glaucoma Unit, Moorfields Eye Hospital, London, UK. Department of Ophthalmology, Shaare Zedek Medical Center, Jerusalem, Israel. OBJECTIVE: To compare the ability of expert clinicians, using qualitative assessment of stereoscopic optic disc photographs, and confocal scanning laser ophthalmoscope imaging to discriminate between healthy persons and patients with early glaucoma. DESIGN: Comparative 7 instrument validation study. PARTICIPANTS: Seventy-two healthy persons and 51 patients with early glaucoma (average visual field mean deviation, -3.6 dB). Early glaucoma was defined as a history of ocular hypertension and a reproducible visual field defect scoring 5 or less in the Advanced Glaucoma Intervention Study classification, regardless of optic disc appearance. INTERVENTION: Stereoscopic optic nerve head (ONH) photography and Heidelberg Retina Tomograph (HRT) imaging, (Heidelberg Engineering GmbH, Dossenheim, Germany). MAIN OUTCOME MEASURES: Ability of clinical assessment of stereoscopic ONH photographs and analysis of HRT parameters, taking into account the optic disc size, to detect early glaucomatous optic disc changes. RESULTS: The specificity of the majority opinion of five observers to detect early glaucomatous optic disc changes was 94.4%, with a sensitivity of 70.6%. Using the HRT analysis, the specificity was 95.8% and the sensitivity was 84. 3%. CONCLUSIONS: Heidelberg Retina Tomograph image analysis that takes into account the optic disc size is more sensitive than clinical assessment of stereoscopic optic disc photographs in distinguishing between healthy persons and patients with early glaucoma. Ophthalmology 2000 Dec;107(12):2267-2271 Glaucomatous optic disc changes in the contralateral eye of unilateral normal pressure glaucoma patients. Wollstein G, Garway-Heath DF, Poinoosawmy D, Hitchings RA. Glaucoma Unit, Moorfields Eye Hospital, City Road, London, UK. OBJECTIVE: To evaluate the optic disc for structural abnormalities in the contralateral eye of unilateral normal pressure glaucoma patients. DESIGN: Cross-sectional study. PARTICIPANTS: Fifty-three unilateral normal pressure glaucoma patients. TESTING: Optic disc imaging with the Heidelberg Retina Tomograph (HRT). MAIN OUTCOME MEASURES: Optic disc structural parameters. RESULTS: Of the contralateral (normal visual field) eyes, 79.2% were found to have an abnormal optic disc by HRT analysis. Of the glaucomatous (abnormal visual field) eyes, 94.3% were found to have an abnormal disc. The patterns of disc abnormality were defined as marked or moderate diffuse thinning of the neuroretinal rim (NRR) or broad or narrow focal thinning of the NRR. The most common pattern in the contralateral eyes was moderate diffuse thinning of the NRR (45.2%). The most frequently abnormal segments were the nasal superior (73. 8%) followed by the nasal inferior and the global NRR parameter (both 54.8%). CONCLUSIONS: A high frequency of NRR thinning was found in the contralateral (normal visual field) eyes of unilateral normal pressure glaucoma patients by HRT analysis. Knowing whether these abnormalities predict future progression to the development of visual field abnormality must wait until longitudinal studies are completed. If a disc abnormality is shown to predict future field loss, then early identification will allow early treatment. Graefes Arch Clin Exp Ophthalmol 2000 Sep;238(9):746-751 Three-dimensional analysis of measurements of the Heidelberg Retina Tomograph. Muller-Richter UD, Malig HJ, Schwerdtner A, Lang M, Hille K, Ruprecht KW. Augenklinik und Poliklinik der Universitat des Saarlandes, Homburg, Germany. BACKGROUND: With the aid of scanning laser tomography, feasible with the Heidelberg Retina Tomograph (HRT), refined structures can be measured three-dimensionally. Pictures are built up from scanned layers which are represented as two-dimensional topographical or reflectivity pictures by the HRT software. The kind of information that is provided by the third dimension can be exploited much better by real spatial three-dimensional presentation. The autostereoscopic Dresden 3D display makes such a spatial presentation feasible as add-on to the HRT. METHODS: Seventeen patients (9 women, 8 men) were chosen on the basis of a long duration of observation (mean 42.41 8 months) and a large number of follow-up examinations (mean 5.29). These patients were examined with the HRT as well as with the Dresden 3D display. The results were compared regarding their correlation pairs. RESULTS: Comparing the correlation pairs (r>0.7) the Dresden 3D display provided a higher Pearson correlation coefficient with 8 out of 10 pairs. It was evident that the evaluations of the two devices referred to the same parallel structures. DISCUSSION: The Dresden 3D display facilitates, with its form of presentation, a better evaluation of the measurements of the HRT. More precise evaluation of retinal structures by virtue of the autostereoscopic display presents an improvement. Br J Ophthalmol 2000 Sep;84(9):993-998 Use of sequential Heidelberg retina tomograph images to identify changes at the optic disc in ocular hypertensive patients at risk of developing glaucoma. Kamal DS, Garway-Heath DF, Hitchings RA, Fitzke FW. Glaucoma Unit, Moorfields Eye Hospital, London EC1V 2PD. AIM: To determine if global and segmental changes in optic disc parameters of sequential Heidelberg retina tomograph (HRT) images develop in individual ocular hypertensive (OHT) patients without white on white visual field defects. METHODS: Patients and normal controls were recruited from a prospective ocular hypertension treatment trial. The subject groups consisted of 21 OHT patients who had converted to early glaucoma on the basis of visual field criteria (24-2 program on the Humphrey perimeter), 164 OHT subjects with normal visual fields, and 21 normal controls. Sequential HRT images 16-21 months apart were obtained for each subject and segmental optic disc parameters were measured to determine if any change had occurred. From the analysis of sequential HRT images of the 21 normal eyes we established normal limits of interimage variation. Individual discs in each group showing changes above the 95% limit of normal variability were then sought. RESULTS: Several segmental and global optic disc parameters were found to show significant change in the converter group before confirmed visual field change, confirming our previously published results. Individual optic disc analysis using the 95% limit of normal variability data demonstrated glaucomatous change in 13 out of 21 converter eyes. 47 of the 164 OHT eyes with normal visual fields showed change in global and segmental parameters in a "glaucomatous" direction above the level expected for normal variability. The parameters which changed most frequently in the OHT eyes were: global cup volume (6.7% of discs), inferonasal cup volume (11%), inferotemporal cup volume (8.5%), and superotemporal cup area (7.3%). CONCLUSIONS: We have identified change in a subset of ocular hypertensive patients which could predate the development of glaucomatous visual field loss. The HRT could be of value in the sequential follow up of those suspected of having glaucoma by identifying eyes at risk of developing glaucoma. However, further refinement of the technique is required to eliminate some of the inherent variability of the analysis method described, and to increase the ability to detect at risk individuals. Am J Ophthalmol 2000 Sep;130(3):280-286 Optic disk topography after medical treatment to reduce intraocular pressure. Bowd C, Weinreb RN, Lee B, Emdadi A, Zangwill LM. Glaucoma Center and Diagnostic Imaging Laboratory, Department of Ophthalmology, University of California, San Diego, La Jolla, PURPOSE: We examined changes in optic disk topography using confocal scanning laser ophthalmoscopy after reducing intraocular pressure with administration of latanoprost. METHODS: Twenty-nine patients with glaucoma or ocular hypertension were imaged using the Heidelberg Retina Tomograph before and after the administration of latanoprost to decrease intraocular pressure. Average time between pretreatment and posttreatment imaging was 2.7 +/- 1.8 weeks. 9 Heidelberg Retina Tomograph software-measured parameters were mean height of contour, cup area, cup volume, mean cup depth, maximum cup depth, cup shape, rim area, rim volume, cup-todisk ratio, and retinal nerve fiber thickness. RESULTS: Average intraocular pressure decreased significantly (mean +/- SD) by 7.2 +/- 5.4 mm Hg (25 +/- 16% decrease). No statistically significant changes in measured topographic parameters were found. When data from patients with decreases in intraocular pressure of 7 mm Hg or greater were analyzed separately (mean intraocular pressure decrease = 10.79 +/- 4.32 mm Hg, 36 +/- 8% decrease), cup area (P =.005), cup volume (P =. 002), and cup-to-disk ratio (P =.005) decreased significantly, and rim area (P =.005) increased significantly. Linear regression analysis of the data from all subjects showed that a change in intraocular pressure after latanoprost administration accounted for 12% or more of the variance in two measured topographic parameters (mean cup depth and cup shape). CONCLUSIONS: These results suggest that, in some patients, moderate decreases in intraocular pressure may affect disk topography, as measured by Heidelberg Retina Tomograph. Intraocular pressure should be considered when analyzing consecutive confocal scanning laser ophthalmoscopy images for glaucomatous progression. Klin Monatsbl Augenheilkd 2000 Aug;217(2):82-87 Monitoring of morphometric changes of optic discs with morphologic progression of glaucomatous optic atrophy by means of laser scanner tomography. Mardin CY, Horn F, Budde WM, Jonas JB. Augenklinik mit Poliklinik der Universitat Erlangen-Nurnberg. [email protected] AIM: Aim of this study was to measure morphometric changes in optic discs with laser-scanning tomography (HRT, Heidelberg-Retina-Tomograph, Heidelberg) in eyes with early glaucomatous morphologic progression. PATIENTS AND METHODS: 61 eyes of 36 patients with marked neuroretinal rim loss or its early morphologic signs (1. optic disc hemorrhages, 2. reduced visibility of the retinal nerve fiber layer (RNF), 3. appearance of narrowing of retinal vessels, 4. enlargement of the choroidal, parapapillary atrophy) were compared to 74 normal eyes of 39 probands. 15 degrees stereographs of the optic discs were evaluated for morphologic changes. The morphometric variables of the neuroretinal rim and excavation measured by the HRT were examined in the course of the disease. RESULTS: In the group of normals no significant changes of the neuroretinal rim in the course of 2.0 +/- 1.2 years were found. In the group of glaucomatous eyes (3.0 +/- 1.5 years follow-up) 34 eyes showed marked neuroretinal rim loss, 17 disc hemorrhages, 4 vessel narrowing, 3 an increased chorioidal atrophy, 3 a decreased visibility of the retinal nerve fiber layer. In these eyes a significant loss of rim area (p = 0.01) and an increase of excavation area (p = 0.0001) and volume (p = 0.003) was measured by the HRT. Only three eyes showed a perimetric loss of sensitivity (0.8-3.4 db) in Octopus static perimetry. CONCLUSIONS: Laser-scanning tomography of the optic disc seems to be able to measure morphometric changes in eyes with morphologic progression of glaucomatous optic atrophy, even before perimetric changes occur. Graefes Arch Clin Exp Ophthalmol 2000 Aug;238(8):669-676 Measurement of a novel optic disc topographic parameter, "spikiness", in glaucoma. Morgan-Davies J, King AJ, Aspinall P, O'Brien CJ. Visual Impairment Research Group, Heriot Watt University, Edinburgh, Scotland, UK. BACKGROUND: Structural changes in the lamina cribrosa have been implicated in the pathogenesis of glaucomatous optic atrophy, but not observed. This paper presents a novel parameter of topographic variability within the optic disc, termed "spikiness", which may reflect glaucoma-related changes in the lamina. METHODS: Four age-matched groups of normal patients 10 (n=12, mean age 64.8 years) and patients with ocular hypertension (n=14, mean age 63.1), primary open-angle glaucoma (n=11, mean age 70) and low-tension glaucoma (n=15, mean age 66.3) were recruited. Images of normal and glaucomatous eyes from the Heidelberg Retina Tomograph were imported into ERDAS image processing software where the spikiness data (30 consecutive mean surface height values across the base of the optic cup in both the vertical and horizontal meridians) were extracted in a format that facilitated further statistical analysis. RESULTS: Significant differences in topographic variability (spikiness) existed in the vertical (F=3.64, P=0.01) but not the horizontal meridian (F=1.25, P=0.3) through the optic disc. Spikiness was inversely related to Humphrey mean deviation (P<0.05), and cup-disc ratio (P<0.004) and was directly related to nerve fibre layer thickness (P<0.005). Of particular interest was the finding that the spikiness measure was the only optic disc parameter to significantly discriminate low tension glaucoma from primary open angle glaucoma. CONCLUSION: A new measure of surface variability (topography) at the floor of the optic cup has been described. The new index of spikiness may represent a measurement of lamina cribrosa fragility which has been implicated, but not previously estimated, in glaucomatous eyes. Automated analysis of normal and glaucomatous optic nerve head topography images. Swindale_NV; Stjepanovic_G; Chin_A; Mikelberg_FS Invest Ophthalmol Vis Sci, 2000 06, 41: 7, 1730-42 PURPOSE: To classify images of optic nerve head (ONH) topography obtained by scanning laser ophthalmoscopy as normal or glaucomatous without prior manual outlining of the optic disc. METHODS: The shape of the ONH was modeled by a smooth two-dimensional surface with a shape described by 10 free parameters. Parameters were adjusted by least-squares fitting to give the best fit of the model to the image. These parameters, plus others derived from the image using the model as a basis, were used to discriminate between normal and abnormal images. The method was tested by applying it to ONH topography images, obtained with the Heidelberg Retina Tomograph, from 100 normal volunteers and 100 patients with glaucomatous visual field damage. RESULTS: Many of the parameters derived from the fits differed significantly between normal and glaucomatous ONH images. They included the degree of surface curvature of the disc region surrounding the cup, the steepness of the cup walls, the goodness-of-fit of the model to the image in the cup region, and measures of cup width and cup depth. The statistics of the parameters were analyzed and were used to construct a classifier that gave the probability, P(G), that each image came from the glaucoma population. Images were classified as abnormal if P(G) > 0.5. The probabilities assigned to each image were in most cases close to 0 (normal) or 1 (abnormal). Eightyseven percent of the sample was confidently classified with P(G) < 0.3 or P(G) > 0.7. Within this group, the overall classification accuracy was 92%. The overall accuracy of the method (the mean of sensitivity and specificity, which were similar) in the whole sample was 89%. CONCLUSIONS: ONH images can be classified objectively and dependably by an automated procedure that does not require prior manual outlining of disc boundaries. Graefes Arch Clin Exp Ophthalmol 2000 Jun;238(6):477-481 Search for an optimal combination of structural and functional parameters for the diagnosis of glaucoma. Multivariate analysis of confocal scanning laser tomograph, blue-on-yellow visual field and retinal nerve fiber layer data. Vihanninjoki K, Teesalu P, Burk RO, Laara E, Tuulonen A, Airaksinen PJ. Department of Ophthalmology, University of Oulu, Finland. BACKGROUND: The purpose of this study was to evaluate which of the structural and functional parameters--the Heidelberg Retina Tomograph (HRT), white-on-white (W/W) and blue-on-yellow 11 (B/Y) visual fields and semiquantitative retinal nerve fiber layer (RNFL) scoring parameters--can give the best separation between non-glaucomatous and glaucomatous eyes. METHODS: Fifty-five subjects were included in this study: 32 nonglaucomatous subjects with mean age of 54 years, and 23 patients with ocular hypertension or glaucoma and mean age of 59 years. The HRT with software 1.11, the Humphrey 30-2 W/W and lens coloration-corrected B/Y visual fields, and semiquantitative RNFL scores were utilized. Stepwise logistic regression analysis was used in finding, from a given set of parameters, a best discriminating parsimonious subset to a logistic model, the discriminatory performance of which was evaluated by the area under the ROC curve. RESULTS: When all the structural and functional variables were considered, the RNFL total overall score gave the best separation between glaucomatous and non-glaucomatous eyes (ROC area 0.98). Without the RNFL scores and optic disc size-dependent HRT parameters in the model, the cup shape measure was selected first (ROC area 0.88). In the second step the RNFL thickness was selected (ROC area 0.91), and in the third step the corrected B/Y mean deviation (MD) was selected (ROC area 0.91). With only the HRT parameters in the model, the cup/disc ratio was selected first (ROC area 0.88). However, when the groups were matched for optic disc size, all disc size-dependent HRT variables lost their discriminant power. CONCLUSION: Cup shape measure and RNFL thickness, together with age- and lens coloration-corrected MD of the B/Y perimetry provided good discrimination between healthy individuals and patients with glaucoma. Graefes Arch Clin Exp Ophthalmol 2000 May;238(5):375-384 Development of the standard reference plane for the Heidelberg retina tomograph. Burk RO, Vihanninjoki K, Bartke T, Tuulonen A, Airaksinen PJ, Volcker HE, Konig JM. Department of Ophthalmology, University of Heidelberg, Germany. [email protected] BACKGROUND: Topometry of the optic disc is the quantitative assessment of the structure of the optic nerve head by means of three-dimensional parameters. The parameter values depend on definitions of intraocular reference planes. PURPOSE: To describe the development of intraocular reference planes in laser scanning tomography for the Heidelberg Retina Tomograph (HRT) using image intrinsic data with a fixed offset reference plane (320 microm) and to present a contour-linebased "flexible" standard reference plane ("SRP") for calculation of intrapapillary stereometric parameters taking the interindividual variability of optic disc topography into account. METHODS: Ten-degree triple images were obtained by laser scanning tomography from 99 glaucoma eyes and 180 normal eyes. The images were evaluated to assess the variability of height measurements of an optic disc border contour-line segment (6 degrees width) corresponding to the site of the papillomacular bundle as indicated by the average optic disc surface inclination angle. RESULTS: The average optic disc surface inclination angle was -7 degrees +/- 3 degrees below the horizontal meridian (0 degrees). The 6 degrees wide contour-line segment for the SRP was chosen according to the average surface inclination angle (-10 degrees to -4 degrees). The reproducibility of the SRPsegment height measurements was 16.0+/-10.8 microm for normal eyes and 23.4+/-18.0 microm for glaucoma eyes. To ensure that the automatic reference level determination for intrapapillary parameters remained below the disc border height, we defined the SRP level at a 50 microm offset (>2 SD of average segment height reproducibility in glaucoma) added to the individual height position of the 6 degrees contour line segment. CONCLUSION: The flexible standard reference plane allows for automatic determination of intrapapillary variables once a disc border contour line is interactively defined. In contrast to a fixed offset reference plane (e.g. 320 microm below the mean retina height), the interindividual variability of optic disc topography (oblique insertion, glaucomatous surface flattening) is respected at the cost of the need for an accurate optic disc border outline. 12 Measurement of peripapillary retinal nerve fiber layer volume in glaucoma. King_AJ; Bolton_N; Aspinall_P; OBrien_CJ Am J Ophthalmol, 2000 05, 129: 5, 599-607 PURPOSE: To measure peripapillary retinal nerve fiber layer volume in normal subjects and patients with ocular hypertension, primary open-angle glaucoma, and low-tension glaucoma. METHODS: Sixty-five subjects were classified into four groups of normal subjects and subjects with ocular hypertension, primary open-angle glaucoma, and low-tension glaucoma on the basis of intraocular pressure measurements, visual field loss, and optic disk appearance. Groups were matched for sex, age, and optic disk area. Peripapillary retinal nerve fiber layer volume measurements were made with a modification of software version 1.11 of the Heidelberg Retina Tomograph confocal scanning laser ophthalmoscope. Retinal nerve fiber layer volume measurements were taken at 0.1-mm increments from the disk margin for a global 360-degree assessment and at four predefined segments using two different reference planes. Statistical analysis was carried out using analysis of variance with Bonferroni correction. RESULTS: Retinal nerve fiber layer volume measurements showed a gradation from normal to ocular hypertension and from ocular hypertension to glaucoma groups. Mean group measurements showed statistically significant differences (P <.05) in peripapillary retinal nerve fiber layer volume for most segmental measures between the groups. Measurements with the default reference plane in the 0.0-mm to 0.1-mm and 0.1-mm to 0.2-mm increments for the superotemporal segment showed the greatest differences between groups (P <.00005). CONCLUSION: Peripapillary retinal nerve fiber layer volume measurements differ between groups of normal subjects and patients with ocular hypertension, primary open-angle glaucoma, and low-tension glaucoma. This measure offers a further method of assessment of retinal nerve fiber layer in patients with glaucoma and glaucoma suspects. Am J Ophthalmol 2000 May;129(5):592-598 Relationship between structural abnormalities and short-wavelength perimetric defects in eyes at risk of glaucoma. Ugurlu S, Hoffman D, Garway-Heath DF, Caprioli J. Glaucoma Division, Jules Stein Eye Institute, UCLA School of Medicine, Los Angeles, California, USA. PURPOSE: To determine the relative prevalence of blue-yellow perimetric defects and structural abnormalities of the optic nerve and nerve fiber layer in eyes at risk of glaucoma. METHODS: Seventy-two eyes (of 72 patients) at risk of glaucoma, with normal white-on-white full threshold perimetry, were examined prospectively with blue-yellow full-threshold perimetry (Humphrey). Structural evaluations were conducted with qualitative assessment of stereoscopic color optic disk photographs and monochromatic nerve fiber layer photographs performed independently by three masked examiners (a glaucoma specialist and two glaucoma fellows), and statistical analysis of summary parameters was obtained with scanning confocal laser tomography (abnormal defined as values outside 95% confidence limits established in normal control subjects). RESULTS: Kappa values for interobserver agreement were 0.64, 0.88, and 0.79 for optic disk evaluation and 0.59, 0.60, and 0.61 for nerve fiber layer evaluation. Thirteen (18%) of 72 eyes had blue-yellow abnormalities. A total of 30 eyes (42%) were identified as having a structural abnormality; 29 (40%) had qualitatively determined optic disk abnormalities, 21 (29%) had qualitatively determined nerve fiber layer defects, and 26 (36%) had statistically significant structural abnormalities. Twelve of 13 eyes with blue-yellow defects had a detectable structural abnormality; all 12 had abnormalities identified with disk photography, nine with nerve fiber layer photography, and 12 by scanning laser tomography. CONCLUSIONS: Clinically detectable structural abnormalities frequently coexist with blue-yellow perimetric defects in patients with ocular hypertension. A 13 substantial proportion of patients with ocular hypertension with normal blue-yellow perimetry has early detectable glaucomatous structural abnormalities. Comparison of ranked segment analysis (RSA) and cup to disc ratio in computer-assisted optic disc evaluation. Gundersen_KG; Asman_P Acta Ophthalmol Scand, 2000 04, 78: 2, 137-41 PURPOSE: Ranked segment analysis is a new method for evaluation of optic nerve head topography with the Heidelberg Retina Tomograph. This analysis ranks sector measurements around the optic disc and compares these measurements with rank specific significance limits. We evaluated the diagnostic precision of the ranked segment analysis in a large clinical sample and compared with vertical cup/disc ratio measurements. Vertical cup/disc ratio measurements were not corrected for disc size. METHODS: We analysed optic disc images from 153 normal and 75 glaucomatous eyes using the Heidelberg Retina Tomograph (software version 2.01). Ranked segment analyses and vertical cup/disc ratio measurements were obtained from each optic disc image, and ROC curves were plotted. RESULTS: At the 95% specificity level, sensitivity was significantly lower for ranked segment analysis (70%) compared to vertical cup/disc ratio measurements (85%). Almost 30% of the discs in the glaucoma group were classified as normal using the ranked segment analysis. DISCUSSION: Ranked segment analysis yielded unacceptably poor discrimination, in fact, worse than cup/disc ratio with its known clinical limitations Glaucomatous disc damage typically occurs at the vertical poles of the disc. High rank measurements (low sector values) in normal eyes, on the other hand, are more common in the temporal disc sectors. Important spatial information is lost during the ranking procedure. This may partly explain the low sensitivity of the ranked segment analysis observed in our study. The results raise serious concerns regarding the clinical usefulness of ranked segment analysis. Curr Eye Res 2000 Apr;20(4):276-282 Interocular differences in optic disc topographic parameters in normal subjects. Gherghel D, Orgul S, Prunte C, Gugleta K, Lubeck P, Gekkieva M, Flammer J. University Eye Clinic Basel, Basel, Switzerland. PURPOSE: To test the interocular differences in optic disc topography in normal subjects by means of confocal scanning laser ophthalmoscopy. METHODS: Topographic measurements of the optic disc were evaluated by means of confocal scanning laser ophthalmoscopy (Heidelberg Retina Tomograph) in 314 eyes of 157 healthy volunteers. The examination was started randomly either with the right eye or the left eye. Differences between right and left eyes in disc area, cup area, cup volume, cup/disc area ratio, rim area, rim volume, maximum cup depth, cup shape measure, retinal nerve fiber layer thickness, and retinal nerve fiber cross section area for 360 degrees and for the temporal and nasal regions of the optic nerve head were evaluated by means of Student t-test. The same parameters were assessed in a subgroup of 80 elderly (age> 50 years) healthy subjects. Holm's sequentially rejective method was used for significance correction of multiple comparisons. RESULTS: Significant interocular differences in the average retinal nerve fiber layer thickness (p = 0.0010) and retinal nerve fiber layer cross section area (p = 0.0036) were found, with the right eye showing, on the average, lower values.The left eye showed a larger retinal nerve fiber layer thickness in 94 subjects (59.87%) and a larger retinal nerve fiber cross section area in 101 subjects (64. 33%). In the temporal optic disc area there were no statistically significant differences in topometric data (p> 0.05). In the nasal area, significant interocular differences in the retinal nerve fiber layer thickness (p = 0.0002) and retinal nerve fiber layer cross section area (p = 0.0003) were found. Similar results were found when the group of subjects older than 50 years was considered. 14 CONCLUSIONS: This study demonstrates systematic interocular differences in optic disc topometric data. Such a finding, be it due to methodological or biological reasons, should be taken in consideration in clinical trials. Technique for detecting serial topographic changes in the optic disc and peripapillary retina using scanning laser tomography. Chauhan_BC; Blanchard_JW; Hamilton_DC; LeBlanc_RP Invest Ophthalmol Vis Sci, 2000 03, 41: 3, 775-82 PURPOSE: To describe and evaluate a new statistical technique for detecting topographic changes in the optic disc and peripapillary retina measured with confocal scanning laser tomography. METHODS: The 256x256-pixel array of topographic height values obtained with each image from the Heidelberg Retina Tomograph (Heidelberg Engineering, Heidelberg, Germany) was divided into an array of 64x64 superpixels, where each superpixel contained 16 (i.e., 4x4) pixels. An analysis of variance technique was developed to analyze each superpixel with three baseline and three follow-up images. The performance of the technique was tested with and without adjustment for spatial correlation of topographic values using computer simulations and with real data from a normal control subject and a patient with progressive glaucomatous disc change. RESULTS: Computer simulation with fixed population means and variance, and varying spatial correlation showed a monotonically increasing number of superpixels with significant test results (false positives), with 20% false-positives when the spatial correlation was 0.8 (the approximate median value in real patient data). The number of false-positive results was similar (17%) in serial images of a normal subject. When corrected for spatial correlation, the number of false-positives was independent of the level of spatial correlation and remained at the expected value of less than 5% in both simulations and real data. Although the number of significant test results in the patient with progressive glaucoma decreased after correction for spatial correlation, the change was readily apparent. Statistical power to detect mean differences in topographic values ranging from 0.5 to 4.0 SDs in computer simulation showed low power for changes of 1 SD or less, but increased dramatically with larger changes. CONCLUSIONS: This technique has a high level of sensitivity to detect changes in the optic disc while maintaining a high level of specificity. Am J Ophthalmol 2000 Feb;129(2):129-135 Optical coherence tomography and scanning laser polarimetry in normal, ocular hypertensive, and glaucomatous eyes. Hoh ST, Greenfield DS, Mistlberger A, Liebmann JM, Ishikawa H, Ritch R. Department of Ophthalmology, The New York Eye and Ear Infirmary, New York, New York, USA. PURPOSE: To evaluate the relationship between visual function and retinal nerve fiber layer measurements obtained with scanning laser polarimetry and optical coherence tomography in a masked, prospective trial. METHODS: Consecutive normal, ocular hypertensive, and glaucomatous subjects who met inclusion and exclusion criteria were evaluated. Complete ophthalmologic examination, disk photography, scanning laser polarimetry, optical coherence tomography, and automated achromatic perimetry were performed. RESULTS: Seventy-eight eyes of 78 patients (17 normal, 23 ocular hypertensive, and 38 glaucomatous) were enrolled (mean age, 56.8+/-11.5 years; range, 26 to 75 years). Eyes with glaucoma had significantly greater neural network scores on scanning laser polarimetry and lower maximum modulation, ellipse modulation, and mean retinal nerve fiber layer thickness measured with optical coherence tomography compared with normal and ocular hypertensive eyes, respectively (all P<.005). Significant associations were observed between neural network number (r = -.51, r = .03), maximum modulation (r = .39, r = -.32), ellipse 15 modulation (r = .36, r = -.28), and optical coherence tomography-generated retinal nerve fiber layer thickness (r = .68, r = -.59) and visual field mean deviation and corrected pattern standard deviation, respectively. All scanning laser polarimetry parameters were significantly associated with optical coherence tomography-generated retinal nerve fiber layer thickness. CONCLUSION: Optical coherence tomography and scanning laser polarimetry were capable of differentiating glaucomatous from nonglaucomatous populations in this cohort; however considerable measurement overlap was observed among normal, ocular hypertensive, and glaucomatous eyes. Retinal nerve fiber layer structural measurements demonstrated good correlation with visual function, and retinal nerve fiber layer thickness by optical coherence tomography correlated with retardation measurements by scanning laser polarimetry. Acta Ophthalmol Scand 2000 Feb;78(1):9-13 Comparability of three-dimensional optic disc imaging with different techniques. A study with confocal scanning laser tomography and raster tomography. Gundersen KG, Heijl A, Bengtsson B. Department of Ophthalmology, Malmo University Hospital, Sweden. [email protected] PURPOSE: We wanted to compare optic nerve head topography measurements and discrimination between normal and glaucomatous eyes with two entirely different three-dimensional optic disc imaging techniques, confocal scanning laser tomography (Heidelberg Retina Tomograph, Heidelberg Engineering) and raster tomography (Glaucoma-Scope, Ophthalmic Imaging Systems). METHODS: Both eyes of 225 normal subjects and 229 eyes of 166 patients with glaucoma at different stages were imaged with the Heidelberg Retina Tomograph and the Glaucoma-Scope. Optics discs were analysed in 15 degrees sectors around the circumference. Depth measurements were calibrated on objects with known dimensions. RESULTS: We observed no significant differences in absolute measurements of maximum cup depth and cup area between the two instruments. We observed small differences in absolute measurements of disc anti rim area between the two instruments. Discrimination between normal and glaucomatous eyes was close to identical for the two instruments. Both instruments had the same ability to distinguish glaucomatous regional alterations of optic nerve head topography from normal disc configuration. CONCLUSION: Both instruments while using entirely different principles for three-dimensional optic disc imaging gave very similar results. This correspondence of results implies that the same optic disc parameters can be analysed, and the results interpreted similarly for both methods, and probably with other threedimensional imaging instruments. It may also indicate that results of studies with one of the instruments have general validity. Concordance between results of optic disc tomography and high-pass resolution perimetry in glaucoma. Martin_LM; Lindblom_B; Gedda_UK J Glaucoma, 2000 02, 9: 1, 28-33 PURPOSE: To evaluate concordance between results obtained with the Heidelberg Retina Tomograph (HRT) (Heidelberg Engineering GmbH, Heidelberg, Germany) and those obtained with the high-pass resolution perimeter (HRP) in glaucoma diagnosis. METHODS: A total of 217 patients from the glaucoma services at St. Erik Eye Hospital, Stockholm, Sweden (n = 107) and Sahlgrenska University Hospital, Göteborg, Sweden (n = 110) were included in the study. All patients were examined because of known or suspected glaucoma in at least one eye. The conventional indices presented by the instruments were used, i.e., glaucoma index from the HRT (negative values = abnormal, positive = normal) and combined deviation (upper normal limit 2.1 dB) from the HRP. RESULTS: The concordance regarding the classification of normal or 16 glaucomatous by the two instruments was 71% (153/217 eyes). The HRT indicated glaucoma but HRP findings were normal in 47 patients, and the reverse occurred in 17 patients. There was a significant difference in optic disc area between patients with abnormal HRT findings and normal HRP findings and in patients with normal HRT findings and abnormal HRP findings. The concordance could not be improved by adjusting for disc size. The correlation between combined deviation on HRP and the HRT glaucoma index was r = -0.53. CONCLUSION: A significant correlation was found between the combined index given by HRP and the HRT glaucoma index in 217 patients examined for known or suspected glaucoma. Discordant findings were observed in 64 patients; in 22 this discordance was explained by the influence of disc size. No other reasons for differences in examination results could be detected. Surv Ophthalmol 1999 Oct;44:S41-S53 Quantitative morphologic and functional evaluation of the optic nerve head in chronic openangle glaucoma. Bartz-Schmidt KU, Thumann G, Jonescu-Cuypers CP, Krieglstein GK. Department of Ophthalmology, University of Cologne, Germany. [email protected] Glaucoma leads to morphologic changes of the optic nerve head and to functional defects. Morphologic changes in the three-dimensional surface structure of the optic nerve head at its entrance site into the globe can be examined by laser scanning tomography. The standard technique for evaluating functional defects in glaucoma is static computerized perimetry. We compared these two techniques to determine which is more sensitive for follow-up of glaucomatous damage of the optic nerve head. If decreased function is presumed to precede imminent cell death, visual field analysis should be the more sensitive method, as cell death results in absolute defects of the visual field. However, the neuronal networks do not necessarily function in this way. In the case of loss of individual elements in the neuronal network, the complex linkages, even at the retinal level, are able to maintain functions and compensate for loss of function, which means that visual field defects would not be prominent. If the damage increases with time and is accompanied by a progressive loss of ganglion cells, however, compensation is eventually no longer possible, and the functional defects then become measurable by visual field analysis. Thus, morphologic absolute changes may be more prominent than visual field defects in the early stages of glaucoma. To evaluate the quantitative relationship between morphometrically measurable defects of the optic nerve head and measurable functional defects, we first examined the visual field with static computerized perimetry and then evaluated the surface structure with a laser scanning tomograph in 90 patients with chronic open-angle glaucoma, 10 patients with ocular hypertension, and 10 patients without any eye disease. Based on the 95th percentile of the standardized rim/disk area ratio, we calculated the relative rim area loss and correlated this with the mean defect in visual field analysis. The scatterplot shows an exponential curve. In the early stages of glaucoma, visual field defects were less prominent than morphologic absolute changes; 40% of the neuroretinal rim area is lost by glaucomatous optic nerve damage before first defects in visual field analysis appear. In late stages of glaucoma, changes in perimetry are more prominent than those observed with biomorphometry. These results show that in the follow-up of patients with early stages of glaucomatous damage, special attention should be given to morphologic absolute changes. In patients with advanced glaucoma, progress of the damage should be observed by repeated functional, rather than morphologic, examinations. It is important to keep in mind, however, that the sensitivity of any method is dependent on technology. One reason why functional tests may not be as sensitive as morphologic examination in observing patients with early stages of glaucoma may simply be that functional tests are not yet sensitive enough to detect early damage. 17 Surv Ophthalmol 1999 Oct;44:S33-S40 Topographic analysis to discriminate glaucomatous from normal optic nerve heads with a confocal scanning laser: new optic disk analysis without any observer input. Iester M, De Ferrari R, Zanini M. Department of Neurological and Visual Sciences, Ophthalmology B, University Eye Clinic of Genoa, Italy. PURPOSE: We evaluated the potential ability of a confocal scanning laser ophthalmoscope to differentiate patients with normal visual fields from those with abnormal visual fields with an optic nerve head topographic map. PATIENTS AND METHODS: Twenty normal eyes with normal visual fields, intraocular pressures of less than 22 mm Hg, and no family history of glaucoma and 20 glaucomatous eyes with abnormal visual fields and open angles were selected. Glaucomatous eyes with advanced visual field damage were not included. One eye was chosen randomly from each patient. All eyes were examined with the Heidelberg Retina Tomograph (HRT [Heidelberg Engineering GMBH, Heidelberg, Germany]) and Humphrey Perimeter, program 30-2 (Humphrey Instruments, Inc., San Leandro, CA, USA). Topographic maps were analyzed with different methods based on contour lines, with use of a program able to differentiate glaucomatous from normal optic disks. Sensitivity, specificity, and diagnostic precision were calculated. RESULTS: The analysis had a sensitivity, specificity, and diagnostic precision of 80%, 100%, and 90%, respectively. CONCLUSION: With the topographic map data and this technique, the HRT's capacity to differentiate normal optic disks from glaucomatous disks was improved. In addition, with this method, we avoided any subjective observer input in drawing the optic nerve head outline. Ophthalmology 1999 Oct;106(10):2027-2032 Heidelberg retina tomography and optical coherence tomography in normal, ocularhypertensive, and glaucomatous eyes. Mistlberger A, Liebmann JM, Greenfield DS, Pons ME, Hoh ST, Ishikawa H, Ritch R. Department of Ophthalmology, The New York Eye and Ear Infirmary, New York 10003, USA. PURPOSE: To evaluate optic disc and retinal nerve fiber layer (RNFL) appearance in normal, ocular-hypertensive, and glaucomatous eyes undergoing confocal scanning laser ophthalmoscopy and optical coherence tomography (OCT). DESIGN: Prospective, cross-sectional study. PARTICIPANTS: Seventy-eight eyes of 78 consecutive normal (n = 17), ocular-hypertensive (n = 23), and glaucomatous subjects (n = 38) were enrolled. METHODS: Each patient underwent complete ophthalmic examination, achromatic automated perimetry, confocal scanning laser ophthalmoscopy (Heidelberg Retinal Tomography [HRT]), and OCT. Topographic HRT parameters (disc area, cup-disc ratio, rim area, rim volume, cup shape measure, mean RNFL thickness, and cross-sectional area) and mean OCT-generated RNFL thickness were evaluated in each group. MAIN OUTCOME MEASURES: OCT and HRT assessment of optic disc and RNFL anatomy. RESULTS: OCT RNFL thickness showed no difference between normal and ocular-hypertensive eyes (P = 0.15) but was significantly less in glaucomatous eyes (P < 0.001). HRT measurements of rim area, cup-disc ratio, cup shape measure, RNFL thickness, and RNFL cross-sectional area were significantly less in glaucomatous eyes (all P < 0.005) and were correlated with mean OCT RNFL thickness (all P < 0.02). RNFL thickness using OCT or HRT was highly correlated with visual field mean defect during achromatic perimetry (P < 0.0001). CONCLUSION: Both HRT and OCT can differentiate glaucomatous from nonglaucomatous eyes. RNFL thickness measurements using OCT correspond to disc topographic parameters using HRT. Jpn J Ophthalmol 1999 Sep;43(5):410-414 Scanning laser tomography to evaluate optic discs of normal eyes. 18 Nakamura H, Maeda T, Suzuki Y, Inoue Y. Eye Division of Olympia Medical Clinic, Tokyo, Japan. PURPOSE: To investigate the effects of age, eye refraction, and disc area on topographic parameters of the optic nerve head in normal volunteers, using the Heidelberg Retina Tomograph. METHODS: Seventy-seven eyes of 77 normal volunteers were examined by scanning laser tomography. The topographic parameters analyzed were disc area, cup area, cup/disc area ratio, rim area, cup volume, rim volume, mean cup depth, maximum cup depth, cup shape measure, height variation contour, mean retinal nerve fiber layer thickness (MnRNFLT), and retinal nerve fiber layer (RNFL) cross-section area. The effect of age, refraction, and disc area on each parameter was analyzed by the multiple linear regression model. RESULTS: Significant declines in MnRNFLT and RNFL cross-section area were found with increasing age (P < .05). The mean cup depth and maximum cup depth were significantly deeper in myopic subjects (P < .05). Large discs had large cup area, cup/disc area ratio, rim area, cup volume, mean cup depth, cup shape measure (P < .01), and maximum cup depth (P < .05). The MnRNFLT was smaller in large discs (P < .01). Rim volume was unaffected by age, refraction, or disc area. CONCLUSIONS: The age, refraction, and disc area were related to several optic disc parameters obtained by the Heidelberg Retina Tomograph. Because of these relationships, care should be taken to analyze the appearance of the optic disc on the basis of these parameters in patients with glaucoma or other diseases. Rim volume appears to be a good parameter for evaluating the optic disc without considering age, refraction, or disc area. Jpn J Ophthalmol 1999 Sep;43(5):392-397 Influence of myopic disc shape on the diagnostic precision of the Heidelberg Retina Tomograph. Yamazaki Y, Yoshikawa K, Kunimatsu S, Koseki N, Suzuki Y, Matsumoto S, Araie M. Department of Ophthalmology, Nihon University School of Medicine, Tokyo, Japan. PURPOSE: To investigate the diagnostic capability of a glaucoma diagnostic classification program for the Heidelberg Retina Tomograph (HRT) in eyes with myopic disc shapes. METHODS: Sixtysix normal subjects (66 eyes) and 78 open-angle glaucoma patients (78 eyes) were enrolled. The eyes were divided into two groups; those eyes with myopic and those with nonmyopic disc shapes. The classification was based on clinical judgment made after the examination of stereophotographs of the discs without considering the refractive errors. The agreement between the classification program and the clinical diagnosis was evaluated for sensitivity, specificity, and diagnostic precision. The influence of the disc shape on the HRT topographic parameters was evaluated. RESULTS: The sensitivity, specificity, and diagnostic precision of the HRT were 83%, 95%, and 89% in eyes with nonmyopic disc shapes, but 71%, 96%, and 83% in those with myopic disc shapes. Rim volume, height variation contour, mean retinal fiber nerve layer (RNFL) thickness, and RNFL cross-section area were significantly larger in eyes with myopic disc shapes than in eyes with nonmyopic discs, regardless of the clinical diagnosis. CONCLUSIONS: The classification program should be modified to take into account the myopic disc shape in order to improve its capability to make more accurate diagnosis of glaucoma possible. Klin Monatsbl Augenheilkd 1999 Sep;215(3):182-185 Initial clinical experiences with the Dresden 3D display in conjunction with the Heidelberg Retina Tomograph (HRT). Muller-Richter UD, Malig HJ, Schwerdtner A, Lang M, Hille K, Ruprecht KW. Augenklinik und Poliklinik, Universitat des Saarlandes, Homburg, Saar. 19 BACKGROUND: For years the Heidelberg Retina Tomograph has been an established method to diagnose early glaucomatous damages at the optic nerve head. The major difficulty consists in defining the outlayer of the optic nerve head in a 2-dimensional reflective or topographic picture. A 3-dimensional presentation of the ocular fundus could ease the defining very much. The Dresden 3D-display tested provides a true 3-dimensional presentation of the HRT-values measured. METHODS: For the study 5 groups of prediagnosed follow-up examinations were formed, which in their course showed various progression. The examination firstly was carried out by manual defining of the papilla contour on the Dresden 3D-display and secondly by the new automatic contour-finding of the 3D-software. RESULTS: Through the 3-dimensional presentation a more correct position of the contour can be found when drawn manually. As a result some diagnoses of the 2-dimensional HRT-pictures had to be revised. The results proved considerable differences between the automatic outlayer-finding and the probably real position of the papilla borders. CONCLUSION: The 3-dimensional presentation of the HRT-pictures represents an subjective improvement regarding the accuracy of manual contour definition. In particular, the fact that it is feasible to make the pictures rotate around the axes offers completely new insights to the morphology of the disc. Ophthalmology 1999 Sep;106(9):1751-1755 Optic disc topographic measurements after pupil dilation. Zangwill LM, Berry CC, Weinreb RN. Glaucoma Center and Diagnostic Imaging Laboratory, University of California San Diego, La Jolla 92093-0946, USA. [email protected] PURPOSE: To determine the effect of pupil dilation on topographic optic disc parameters measured with confocal scanning laser ophthalmoscopy. DESIGN: Prospective, comparative, observational case series. PARTICIPANTS: Thirty-eight subjects (25 glaucoma patients, 5 glaucoma suspects, and 8 normal subjects) representing a range of lens opacities participated in this study. METHODS: Topographic optic disc parameter measurements were obtained before and after pupil dilation with a confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph). Cataract severity was measured with the LOCS III grading system. Image quality was assessed using the standard deviation of the mean topography image and an image quality score. Multiple regression techniques were used to evaluate the effect of image quality, cataract density, and pupil size on the change in topographic parameters after dilation. MAIN OUTCOME MEASURES: Topographic optic disc parameter measurements. RESULTS: With dilation, mean change in most topographic optic disc parameters was not significantly different from zero. Changes in topographic optic nerve parameters tended to be relatively small when undilated images were of good quality and larger in images of relatively poor quality. The strongest predictor of the absolute value of change in topographic optic disc parameters was the standard deviation of the undilated mean topography image. CONCLUSIONS: When confocal scanning laser ophthalmoscope images are of good quality, topographic optic disc parameter measurements obtained with a dilated pupil are similar to those obtained with an undilated pupil. However, caution should be exercised when interpreting information from poor quality confocal scanning laser ophthalmoscopic images. Optom Vis Sci 1999 Aug;76(8):526-536 New technologies for diagnosing and monitoring glaucomatous optic neuropathy. Zangwill LM, Chang CF, Williams JM, Weinreb RN. Glaucoma Center and Diagnostic Imaging Laboratory, Department of Ophthalmology, University of California, San Diego, La Jolla, California 92093-0946, USA. 20 BACKGROUND: Recently, instruments have been developed to provide real-time, quantitative measurements of the optic disc and retinal nerve fiber layer (RNFL) for use in glaucoma management. Our objective is to (1) provide an overview of two of these instruments, the confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph, HRT) and scanning laser polarimeter (Nerve Fiber Analyzer, NFA) and (2) compare measurements obtained with these instruments to clinical features used in the diagnosis of glaucoma. METHODS: Twenty glaucoma patients, 4 normal subjects and 20 glaucoma subjects were included. All subjects had images obtained with the HRT and NFA, and RNFL and optic disc photography completed within 5 weeks of each other. The HRT results were compared with qualitative evaluation of stereophotographs of the optic disc, and NFA results were compared against a semi-quantitative RNFL photograph severity score. RESULTS: Twenty-five (57%) subjects had thinning of the neuroretinal rim identified by evaluation of stereoscopic optic disc photographs. Despite overlap, HRT measurements of rim volume, rim area, and rim/disc ratio were significantly smaller in eyes with evidence of rim thinning than in eyes with no evidence of rim thinning. Moderate to severe RNFL damage was detected by evaluation of photographs in 25 (57%) of subjects. NFA RNFL thickness measures were smaller in eyes with moderate to severe RNFL damage than in relatively healthy eyes. CONCLUSIONS: Previous studies have documented the reproducibility of these instruments and suggested analytic techniques for improving their ability to differentiate between normal and glaucoma eyes. Our results indicate that despite overlap in values, these instruments provide measurements that reflect clinically relevant features of the optic disc and RNFL. Whether these technologies can improve our ability to detect glaucomatous progression over time needs to be determined with well-designed longitudinal studies and comparison with established diagnostic techniques for evaluating glaucomatous optic neuropathy. Arch Ophthalmol 1999 Aug;117(8):1010-1013 Optic nerve head morphologic characteristics in high-tension and normal-tension glaucoma. Iester M, Mikelberg FS. Department of Ophthalmology, University of British Columbia, Vancouver, Canada. OBJECTIVES: To determine the morphometric parameters in high-tension glaucoma (HTG) and normal-tension glaucoma (NTG) with a confocal scanning laser ophthalmoscope, and to determine the relationship to disc size. METHODS: One hundred eighty-six patients with glaucoma were recruited for this study. For each patient, only one eye was randomly chosen. Patients with NTG and HTG were classified using untreated intraocular pressure (IOP) as the variable; the NTG group had IOP less than 22 mm Hg during a diurnal tension curve, while patients with HTG had IOP greater than 21 mm Hg in at least 3 measurements. All the patients were examined with Humphrey perimeter program 30-2 and a Heidelberg Retina Tomograph. Findings were assessed by t test. Patients were then divided by disc area size into 3 subgroups: small discs with an area less than 2 mm2, midsized discs with an area of 2 to 3 mm2, and large discs with an area greater than 3 mm2. RESULTS: One hundred thirty-two HTG eyes and 50 NTG eyes were assessed. Four eyes were excluded because they were classified as having secondary glaucoma. No significant differences were found between HTG and NTG eyes for any Heidelberg Retina Tomograph morphometric parameters, even when patients were divided into subgroups. CONCLUSION: No differences were apparent between HTG and NTG in morphometric parameters as measured by scanning laser ophthalmoscopy. Klin Monatsbl Augenheilkd 1999 Jun;214(6):378-385 Laser scanning topography and polarimetry with implantation of intraocular lenses before and after cataract surgery. Kremmer S, Pflug A, Heiligenhaus A, Fanihagh F, Steuhl KP. 21 Abteilung fur Erkrankungen der vorderen, Universitats-Augenklinik Essen. BACKGROUND: In the last years, scanning laser measurements were established in glaucoma diagnostics. Techniques of special interest are scanning laser topometry (SLT) for exact measurements of the optic disc and its cup and scanning laser polarimetry (SLP) for precise assessment of the retinal nerve fiber layer thickness. As glaucoma patients often suffer from a cataract, too, and a trabeculectomy additionally favors the advance of lens opacities, in the follow up of glaucoma patients cataract surgery is often necessary. PATIENTS AND METHODS: The influence of cataract surgery in phacotechnique with intraocular lens implantation (31 PMMAIOLs, Pharmacia/Upjohn, model 811 B, and 25 HEMA/MMA-IOLs, Technomed, Memory Lens) on SLT and SLP was evaluated before and 3 to 4 weeks after cataract surgery in 56 eyes of otherwise healthy patients. Lens opacities were classified according to LOCS III. For SLT, we applied a TopSS, and for SLP a Nerve Fiber Analyzer II and a GDx (LDT, USA). RESULTS: Our results show that SLT and SLP are mostly performable at lens opacities with visual acuity reductions down to 0.16. In SLT, we usually found no big differences in the assessed parameters before and after cataract surgeries with IOL implantation. Standard deviations between three single measurements were mostly smaller postop. In SLP, nerve fiber layer patterns were very similar before and after cataract surgeries with IOL implantation whereas total nerve fiber layer thickness values postoperatively were slightly higher. CONCLUSIONS: Our results indicate that cataract surgeries with IOL-implantation have only mild influence on SLT and SLP. These findings seem to be of clinical interest especially in the follow up of glaucoma patients. Ophthalmology 1999 Jun;106(6):1147-1151 Comment in: Ophthalmology. 2000 Mar;107(3):407 Longitudinal changes in optic disc topography of adult patients after trabeculectomy. Topouzis F, Peng F, Kotas-Neumann R, Garcia R, Sanguinet J, Yu F, Coleman AL. Jules Stein Eye Institute and Department of Ophthalmology, University of California Los Angeles, School of Medicine 90095-7004, USA. OBJECTIVE: To study longitudinal changes in optic disc topography after trabeculectomy in adult patients. DESIGN: Prospective case series. PARTICIPANTS: Twenty-five eyes of 25 patients undergoing trabeculectomy were enrolled. INTERVENTION: Images of the optic disc were obtained preoperatively and approximately 2 weeks, 4 months, and 8 months after surgery by use of a confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph). MAIN OUTCOME MEASURES: The topographic optic disc parameters (cup volume, cup area, rim volume, rim area, cup-disc area ratio, mean cup depth, maximum depth, cup shape, and height variation contour) were measured automatically for each image with the Heidelberg Retina Tomograph Software (version 1.11). RESULTS: Approximately 2 weeks after surgery, the mean preoperative intraocular pressure (IOP) of 19.3 mmHg (SD, 6.4 mmHg) decreased to 6.0 mmHg (SD, 3.6 mmHg), cup volume and mean cup depth decreased, height variation contour increased, and the cup shape parameter became more negative. Approximately 4 months after surgery, mean IOP was 9.7 mmHg (SD, 4.2 mmHg), and the only statistically significant change from preoperative values of optic disc parameters was in the cup shape measure. Approximately 8 months after surgery, there was no statistically significant change in any of the optic disc parameters compared with preoperative values, although IOP was 10.4 mmHg (SD, 5.9 mmHg). CONCLUSIONS: Changes in the optic disc that may be present 2 weeks after a trabeculectomy do not appear to persist 4 and 8 months later in eyes with advanced glaucomatous optic nerve damage, except for cup shape, which was different from preoperative values at 4 months but not at 8 months. Ophthalmology 1999 May;106(5):1013-1018 22 Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Lesk MR, Spaeth GL, Azuara-Blanco A, Araujo SV, Katz LJ, Terebuh AK, Wilson RP, Moster MR, Schmidt CM. William and Anna Goldberg Glaucoma Service, Wills Eye Hospital, Jefferson Medical College, Thomas Jefferson University, Philadelphia, Pennsylvania 19107-5598, USA. OBJECTIVE: To detect and quantitate changes in optic nerve morphology after glaucoma surgery using the Heidelberg Retina Tomograph (HRT, Heidelberg Instruments, Heidelberg, Germany). DESIGN: Nonconsecutive observational case series. PARTICIPANTS AND INTERVENTION: The authors prospectively enrolled 21 adult patients undergoing incisional glaucoma surgery for progressive glaucoma damage. Quantitative analysis of the optic nerve head by scanning laser tomography and automated perimetry were performed before and after glaucoma surgery. MAIN OUTCOME MEASURES: Changes in optic nerve parameters were subjected to linear regression analysis with respect to percent of postoperative reduction of intraocular pressure (IOP), as well as with respect to age, refraction, preoperative cup:disc ratio, and change in visual field parameters. RESULTS: Seventeen patients had pre- and postoperative images suitable for analysis. Mean IOP at the time of image acquisition before surgery was 30.5+/-12 mm Hg, and after surgery 11.8+/-5.2 mm Hg (mean follow-up, 26+/-7 weeks). Eleven of 13 (85%) patients having IOP reduction of greater than 40% showed improvement in optic disc parameters. All four patients with less than 25% reduction in IOP showed worsening of most parameters. Changes in optic disc parameters were highly correlated with percent IOP reduction and with age. The parameters in which change most strongly correlated with percent change of IOP were cup area, rim area, cup:disc ratio, and mean cup depth (each, P<0.005). The age of the patient correlated highly with change in maximum cup depth (P<0.005). Refraction and clinically determined cup:disc ratio correlated poorly with changes in measured optic disc parameters. Clinical improvement in visual fields was correlated with the degree of improvement of cup:disc ratio (P = 0.025). CONCLUSION: Most patients showing a 40% lowering of IOP after glaucoma surgery show improved optic nerve morphology as measured by the HRT. The amount of improvement correlated highly with the percent reduction of IOP. Ophthalmologica 1999;213(4):219-223 Asymmetry in intraocular pressure and retinal nerve fiber layer thickness in normal-tension glaucoma. Gugleta K, Orgul S, Flammer J. University Eye Clinic, Basel, Switzerland. The etiology of glaucoma is most probably multifactorial. This study intended to investigate the asymmetry in intraocular pressure (IOP) and that in retinal nerve fiber layer (RNFL) thickness in normal-tension glaucoma patients. Two diurnal tension curves, obtained within 3 months and counting at least five IOP readings each, including an early morning IOP measurement upon awaking, were obtained in 15 normal-tension glaucoma patients. None of the patients received IOPlowering therapy. IOP asymmetry was present in at least three readings and was always in the same direction. The optic nerve was imaged in both eyes in each patient by means of confocal scanning laser ophthalmoscopy (Heidelberg Retina Tomograph). The interocular difference in RNFL thickness and the RNFL cross-sectional area were correlated with the interocular difference in IOP by means of Spearman's rank correlation factor. Nine female and 6 male normal-tension glaucoma patients (mean +/- SD age was 62. 4 +/- 16.9 years) were included in this study. Interocular IOP asymmetry varied between 0.30 and 4 mm Hg. Strong negative correlations were found between interocular asymmetry in IOP and interocular asymmetry in RNFL thickness asymmetry (R = 0.652, p = 0. 0083) and interocular asymmetry in RNFL cross-sectional area (R = -0. 702, p = 23 0.0034). The present results demonstrate for the first time a more marked thinning of the neuroretinal nerve fiber layer in the eye with the higher IOP in normal-tension glaucoma patients. J Glaucoma 1999 Apr;8(2):99-104 Agreement in assessing glaucomatous discs in a clinical teaching setting with stereoscopic disc photographs, planimetry, and laser scanning tomography. Hatch WV, Trope GE, Buys YM, Macken P, Etchells EE, Flanagan JG. School of Optometry, University of Waterloo, Canada. PURPOSE: Agreement between three observers--two recently trained fellows and their supervisor-was measured using estimations of cup/disc ratio from stereoscopic optic nerve head photographs and planimetric measurements of cup/disc ratio. Agreement between the clinicians' planimetric measurements of cup/disc ratio and laser scanning tomographic measurements of cup/disc ratio also was assessed. METHODS: From 16 stereoscopic optic nerve head photographs of 16 subjects, the three observers performed clinical estimations of horizontal and vertical cup/disc ratios and planimetric measurements of cup/disc ratios. Interobserver agreement was measured using intraclass correlation coefficients (ICCs). Agreement between the planimetric cup/disc ratios and laser scanning tomographic cup/disc ratios obtained with the Heidelberg Retina Tomograph (HRT; Heidelberg Engineering, Heidelberg, Germany) also was measured using ICCs. The difference between the planimetric and HRT cup/disc ratios was calculated. RESULTS: The agreement between observers for clinical estimations from stereoscopic optic nerve head photographs (ICC = 0.74 horizontally and 0.83 vertically) was substantial. Agreement between the observers' planimetric measurements of cup/disc ratio was substantial (ICC = 0.79). Agreement between HRT cup/disc ratio and each observer's planimetric cup/disc ratio was moderate (ICC = 0.57-0.65), with large confidence intervals. The cup/disc ratio measured with HRT was an average of 0.07 to 0.11 larger than the planimetric cup/disc ratio. CONCLUSION: Substantial agreement between observers can be achieved when estimating cup/disc ratio with stereoscopic optic nerve head photographs and with planimetric measurements of cup/disc ratios, provided there is a standard protocol and sufficient training period. Good agreement is critical in a teaching institution to ensure accurate follow-up care of patients with glaucoma, especially if patients are examined by different clinicians. Laser scanning tomography is a more repeatable and objective method, which may provide further standardization of optic nerve head assessments. Future studies will determine the reference plane that optimizes agreement between the HRT findings and each clinician's estimations. J Glaucoma 1999 Apr;8(2):105-110 Agreement of measurement of parapapillary atrophy with confocal scanning laser ophthalmoscopy and planimetry of photographs. Kono Y, Jonas JB, Zangwill L, Berry CC, Weinreb RN. Glaucoma Center, University of California at San Diego, La Jolla 92093-0946, USA. PURPOSE: To evaluate whether parapapillary atrophy can be measured interactively using confocal scanning laser ophthalmoscopy. METHODS: For 36 patients with open-angle glaucoma or suspected of having glaucoma, confocal scanning laser ophthalmoscopy of the optic nerve head was performed using the Heidelberg Retina Tomograph (HRT; Heidelberg Engineering, Heidelberg, Germany). Alpha and beta zones of parapapillary atrophy were plotted independently by two examiners on HRT images before and after reviewing optic disc photographs. These data were compared with planimetric measurements obtained from analyzing the disc photographs. RESULTS: Before viewing the disc photographs, assessment using the HRT images correlated better with the beta zone than alpha zone planimetric measurements. If the HRT images were 24 evaluated while simultaneously viewing disc photographs, correlation coefficients increased for both examiners 1 and 2. Interobserver and intraobserver reliability were 0.431 and 0.802, respectively, for alpha zone, and 0.882 and 0.948, respectively, for beta zone. CONCLUSION: Parapapillary atrophy can be estimated with confocal scanning laser ophthalmoscopy. Correlation with planimetric measurements is best if conventional optic disc photographs are simultaneously viewed. Intraobserver and interobserver reliability are higher for beta zone than for alpha zone. Br J Ophthalmol 1999 Mar;83(3):299-304 Preperimetric glaucoma diagnosis by confocal scanning laser tomography of the optic disc. Mardin CY, Horn FK, Jonas JB, Budde WM. Department of Ophthalmology and Eye Hospital, Friedrich-Alexander-University, ErlangenNurnberg, Germany. AIM: To evaluate the ability of confocal scanning laser tomography of the optic nerve head to detect glaucomatous optic nerve damage in ocular hypertensive eyes without visual field defects. METHODS: The study included 50 normal subjects, 61 glaucoma patients with glaucomatous changes in the optic disc and visual field, and 102 "preperimetric" patients with increased intraocular pressure, normal visual fields, and glaucomatous appearance of the optic disc as evaluated on colour stereo optic disc photographs. For all individuals, confocal scanning laser tomographs of the optic nerve head were taken using the Heidelberg retina tomograph (HRT; software 2.01). RESULTS: Almost all investigated HRT variables varied significantly (p < 0.05) between the normal eyes and preperimetric glaucoma eyes with pronounced overlap between the two study groups. Corresponding to the overlap, sensitivity and specificity values were relatively low when HRT variables were taken to differentiate between normal and preperimetric glaucoma eyes. At a given specificity of 95% highest sensitivities were found for the variables "rim area in the superior disc sector" (24.8%), "nerve fibre layer thickness in the inferior disc sector" (26.5%), and "rim volume in the superior disc sector" (25.5%). A multivariate approach increased sensitivity to 42.2% at a given specificity of 95%. For the glaucoma group highest sensitivity values were reached by rim volume in the superior disc sector (73.8%) and rim area (72.1%); the multivariate approach reached 83.6%. CONCLUSIONS: Owing to pronounced overlapping between the groups, confocal scanning laser tomography of the optic nerve head has relatively low diagnostic power to differentiate between normal eyes and preperimetric glaucoma eyes. One of the reasons may be the biological interindividual variability of quantitative optic disc variables. Br J Ophthalmol 1999 Mar;83(3):295-298 Comparison between laser scanning tomography and computerised image analysis of the optic disc. Azuara-Blanco A, Spaeth GL, Nicholl J, Lanzl IM, Augsburger JJ. Department of Ophthalmology Queen's Medical Centre, University of Nottingham. AIMS: To study the interchangeability of the measurements of the optic disc topography obtained by one computerised image analyser and one confocal laser tomographic scanner. METHODS: One eye of 28 patients with glaucoma or glaucoma suspects was studied. All cases had simultaneous stereoscopic disc photographs taken with the fundus camera Topcon TRC-SS and optic disc examination with the Heidelberg retina tomograph (HRT) during the same visit. The optic disc photographs were digitised and analysed with the Topcon ImageNet (TI) system. Three variables of the optic disc topography provided by the TI and the HRT were compared—cup volume (CV), rim area (RA), and cup area to disc area ratio (CA/DA). RESULTS: The mean values of CV and RA provided by the TI (0.52 (SD 0.32) mm3 and 1.58 (0.39) mm2, respectively) were greater (p < 0.01) than the mean values of CV and RA determined by the HRT (0.32 (0.25) mm3, and 1.33 (0.47) 25 mm2, respectively). The mean value of CA/DA provided by the TI (0.42 (0.14)) and the HRT (0.42 (0.18)) was similar (p = 0.93). Correlation coefficients between measurements obtained by the two methods ranged from 0.53 to 0.73. CONCLUSION: There was a significant discrepancy in the measurements of rim area and cup volume of the optic disc obtained by a computerised image analyser and a laser scanning tomograph. Am J Ophthalmol 1998 Dec;126(6):763-771 Patterns of optic disk damage in patients with early focal visual field loss. Emdadi A, Zangwill L, Sample PA, Kono Y, Anton A, Weinreb RN. Glaucoma Center and Research Laboratories, University of California, San Diego, La Jolla 920930946, USA. PURPOSE: To study the patterns of structural damage of the optic disk in patients with early focal visual field loss using a confocal scanning laser ophthalmoscope. METHODS: Thirty-nine subjects with repeatable early focal visual field loss were included. The Heidelberg Retina Tomograph (Heidelberg Engineering, Heidelberg, Germany) was used to obtain topographic optic disk measurements. For analysis of structural damage, the topographic measurements were divided into 36 10-degree sectors. Sector analysis was performed using sector rim area to sector disk area ratio. Patients were assigned to one of three groups based on the measurement of the optic disk damage: (1) diffuse disk damage; (2) focal disk damage; or (3) no detectable disk damage. RESULTS: Approximately half of the patients with early focal glaucomatous visual field loss showed diffuse optic disk damage, one quarter to one third had focal damage, and one sixth had no detectable damage. Optic disk area was smallest in the no-detectable-damage group (1.71 + 0.19 mm2), followed by the focal-damage group (2.06 + 0.54 mm2), and was largest in the diffuse damage group (2.29 + 0.48 mm2; P = .22). CONCLUSION: In patients with early focal glaucomatous visual field loss, observable optic disk damage can be diffuse, focal, or undetectable. The Heidelberg Retina Tomograph may be capable of detecting different patterns of diffuse or focal structural damage. Ophthalmology 1998 Dec;105(12):2186-2192 Magnification characteristics of fundus imaging systems. Rudnicka AR, Burk RO, Edgar DF, Fitzke FW. Applied Vision Research Centre, City University, London, England. OBJECTIVE: To compare the magnification properties of 11 different fundus cameras (including 1 stereo fundus camera), a Rodenstock (infrared) scanning laser ophthalmoscope (SLO), the Heidelberg Laser Tomographic Scanner (LTS), and the Heidelberg Retina Tomograph (HRT). DESIGN: A cross-sectional study of the relationship between the true size of a fundus feature and its photographic-computer image in 14 different fundus imaging devices. This relationship was evaluated for each instrument using a model eye adjusted for axial ametropia between +11 diopter (D) and -14 D. To simulate refractive ametropia, the "crystalline lens" was removed to render the model eye aphakic, and the axial length was adjusted to give aphakic ametropia from emmetropia to +20 D. MAIN OUTCOME MEASURES: A correction factor (p) was calculated for each instrument, which can be used in calculations for determining true retinal size. RESULTS: The following were found to be of telecentric construction, Zeiss Oberkochen (WS240 Heidelberg), Zeiss Oberkochen (UK), Zeiss Oberkochen (Cologne), Nikon NF505, Kowa RCXV, SLO prototype (UK), LTS, and the HRT, and each exhibited a constant relationship between p and degree of ametropia of the model eye. The Canon CF6OU, Canon CF6OS, Canon CR4-45NM, Nidek 3-DX, Olympus GRCW, and Carl Zeiss Jena Retinophot were found not to be telecentric and exhibited a linear relationship between p and degree of ametropia of the model eye. For all instruments, p 26 remained unchanged for axial and refractive ametropias of the same degree. CONCLUSIONS: The study has shown that not all fundus imaging systems are telecentric, so the use of a single magnification correction value may not be appropriate. These findings have important implications for the way in which true retinal size calculations are performed. Examples are given to show how the tabulated values of correction factors can be used for both telecentric and nontelecentric cameras in image size calculations. Eye 1998;12( Pt 4):686-690 The correlation of the visual field with scanning laser ophthalmoscope measurements in glaucoma. Tole DM, Edwards MP, Davey KG, Menage MJ. Eye Department, Clarendon Wing, Leeds General Infirmary, UK. PURPOSE: To assess the relationship between Humphrey visual field data and optic disc topographical data collected by the Heidelberg Retina Tomograph (HRT) scanning laser ophthalmoscope in chronic glaucoma patients. METHODS: The mean deviation (MD) and corrected pattern standard deviation (CPSD) from Humphrey visual fields of 106 eyes of 106 patients with glaucoma were analysed for correlation with the multiple topographical measures calculated by the HRT. RESULTS: Significant correlations were found between MD of the visual field and several optic disc measurements. These included neuroretinal rim volume, mean nerve fibre layer thickness and cross-sectional area, and the cup shape measure. CPSD correlated significantly only with mean nerve fibre layer cross-sectional area. This pattern was common to the whole circumference of the disc with the exception of the directly temporal segment. CONCLUSION: Optic disc topography performed by HRT reflects the optic disc pathology in correlation with perimetry. Br J Ophthalmol 1998 Oct;82(10):1112-1117 Laser scanning tomography of localised nerve fibre layer defects. Burk RO, Tuulonen A, Airaksinen PJ. Department of Ophthalmology, University of Heidelberg, Germany. AIMS: Retinal nerve fibre layer photography is a well established method to qualitatively document early structural changes which might be induced by primary open angle glaucoma. The aim was to analyse localised retinal nerve fibre layer (RNFL) defects in a new quantitative way with respect to surface topography, defect width, and surface reflectivity by means of the technique of confocal scanning laser tomography. METHODS: 12 eyes of 12 patients with a localised RNFL defect documented in RNFL photographs and a normal appearance of the optic disc were enrolled in the study. Using confocal laser scanning tomography (Heidelberg retina tomograph, HRT) a series of 32 optical section images from different focal planes of the retina at the site of the RNFL defects were obtained. The optical section images, the reflectivity images, and the topographic images were analysed regarding the visibility of the RNFL defects. The mean surface height and the reflectance at the sites of the RNFL damage were measured and compared with the adjacent apparently normal retina. The width of the RNFL defect at 1 mm distance from the disc border was evaluated. RESULTS: RNFL defects could be detected in nine of 12 reflectivity images (75%). Single optical section images displayed the RNFL defects in 12 of 12 eyes. The defect width ranged from 0.11 to 1.0 mm. In six of 12 eyes a surface depression (34 (SD 5) microns; range 21-47 microns) was present. The reflectance ratio ranged from 0.68 to 0.94 at the site of the RNFL defect. In eyes with a glaucomatous scotoma in a 6 degrees grid visual field (VF), the defect width was at least 0.25 mm. Surface depression and low reflectance ratio were found irrespective of the presence of a scotoma in the 6 degrees grid VF. CONCLUSION: The majority of localised RNFL defects can be detected in 27 reflectivity images from laser scanning tomograms. Localised RNFL defects may be differentiated according to surface topography into those with and those without a measurable surface depression. A small but deep RNFL defect is not necessarily associated with a scotoma in routine 6 degrees grid VF static perimetry. Curr Eye Res 1998 Sep;17(9):903-916 Study of regional deformation of the optic nerve head using scanning laser tomography. Yan DB, Flanagan JG, Farra T, Trope GE, Ethier CR. Department of Ophthalmology, University of Toronto, Ontario, Canada. PURPOSE: Previous studies have suggested that IOP-induced deformation of the optic nerve head (ONH) at the level of the lamina cribrosa may contribute to axonal damage in glaucomatous optic neuropathy. Our purpose was to introduce a novel enucleated eye model for characterizing acute IOP-induced changes in ONH topography, and to develop improved analytical methods for detection of regional topographic change in the ONH. METHODS: Using a specially designed experimental apparatus, enucleated human eyes were progressively pressurized to 5, 15, 30, and 50 mmHg. Seven topographic images of the optic disc were taken at each pressure by a scanning laser tomographer (Heidelberg Retina Tomograph-HRT). The dependence of ONH topography on IOP was quantified for the entire nerve using standard HRT indices of ONH topographic change. The supero-inferior and nasal-temporal hemifields were also analyzed. A new method of analysis was developed which computes the location of the point of maximum slope within a 10 degrees sector of the ONH, as well as the magnitude of this slope. This method, termed "Inflection Point Analysis," was designed to be robust to the potential artefacts of image translation, reference plane location, and the subjective determination of ONH limits. RESULTS: The results of three eyes are presented to illustrate the techniques. In our enucleated eye model, average ONH depth progressively increased with IOP, showing a maximum average posterior displacement of 36 microm as IOP was changed from 5 to 50 mmHg. Significant regional variability in ONH displacement was observed, which both Inflection Point Analysis and standard HRT parameters were able to detect. Inflection point analysis showed several advantages over standard HRT parameters: it was insensitive to artefacts due to tilt, was able to objectively delineate the boundary between the optic cup and neuroretinal rim, and was able to sensitively track changes in the location of this margin. CONCLUSIONS: Scanning laser tomography is capable of detecting regional variation in the deformation of the ONH in response to acute changes in IOP. Our enucleated eye model and Inflection Point Analysis are promising tools for basic studies of ONH deformation in response to IOP. More extensive studies of both enucleated and in vivo eyes are required to determine the potential of Inflection Point Analysis for studying and tracking the progression of glaucomatous optic neuropathy. Ophthalmology 1998 Aug;105(8):1557-1563 Identification of early glaucoma cases with the scanning laser ophthalmoscope. Wollstein G, Garway-Heath DF, Hitchings RA. Glaucoma Unit, Moorfields Eye Hospital, London, England. PURPOSE: This study aimed to define the confocal laser scanning ophthalmoscope (Heidelberg Retina Tomograph [HRT]) parameters that best separate patients with early glaucoma from normal subjects. STUDY DESIGN: A cross-sectional study. PARTICIPANTS: A total of 80 normal subjects and 51 patients with early glaucoma participated (average visual field mean deviation = 3.6 dB). INTERVENTION: Imaging of the optic nerve head with the HRT and analysis using software version 1.11 were performed. MAIN OUTCOME MEASURES: The relation between neuroretinal rim area and optic disc area, and cup-disc area ratio and optic disc area, was defined by linear regression of data derived from the normal subjects. The normal ranges for these two 28 parameters were defined by the 99% prediction intervals of the linear regression between the parameter and optic disc area, for the whole disc, and for each of the predefined segments. Normal subjects and patients were labeled as abnormal if the parameter for either the whole disc or any of the predefined segments was outside the normal range. The sensitivity and specificity values of the method were calculated. RESULTS: The highest specificity (96.3%) and sensitivity (84.3%) values to separate normal subjects and those patients with early glaucoma were obtained using the 99% prediction interval from the linear regression between the optic disc area and the log of the neuroretinal rim area. Similar specificity (97.5%) and lower sensitivity (74.5%) values were obtained with the 99% prediction interval derived from regression between the disc area and cupdisc area ratios. Poor separation between groups was obtained with the other parameters. CONCLUSIONS: The HRT, using the technique of linear regression to account for the relationship between optic disc size and rim area or cup-disc area ratio, provides good separation between control subjects and patients with early glaucoma in this population. Nippon Ganka Gakkai Zasshi 1998 Jun;102(6):378-382 Use of a scanning laser tomograph to evaluate the optic disc of the normal eyes. Nakamura H, Maeda T, Suzuki Y, Inoue Y. Eye Division of Olympia Medical Clinic, Tokyo, Japan. We evaluated the optic disc in 77 eyes of 77 normal volunteers using a scanning laser tomograph (Heidelberg Retina Tomograph: HRT, version 1.11). Particular attention was paid to age, refractive error, and disc size. The topographic parameters included: cup area, C/D area ratio, rim area, cup volume, rim volume, mean cup depth, maximum cup depth, cup shape measure, height variation contour, mean RNFL thickness, and RNFL cross section area. There was a significant decline in mean RNFL thickness and RNFL cross section area with increase in age (p < 0.05). The mean and maximum cup depths were significantly deeper in myopic eyes (p < 0.05). Large discs had large values of cup area, C/D area ratio, rim area, cup volume, mean cup depth, cup shape measure (p < 0.01), and maximum cup depth (p < 0.05). Large discs had small values of mean RNFL thickness and RNFL cross section area. Rim volume was independent of age, refractive error, or disc area. Br J Ophthalmol 1998 Apr;82(4):362-366 Comparison of measurements of neuroretinal rim area between confocal laser scanning tomography and planimetry of photographs. Jonas JB, Mardin CY, Grundler AE. Department of Ophthalmology and Eye Hospital, Friedrich-Alexander-University, ErlangenNurnberg, Germany. BACKGROUND: To compare neuroretinal rim area measurements by confocal scanning laser tomography and planimetric evaluation of optic disc photographs. METHODS: For 221 patients with primary and secondary open angle glaucoma, 72 subjects with ocular hypertension, and 139 normal subjects, the optic disc was morphometrically analysed by the confocal scanning laser tomograph HRT (Heidelberg retina tomograph) and by planimetric evaluation of stereo colour optic disc photographs. RESULTS: Absolute rim area and rim to disc area were significantly (p < 0.0001) larger with the HRT than with planimetric evaluation of photographs. Differences between the two methods were significantly (p < 0.01) larger in normal eyes with small cupping than in normal eyes with large cupping, and differences were significantly (p < 0.01) larger in glaucomatous eyes with marked nerve damage than in glaucomatous eyes with moderate nerve damage. Coefficients of correlations between rim measurements of both methods were R2 = 0.60 for rim to disc area and R2 = 0.33 for absolute rim area. Planimetric measurements of rim area correlated significantly (p < 0.05) better than HRT determinations of rim area with mean visual 29 field defect and retinal nerve fibre layer visibility. CONCLUSIONS: Measurements of absolute rim area and rim to disc area are significantly larger with the HRT compared with planimetry of disc photographs. Differences between both methods depend on disc area, cup size and glaucoma stage. The reason may be that the HRT measures the retinal vessel trunk as part of the neuroretinal rim. The differences between both methods, which should be taken into account if disc measurements performed by both methods are compared with each other, may not influence the main advantage of the HRT--that is, morphological follow up examination of patients with glaucoma. J Glaucoma 1998 Apr;7(2):121-127 Detection of early glaucomatous structural damage with confocal scanning laser tomography. Bathija R, Zangwill L, Berry CC, Sample PA, Weinreb RN. Department of Ophthalmology, University of California, San Diego, La Jolla 92093-0946, USA. PURPOSE: The authors determine which optic disc topographic parameters obtained by the Heidelberg Retina Tomograph (HRT, Heidelberg Engineering, Heidelberg, Germany) are most useful in detecting individuals with early glaucomatous visual field loss. METHODS: Ninety-nine eyes of 49 healthy individuals and 50 age-matched individuals with early glaucomatous visual field loss were included. Three images were obtained and the mean topography image was created and used in the analyses. The HRT discriminant analysis function (software version 2.01) was applied and compared to the Fisher linear discriminant function developed in this population. Analysis was repeated after stratifying by disc area (< 2 mm2 or 2-3 mm2). RESULTS: There were statistically significant differences between the healthy and glaucomatous groups for all optic disc topographic parameters (p < 0.05) measured. These differences remained after the analysis was repeated controlling for disc size, except for height variation contour. Applying the HRT discriminant function to this study population resulted in sensitivity and specificity of 62% and 94%, respectively. The sensitivity was 83% while specificity remained high (91%) for larger disc sizes. Using this data, additional discriminant functions that differentiated similarly between the two groups were found. The best formula used cup-shape measure (third moment), rim area, height variation contour, and retinal nerve fiber layer thickness and had a sensitivity and specificity of 78% and 88%, respectively. CONCLUSIONS: Several different discriminant analysis formulas are capable of detecting early glaucomatous visual field loss in a comparable manner. The characteristics of the study population are likely to influence the discriminating power of these various formulas. Ophthalmologica 1998;212(2):95-98 Reproducibility of optic disk topographic measurements with the Topcon ImageNet and the Heidelberg Retina Tomograph. Azuara-Blanco A, Harris A, Cantor LB. Department of Ophthalmology, Indiana University, School of Medicine, Indianapolis, USA. OBJECTIVE: To compare the reproducibility of optic disk measurements provided by an image analyzer and a scanning laser tomograph. METHODS: Ten images of the same eye of 10 normal volunteers were taken with the Heidelberg Retina Tomograph and with the Topcon ImageNet. Intraclass correlation coefficient (ICC) and coefficient of variation (CV) were used to evaluate the reproducibility of the measurements. RESULTS: Eleven parameters were analyzed with the Topcon ImageNet. Six parameters (55%) had ICC greater than 90%. Four parameters (36%) had CV less than 10%. Twelve parameters were evaluated with the Heidelberg Retina Tomograph. Nine parameters (75%) had ICC over 90%. Nine parameters (75%) had CV less than 10%. CONCLUSION: Both systems provided reproducible data. The optic disk parameters provided by 30 the Heidelberg Retina Tomograph had a better reproducibility than those obtained from the Topcon ImageNet. Klin Monatsbl Augenheilkd 1998 Feb;212(2):74-79 Can the extent of glaucoma damage be assessed by measuring the asymmetry of the peripapillary height profile between the upper and lower retinal half? A clinical study with the Heidelberg Retina Tomograph. Serguhn S, Gramer E. Universitats-Augenklinik Ulm. BACKGROUND: Peripapillary height measurements are possible using 2 different reference planes of the Heidelberg-Retina-Tomograph. It is not tested yet, whether the extent of glaucoma damage should be better quantified using reference plane 1 or 2. PATIENTS AND METHODS: In 32 eyes of 32 glaucoma patients with a defined up-down asymmetry of visual field loss is tested I.) if there is a significant correlation between peripapillary height and visual field loss comparing reference plane 1 and 2. II.) if there is a conformable up-down asymmetry of the peripapillary height using a new "retinal-asymmetry-difference" (RAD). III.) if conformity between peripapillary height and visual field loss depends on the distance from the disc margin. RESULTS: 1.) For an advanced visual field loss there was a significant correlation between visual field loss and peripapillary height using reference plane 1. II.) In eyes with a big up-down asymmetry of visual field loss there was a bigger conformity between the up-down asymmetry of visual field loss and the up-down asymmetry of peripapillary height (11 of 12 eyes), as for a small up-down asymmetry (12 of 20 eyes). III.) Conformity decreases with the distance from the disc margin. CONCLUSIONS: Peripapillary height should be examined using measurement circles near the disc margin. Because of its independence on the age and on different reference planes additional calculation of an up-down "retinal-asymmetry-difference" (RAD) seems to be useful. Using this up-down "retinal-asymmetrydifference" (RAD) a big up-down asymmetry of visual field loss, equivalent to an advanced glaucomatous disease, is quantified with high sensitivity. J Glaucoma 1997 Dec;6(6):363-370 A comparison of healthy, ocular hypertensive, and glaucomatous optic disc topographic parameters. Iester M, Broadway DC, Mikelberg FS, Drance SM. Department of Ophthalmology, University of British Columbia, Vancouver, Canada. PURPOSE: To compare the optic discs of 62 healthy individuals 68 patients who have ocular hypertension (OH), and 182 patients with primary open-angle glaucoma (132 high-tension glaucoma (HTG) and 50 normal-tension glaucoma (NTG)), and determine whether disc size exerted an influence on the group differentiation. PATIENTS AND METHODS: Standard criteria were used to define glaucoma and normality. Ocular hypertension was defined as having raised intraocular pressure, a normal visual field, and a healthy optic disc/retinal nerve fiber layer (RNFL). The optic disc of one eye from each individual was analyzed using a confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph software version 1.11, Heidelberg Engineering, Heidelberg, Germany). Thirteen topographical, volumetric, and shape parameters were compared between the three diagnostic groups. In addition, the individuals were divided into subgroups on the basis of disc size to determine any effect of disc size on the differentiating ability of the confocal scanning laser ophthalmoscope. Differences between the groups were evaluated using an analysis of variance. RESULTS: Glaucomatous optic discs were found to differ from both healthy and OH discs, although no differences in disc area between the groups were identified. On the basis of disc size, differentiating the glaucomatous discs was best for midsized discs of 2 mm2 to 3 mm2. 31 However, no difference was found between healthy and OH discs, even when allowing for disc size. CONCLUSIONS: Ocular hypertensive optic discs (with a clinically normal appearance) could not be distinguished from healthy discs using a confocal scanning laser ophthalmoscopic technique. Glaucomatous optic discs were found to differ from both healthy and OH discs, with a limited effect of disc size. Invest Ophthalmol Vis Sci 1997 Nov;38(12):2452-2459 Correlation of blue-on-yellow visual fields with scanning confocal laser optic disc measurements. Teesalu P, Vihanninjoki K, Airaksinen PJ, Tuulonen A, Laara E. Department of Ophthalmology, University of Oulu, Finland. PURPOSE: Visual field defects and changes in the optic nerve head are signs of glaucoma. It has been shown that blue-on-yellow (B-Y) perimetry can reveal visual field defects earlier and shows them larger than does white-on-white (W-W) perimetry. The Heidelberg retina tomograph (HRT) can produce three-dimensional images of the optic disc. The aim of this study was to find out how B-Y perimetry results correlate with optic disc parameters in comparison with W-W perimetry results. METHODS: One randomly chosen eye was evaluated in each of 40 normal subjects and 37 patients with ocular hypertension and different stages of glaucoma. B-Y and W-W visual fields (program 30-2) were obtained with a Humphrey perimeter. B-Y perimetry results were adjusted for the patient's age and lens transmission index measured with a lens fluorometer. The B-Y visual field adjusted mean deviation (MD) was calculated as the difference between the measured and expected mean sensitivity values, predicted by the regression model fitted in normal subjects. The HRT with software version 1.11 was used to acquire and evaluate topographic measurements of the optic disc. RESULTS: The cup shape measure showed strongest correlation with the MD of both the B-Y and W-W visual fields. The multiple correlation coefficients from quadratic regression were 0.65 for both visual fields. Except for peripapillary retinal nerve fiber layer measurements, the statistically significant correlations of the B-Y visual field indexes with other HRT parameters were equal to or better than those of W-W perimetry. CONCLUSIONS: B-Y perimetry MDs are well correlated with optic nerve head parameters measured with the HRT. In early stages of glaucoma, most HRT variables were better correlated with the B-Y MD than with the W-W MD. Invest Ophthalmol Vis Sci 1997 Nov;38(12):2452-2459 Correlation of blue-on-yellow visual fields with scanning confocal laser optic disc measurements. Teesalu P, Vihanninjoki K, Airaksinen PJ, Tuulonen A, Laara E. Department of Ophthalmology, University of Oulu, Finland. PURPOSE: Visual field defects and changes in the optic nerve head are signs of glaucoma. It has been shown that blue-on-yellow (B-Y) perimetry can reveal visual field defects earlier and shows them larger than does white-on-white (W-W) perimetry. The Heidelberg retina tomograph (HRT) can produce three-dimensional images of the optic disc. The aim of this study was to find out how B-Y perimetry results correlate with optic disc parameters in comparison with W-W perimetry results. METHODS: One randomlychosen eye was evaluated in each of 40 normal subjects and 37 patients with ocular hypertension and different stages of glaucoma. B-Y and W-W visual fields (program 30-2) were obtained with a Humphrey perimeter. B-Y perimetry results were adjusted for the patient's age and lens transmission index measured with a lens fluorometer. The B-Y visual field adjusted mean deviation (MD) was calculated as the difference between the measured and expected mean sensitivity values, predicted by the regression model fitted in normal subjects. The HRT with software version 1.11 was used to acquire and evaluate topographic measurements of the optic disc. 32 RESULTS: The cup shape measure showed strongest correlation with the MD of both the B-Y and W-W visual fields. The multiple correlation coefficients from quadratic regression were 0.65 for both visual fields. Except for peripapillary retinal nerve fiber layer measurements, the statistically significant correlations of the B-Y visual field indexes with other HRT parameters were equal to or better than those of W-W perimetry. CONCLUSIONS: B-Y perimetry MDs are well correlated with optic nerve head parameters measured with the HRT. In early stages of glaucoma, most HRT variables were better correlated with the B-Y MD than with the W-W MD. Ophthalmology 1997 Nov;104(11):1926-1933 The associations of optic disc hemorrhage with retinal nerve fiber layer defect and peripapillary atrophy in normal-tension glaucoma. Sugiyama K, Tomita G, Kitazawa Y, Onda E, Shinohara H, Park KH. Department of Ophthalmology, Gifu University School of Medicine, Japan. OBJECTIVE: The purpose of the study is to elucidate a topographic correlation between optic disc hemorrhages and retinal nerve fiber layer defects as well as peripapillary atrophy in normal-tension glaucoma (NTG). DESIGN: The authors prospectively studied the relation between the precise locations of disc hemorrhages and retinal nerve fiber layer defects in the first part of the study. The authors also compared morphometrically the peripapillary atrophy and the optic disc in eyes with disc hemorrhage with eyes without a history of disc hemorrhage in age-matched patients in the second part of the study. PARTICIPANTS: In part 1, 42 patients with NTG (male/female = 11/31; age, 56.8 +/- 14.2 years) in whom new disc hemorrhages developed were enrolled. In part 2, 51 randomly selected age-matched patients with NTG without a history of disc hemorrhage (male/female = 16/35; age, 55.7 +/- 12.5) were examined. MAIN OUTCOME MEASURE: In part 1, retinal nerve fiber layer defects were observed by scanning laser ophthalmoscopy using an argonblue laser. In part 2, the area, angular extent, and radial extent of zone beta of peripapillary atrophy and the structural parameters of optic disc were measured by scanning laser tomography using a diode laser. RESULTS: In part 1, the authors detected 64 disc hemorrhages in 48 eyes of 42 patients; retinal nerve fiber layer defects were shown in 47 (97.9%) of 48 eyes by scanning laser ophthalmoscopy. Of 64 disc hemorrhages, 51 (79.7%) coincided with retinal nerve fiber layer defects in location. These 51 hemorrhages were present on the border (41.2%) or adjacent to the border (58.8%) between the retinal nerve fiber layer defect and the apparently healthy-looking retinal nerve fiber layer. In part 2, the prevalence, area, angular extent of zone beta, and ratio of zone beta area to disc area were significantly greater in the disc hemorrhage group than in the nonhemorrhage group, even though there were no significant differences in disc parameters between the two groups. CONCLUSIONS: Disc hemorrhage is associated closely with retinal nerve fiber layer defect in location and the size of peripapillary atrophy in NTG. Klin Monatsbl Augenheilkd 1997 Oct;211(4):235-240 Are there genuine and pseudo-normal pressure glaucomas? Body position-dependent intraocular pressure values in normal pressure glaucoma. Mardin CY, Jonas J, Michelson G, Junemann A. Universitats-Augenklinik mit Poliklinik Erlangen-Nurnberg, Erlangen. BACKGROUND: Elevation of intraocular pressure in the supine position has been previously described in literature. Aim of this study is to investigate the elevation of intraocular pressure in normal tension glaucoma and its effect on the morphology of the optic disc, visual field function and capillary blood flow of the retina and optic disc. PATIENTS AND METHODS: 56 eyes of 28 preperimetric and advanced normal tension glaucoma patients were prospectively evaluated. Ten eyes of ten normal patients served as a control group for the measurements of the intraocular 33 pressure. In the course of a 24-h pressure profile applanation tonometry was performed in the morning in a supine and three and ten minutes later in a sitting position with Draeger's and Goldmann's tonometers. Arterial blood pressure was measured at the same time. The optic disc's morphology was evaluated by stereo photographs and Laser Scanning Tomography. As a sensory test computer perimetry was used. Capillary blood flow was measured at defined areas of the retina and optic disc. An intraocular pressure above 21 mm Hg in the supine position was used as a criterium to define two groups of normal tension glaucoma patients. RESULTS: In the supine position a statistically significant elevation of intraocular pressure was observed in 24 normal tension glaucoma patients by 6.2 +/- 2.8 mm Hg up to 21.8 +/- 3 mm Hg. Diastolic blood pressure in the supine position (80 +/- 10.5 mm Hg) was significantly lower than in the sitting position (94 +/- 11 mm Hg, p = 0.021). 12 of 28 normal tension glaucoma patients showed an intraocular pressure lower than 22 mm Hg in the supine position. In these patients a tendency towards a higher incidence for the occurrence of optic disc haemorrhages and significantly higher values for blood flow (p < 0.0005) and volume (p < 0.005) in the retina and optic nerve head could be shown. In this group of normal pressure glaucoma patients a higher incidence of migraine and vasospastic complaints was reported in the patients' history. CONCLUSION: In this study some normal tension glaucoma patients showed intraocular pressures in the supine position higher than 21 mm Hg and a lower diastolic arterial pressure. The higher incidence of haemorrhages and higher values for flow and volume parameters of the optic disc in normal tension glaucoma patients with an intraocular pressure lower than 22 mm Hg implicate the existence of two entities: real and pseudo normal tension glaucomas. Br J Ophthalmol 1997 Oct;81(10):871-876 Laser scanning tomography of the optic nerve head in ocular hypertension and glaucoma. Hatch WV, Flanagan JG, Etchells EE, Williams-Lyn DE, Trope GE. University of Waterloo, Toronto Hospital Glaucoma Research Unit, Ontario, Canada. BACKGROUND: This study evaluated the ability of laser scanning tomography to distinguish between normal and glaucomatous optic nerve heads, and between glaucomatous subjects with and without field loss. METHODS: 57 subjects were classified into three diagnostic groups: subjects with elevated intraocular pressure, normal optic nerve heads, and normal visual fields (n = 10); subjects with glaucomatous optic neuropathy and normal visual fields (n = 30); and subjects with glaucomatous optic neuropathy and repeatable visual field abnormality (n = 17). Three 10 degrees image series were acquired on each subject using the Heidelberg retina tomograph (HRT). From the 14 HRT stereometric variables, three were selected a priori for evaluation: (1) volume above reference (neuroretinal rim volume), (2) third moment in contour (cup shape), and (3) height variation contour (variation in relative nerve fibre layer height at the disc margin). Data were analysed using analysis of covariance, with age as the covariate. RESULTS: Volume above reference, third moment in contour, and mean height contour were significantly different between each of the three diagnostic groups (p < 0.001). Height variation contour showed no significant difference among the three diagnostic groups (p = 0.906). CONCLUSIONS: The HRT variables measuring rim volume, cup shape, and mean nerve fibre layer height distinguished between (1) subjects with elevated intraocular pressures and normal nerve heads, and glaucomatous optic nerve heads, and (2) glaucomatous optic nerve heads with and without repeatable visual field abnormality. This study did not directly assess the ability of the HRT to identify patients at risk of developing glaucoma. It is hypothesised that the greatest potential benefit of laser scanning tomography will be in the documentation of change within an individual over time. Br J Ophthalmol 1997 Oct;81(10):871-876 Laser scanning tomography of the optic nerve head in ocular hypertension and glaucoma. 34 Hatch WV, Flanagan JG, Etchells EE, Williams-Lyn DE, Trope GE. University of Waterloo, Toronto Hospital Glaucoma Research Unit, Ontario, Canada. BACKGROUND: This study evaluated the ability of laser scanning tomography to distinguish between normal and glaucomatous optic nerve heads, and between glaucomatous subjects with and without field loss. METHODS: 57 subjects were classified into three diagnostic groups: subjects with elevated intraocular pressure, normal optic nerve heads, and normal visual fields (n = 10); subjects with glaucomatous optic neuropathy and normal visual fields (n = 30); and subjects with glaucomatous optic neuropathy and repeatable visual field abnormality (n = 17). Three 10 degrees image series were acquired on each subject using the Heidelberg retina tomograph (HRT). From the 14 HRT stereometric variables, three were selected a priori for evaluation: (1) volume above reference (neuroretinal rim volume), (2) third moment in contour (cup shape), and (3) height variation contour (variation in relative nerve fibre layer height at the disc margin). Data were analysed using analysis of covariance, with age as the covariate. RESULTS: Volume above reference, third moment in contour, and mean height contour were significantly different between each of the three diagnostic groups (p < 0.001). Height variation contour showed no significant difference among the three diagnostic groups (p = 0.906). CONCLUSIONS: The HRT variables measuring rim volume, cup shape, and mean nerve fibre layer height distinguished between (1) subjects with elevated intraocular pressures and normal nerve heads, and glaucomatous optic nerve heads, and (2) glaucomatous optic nerve heads with and without repeatable visual field abnormality. This study did not directly assess the ability of the HRT to identify patients at risk of developing glaucoma. It is hypothesised that the greatest potential benefit of laser scanning tomography will be in the documentation of change within an individual over time. Ophthalmologe 1997 Sep;94(9):673-677 Quantitative and objective follow-up of papilledema with the Heidelberg Retina Tomograph. Gobel W, Lieb WE, Grein HJ. Universitats-Augenklinik Wurzburg. The Heidelberg retina tomograph (HRT) is a new instrument to analyze the three-dimensional structure of the retina. It is based on confocal laser scanning technology. Scientific interest has so far focused on the follow-up of glaucomatous optic nerve head damage. As parameters such as cup depth and cup volume can be reproduced with a high degree of accuracy, this new instrument may prove to be an excellent tool to follow up swelling of the optic disk. PATIENTS AND METHOD: A total of 21 patients suffering from optic disk swelling of various etiologies were included in a pilot study. Measurements were taken at six different time points. The maximum optic disk elevation and the volume of swelling were evaluated. Visual acuity and the visual field were determined, and fundus photographs were taken. RESULTS: A reduction in optic disk swelling over time may be demonstrated by both morphological parameters and correlates with improvement in fundus changes. The change in the volume of swelling is greater than the change in maximum disk elevation. The course of optic disk swelling differs between patients with anterior ischemic optic neuropathy and those with pseudotumor cerebri. No correlation was found between our measurements with the HRT and functional parameters (visual acuity and visual field). CONCLUSION: The HRT is a good tool for the follow-up of optic disk swelling, particularly optic disk elevation due to increased intracranial pressure. J Glaucoma 1997 Aug;6(4):221-230 Quantitative estimation of retinal nerve fiber layer height in glaucoma and the relationship with optic nerve head topography and visual field. Eid TM, Spaeth GL, Katz LJ, Azuara-Blanco A, Agusburger J, Nicholl J. 35 William and Anna Goldberg Glaucoma Service, Wills Eye Hospital, Jefferson Medical College, Philadelphia, Pennsylvania 19107, U.S.A. PURPOSE: The authors estimated the retinal nerve fiber layer height (RNFLH) measurements in patients with glaucoma compared with those in age-matched healthy subjects as obtained by the laser scanning tomography and assessed the relationship between RNFLH measurements and optic and visual field status. METHODS: Parameters of optic nerve head topography and RNFLH were evaluated in 125 eyes of 21 healthy subjects and 104 patients with glaucoma using the Heidelberg Retina Tomograph ([HRT] Heidelberg Engineering GmbH, Heidelberg, Germany) for the entire disc area and for the superior 70 degrees (50 degrees temporal and 20 degrees nasal to the vertical midline) and inferior 70 degrees sectors of the optic disc. The mean deviation of the visual field, as determined by the Humphrey program 24-2 (Humphrey Instruments, Inc., San Leonardo, CA, U.S.A) was calculated in the entire field and in the superior and inferior Bjerrum area. RESULT: Retinal nerve fiber layer height parameters (mean RNFLH and RNFL cross-sectional area) were decreased significantly in patients with glaucoma compared with healthy individuals. Retinal nerve fiber layer height parameters was correlated strongly with rim volume, rim area, and cup/disc area ratio. Of the various topography measures, retinal nerve fiber layer (RNFL) parameters and cup/disc area ratio showed the strongest correlation with visual field mean deviation in patients with glaucoma. CONCLUSION: Retinal nerve fiber layer height measures were reduced substantially in patients with glaucoma compared with age-matched healthy subjects. Retinal nerve fiber layer height was correlated strongly with topographic optic disc parameters and visual field changes in patients with glaucoma. Arch Ophthalmol 1997 Aug;115(8):983-990 Effect of cataract and pupil size on image quality with confocal scanning laser ophthalmoscopy. Zangwill L, Irak I, Berry CC, Garden V, de Souza Lima M, Weinreb RN. Department of Ophthalmology, University of California-San Diego, La Jolla, USA. OBJECTIVE: To determine the effect of pupil size and cataract on the reproducibility and image quality obtained with confocal scanning laser ophthalmoscopy. METHODS: Three image series were obtained with a confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph, Heidelberg, Germany) before and after pupillary dilation in each of 39 subjects (8 normal subjects, 5 glaucoma suspects, and 26 patients with glaucoma). The cataract density was measured with both a lens opacity meter and the Lens Opacities Classification System III system. The image quality of each image series was subjectively scored on a scale of 0 (poor) to 9 (high) by 2 independent observers who were unaware of the cataract density and pupil size during image acquisition. The image quality and reproducibility were objectively evaluated using the SD of the mean topography image of each subject. RESULTS: The mean pupil diameter in all subjects before and after dilation was 2.5 +/- 0.8 mm and 5.8 +/- 1.4 mm, respectively. After pupillary dilation, both the mean image quality score and mean SD of the mean topography image improved (from 4.5 +/- 3.5 to 7.4 +/- 2.3 and from 48.6 +/- 18.8 microns to 35.6 +/- 15.5 microns, respectively). The quality score of the images that were obtained before pupillary dilation was associated with the pupil size and density of nuclear and posterior subcapsular cataracts. The SD of the mean topography images that were obtained before pupillary dilation increased with a decreasing pupil size (P = .003) and an increasing density of the nuclear (P < .03), cortical (P = .02), and posterior subcapsular (P = .002) opacity. CONCLUSIONS: Although pupillary dilation improved the image quality in most subjects, the improvement was sometimes small. Those subjects with small undilated pupils and/or cataracts may benefit most from pupillary dilation. 36 Korean J Ophthalmol 1997 Jun;11(1):7-14 Circumferential profiles of peripapillary surface height with confocal scanning laser ophthalmoscopy. Park HJ, Caprioli J. Ghil Medical Center, Department of Ophthalmology, Inchon, Korea. The purpose of this study was to compare the circumferential profiles of relative peripapillary retinal surface height (RPSH) between normal and glaucoma, with a confocal scanning laser ophthalmology (CSLO), and to examine the ability of the mean height to distinguish glaucoma from normal. Fifty-three patients with open-angle glaucoma and forty-three normal subjects matched for age, race and refractive error were studied. To extract circumferential profiles, we developed software to quantify RPSH from images obtained with a CSLO (Heidelberg Retina Tomograph (HRT), Heidelberg Engineering, Germany, Software: IR1-V1.11) outside the optic disc margin every 50 microns. Mean heights from circumferential profiles were calculated and compared between normal and glaucoma. Receiver operating characteristic (ROC) curves were used to evaluate sensitivity and specificity of the mean height to discriminate normal from glaucoma subjects. T he average (+/- SD) visual field mean deviation in the glaucoma group was -4.8 +/3.4dB. The average height of each circumference increased from the disc margin to 250 microns away in both normal and glaucoma subjects. There were statistically significant differences for the mean height (P < 0.001) between the two groups. The largest difference between normal and glaucoma was found in the inferior sector compared with the other sectors (p < 0.001). The sensitivity, specificity and diagnostic precision of the mean height were 83%, 67% and 76%, respectively. The mean height from the circumferential profiles of RPSH can be used as a useful marker to identify early glaucoma. Ophthalmologe 1997 May;94(5):360-363 Does the fundus perimetry determined edge of the blind spot depend on the superficial form of the papilla? Meyer JH, Guhlmann M, Funk J. Universitats-Augenklinik Freiburg. BACKGROUND: We wanted to find out whether the borders of the blind spot depend on the surface topography of the optic disc and its surrounding area. PATIENTS AND METHODS: We therefore examined ten eyes with parapapillary atrophy adjacent to the temporal side of the disc. Fundus perimetry was performed under direct fundus control using a Rodenstock scanning laser ophthalmoscope. We examined the horizontal meridian of the optic discs in 0.5 degree steps using Goldmann IV-stimuli with 10 different degrees of brightness and the Goldmann stimulus 1, 0 dB (greatest luminance). Six eyes with symmetric, "normal" excavation served as controls. Optic disc topography was measured with the Heidelberg Retina Tomograph (HRT). RESULTS: Stimuli with a large luminance power (Goldmann IV, 4 dB) were seen up to 0.8 degree centrally (i.e., towards the optic disc center) from the temporal edge of the parapapillary atrophy, but up to 1.9 degrees centrally from the nasal optic disc border (P < 0.01). Horizontal HRT section profiles of the optic disc consistently showed prominent nasal disc borders contrasting with a shallow excavation within the temporal parapapillary atrophy. In all six subjects with a normally shaped disc there was no such "nasotemporal asymmetry." CONCLUSIONS: The size of scotomas depends on the surface topography of the tested area. The prominent nasal part of the optic disc appears less "blind" than the shallow temporal part, probably due to more intensive light scattering by the prominent nasal part of the disc. Phys Med Biol 1997 May;42(5):951-966 37 The scanning laser ophthalmoscope. Sharp PF, Manivannan A. Department of Biomedical Physics and Bioengineering, University of Aberdeen, Foresterhill, UK. The imaging of the fundus of the eye poses two major technical challenges. First, it is necessary for both the illuminating and reflected beams to pass through the same aperture, the iris. In some commonly used instruments this leads to the use of levels of illumination close to the maximum tolerable by a patient. Second, in order to visualize the different structures present in the various layers of the fundus it is necessary to perform tomographic imaging. The scanning laser ophthalmoscope provides an answer to these particular problems. By scanning the fundus with a narrow laser beam most of the area of the iris is then available for the reflected light and so the intensity of the illuminating beam can be kept low, making it more acceptable for patients. The use of confocal imaging allows 3D images to be produced. In this short review the performance of the instrument will be discussed and its application to a number of clinical problems in ophthalmology considered. Finally there will be a brief description of other instrumentation currently under development. Br J Ophthalmol 1997 May;81(5):355-359 Blind spot size depends on the optic disc topography: a study using SLO controlled scotometry and the Heidelberg retina tomograph. Meyer JH, Guhlmann M, Funk J. Universitats-Augenklinik, Freiburg, Germany. AIMS: To find out whether the size of the blind spot area, determined by static perimetry, depends on the surface topography of the optic disc and its surrounding area. METHODS: Ten eyes were examined; all had a parapapillary atrophy adjacent to the temporal side of the disc. Microperimetry was performed under direct fundus control using a Rodenstock scanning laser ophthalmoscope. The horizontal meridian of the optic discs was examined in 0.5 degree steps using five stimulus sizes (Goldmann I to V), each with 10 different degrees of brightness. Optic disc topography was measured with the Heidelberg retina tomograph (HRT). RESULTS: Stimuli with a high luminance level (Goldmann IV, 4 dB), presented on the horizontal meridian, were seen up to 0.75 degree centrally (that is, towards the optic disc centre) from the temporal edge of the parapapillary atrophy but up to 1.85 degrees centrally from the nasal optic disc border (p < 0.01). Horizontal HRT section profiles of the optic disc consistently showed prominent nasal disc borders contrasting with a shallow excavation within the temporal parapapillary atrophy. CONCLUSIONS: The size of scotomas depends on the surface topography of the tested area. The prominent nasal part of the optic disc appears less 'blind' than the shallow temporal part, probably because of more intensive light scattering by the prominent nasal part of the disc. These considerations should also apply to other scotomas. Curr Opin Ophthalmol 1997 Apr;8(2):50-54 Methods to objectify reversibility of glaucomatous cupping. Azuara-Blanco A, Spaeth GL. Glaucoma Service, Wills Eye Hospital, Philadelphia, PA 19107, USA. Lowering intraocular pressure in adults with glaucoma may be associated with an improvement in appearance of the optic nerve head. The stage of disease, the amount of intraocular pressure reduction, and the age of the patient probably influence the occurrence of this event. The clinical relevance of "reversal" has not been established with certainty. The reversibility of glaucomatous cupping can be detected by subjective and qualitative means (examination of the patient or of 38 fundus photographs) or by quantitative techniques such as photogrammetry, computerized image analysis, and scanning laser tomography. Clinical and experimental studies are providing new information about the behavior of the optic nerve head tissues in response to changes in intraocular pressure. Curr Opin Ophthalmol 1997 Apr;8(2):38-41 New definitions of glaucoma. Gupta N, Weinreb RN. Glaucoma Center, University of California San Diego, La Jolla 92093-0946, USA. At this time, there is no comprehensive and specific definition of glaucoma. Diagnostic tests such as retinal nerve fiber layer observation, scanning laser polarimetry, and confocal scanning laser tomography may improve the diagnosis and detection of glaucoma. Also, new functional tests, including short-wave-length automated perimetry, may provide better detection of glaucoma. Curr Opin Ophthalmol 1997 Apr;8(2):7-12 Laser scanning tomography and angiography of the optic nerve head for the diagnosis and follow-up of glaucoma. Melamed S, Levkovitch-Verbin H. Sam Rothberg Glaucoma Center, Goldschleger Eye Institute, Sheba Medical Center, Tel-Hashomer, Israel. New imaging technologies allow us to detect and follow very subtle changes of the structure and perfusion of the optic nerve head. Two of these technologies, confocal scanning laser ophthalmoscopy and confocal tomographic angiography are reviewed, focusing on new data and advances reported in the past year. These and other technologies (eg, nerve fiber layer polarimetry, optical coherent topography, and laser doppler flowmetry) will enhance the ability to diagnose and monitor glaucomatous disc damage. Ophthalmology 1997 Mar;104(3):545-548 The effect of optic disc size on diagnostic precision with the Heidelberg retina tomograph. Iester M, Mikelberg FS, Drance SM. Department of Ophthalmology-University of British Columbia, Vancouver, Canada. PURPOSE: The authors evaluated the ability of a confocal scanning laser ophthalmoscope to detect glaucomatous visual field loss by using their previously described discriminant formula on a prospectively obtained cohort. The relationship of optic disc size to diagnostic classification was also evaluated. METHODS: One eye was chosen randomly from each of 153 subjects. Sixty control eyes had intraocular pressure less than 21 mmHg and normal visual fields; 93 glaucomatous eyes had intraocular pressure greater than 21 mmHg and abnormal visual fields. The optic disc status purposely was not used for classification purposes. All subjects were examined with the Heidelberg Retina Tomograph (HRT; Heidelberg Engineering GMBH, Heidelberg, Germany) and Humphrey Perimeter, program 30-2 (Humphrey Instruments, Inc., San Leandro, CA). Visual fields were considered abnormal by the authors' previously published criteria. The HRT classification used age, adjusted cup shape measure, rim volume, and height variation contour to classify the optic disc as normal or glaucomatous. Then the authors assessed the sensitivity, specificity, and diagnostic precision for the entire group, and for three subsets classified by disc area: disc area less than 2 mm2, between 2 and 3 mm2, and more than 3 mm2. RESULTS: The entire group had a sensitivity, specificity, and diagnostic precision of 74%, 88%, and 80%, respectively. The specificity was 83% 39 when disc area was less than 2 mm2 and improved to 89% when disc area was more than 2 mm2. The sensitivity tended to improve from 65% to 79%, and to 83% if the disc area increased, but the difference was not statistically significant. CONCLUSIONS: In a prospective cohort of patients, the HRT discriminant analysis formula was capable of detecting glaucomatous visual field loss with good precision. Unusually small optic discs continue to present diagnostic difficulties. Ophthalmology 1996 Nov;103(11):1899-1906 Correlation between peripapillary atrophy and optic nerve damage in normal-tension glaucoma. Park KH, Tomita G, Liou SY, Kitazawa Y. Department of Ophthalmology, College of Medicine, Seoul National University Hospital, Korea. PURPOSE: To investigate the correlation between peripapillary atrophy and visual field defects as well as optic nerve head configurations in patients with normal-tension glaucoma (NTG). METHODS: Topographic measurements for peripapillary atrophy and optic nerve head using confocal scanning laser tomography and automated static threshold perimetry were performed on 102 eyes of 51 patients with NTG. Peripapillary atrophy was divided into (1) a central zone (zone Beta) with visible, large choroidal vessels and sclera, and (2) a peripheral zone (zone Alpha) with irregular hyper- and hypopigmentation. The area, angular extent around the disc, and radial extent of each zone were measured. RESULTS: The area and extent of zone Beta increased significantly with increasing visual field defects expressed in terms of mean deviation, corrected pattern standard deviation, central visual field defects within 5 degrees of fixation, and superior hemifield defects (r = 0.3770-0.5291, P < 0.01). The angular extent of zone Beta represented localized field defects better (r = 0.5217, P < 0.001) than diffuse field defects (r = -0.3770, P < 0.01). Zone Beta significantly correlated with optic nerve head topography. Intraindividual right-left-side differences of corrected pattern standard deviation showed the highest correlation with the side differences of zone Beta area (r = 0.6305, P < 0.001). The location of visual field defects correlated significantly with the location of peripapillary atrophy (chi-square = 9.0484, P = 0.011). Zone Alpha was not significantly correlated with visual field defects or optic nerve head configurations (P > 0.05). CONCLUSION: Peripapillary atrophy is significantly associated with functional and structural optic nerve damage in NTG. Am J Ophthalmol 1996 Nov;122(5):690-695 Change in optic disk topography after trabeculectomy. Irak I, Zangwill L, Garden V, Shakiba S, Weinreb RN. Glaucoma Center and Research Laboratories, University of California, San Diego 92093-0946, USA. PURPOSE: To investigate the relationship between optic disk topography and intraocular pressure before and after trabeculectomy with confocal scanning laser ophthalmoscopy. METHODS: The eyes of 49 consecutive patients undergoing trabeculectomy at a university-based glaucoma practice underwent preoperative and postoperative imaging using a confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph). Three images of one eye of each patient were obtained with a 15degree field of view. Preoperative images were obtained approximately 2 months before surgery (mean +/- SD, 2.4 +/- 1.6 months). Postoperative images were obtained at least 3 months after surgery (mean, 4.5 +/- 2.6 months). RESULTS: Mean preoperative intraocular pressure, postoperative intraocular pressure, and percent change in intraocular pressure respectively were 23.1 +/- 6.8 mm Hg, 12.7 +/- 7.1 mm Hg, and 43.8% +/- 29.9%. A significant association (P < .01) was found between percent decrease in intraocular pressure and decreases in cup area, cup volume, and cup/disk area ratio as well as between percent decrease in intraocular pressure and increases in 40 rim area, rim volume, mean height contour, retinal cross-section area, and height in contour. Between 11.7% and 31.2% of the variability (R2) in these parameters was explained by the percent change in intraocular pressure. Topography changes were more strongly associated with percent change than with mean change in intraocular pressure. We found no association between percent decrease in intraocular pressure and reference plane height or maximum cup depth. CONCLUSIONS: Changes in optic nerve topography were associated with reduction in intraocular pressure after trabeculectomy. 41 Heidelberg Retina Tomograph und Macula Medline Abstracts Dezember 1996 bis März 2001 Ophthalmic Surg Lasers 2001 Mar;32(2):95-99 Three-dimensional analysis of macular diseases with a scanning retinal thickness analyzer and a confocal scanning laser ophthalmoscope. Konno S, Takeda M, Yanagiya N, Akiba J, Yoshida A. Department of Ophthalmology, Asahikawa Medical College, Japan. [email protected] OBJECTIVE: To compare three-dimensional analysis of macular diseases obtained using the scanning retinal thickness analyzer (RTA) with that obtained using the confocal scanning laser ophthalmoscope, Heidelberg Retina Tomograph (HRT). PATIENTS AND METHODS: Both the RTA and the HRT were used to examine 50 eyes of 36 patients with diabetic macular edema, macular edema following branch retinal vein occlusion, age-related macular degeneration, and idiopathic macular holes. RESULTS: In most macular diseases, the retinal thickness map constructed using the RTA agreed with the image obtained with the HRT. The two maps were not consistent with each other, however, in patients with dense retinal hemorrhages and with extrafoveal fixation. CONCLUSIONS: Although both the RTA and the HRT give additional information to clinically evaluate macular diseases, they do have limitations. The discrepancy between these two analyses in some specific macular pathologies might be caused by the different wavelengths of the laser beam and the different methodologies used to scan the retina. Br J Ophthalmol 2001 Jan;85(1):34-39 Sensitivity and specificity of a new scoring system for diabetic macular oedema detection using a confocal laser imaging system. Tong L, Ang A, Vernon SA, Zambarakji HJ, Bhan A, Sung V, Page S. Department of Ophthalmology, Queen's Medical Centre, University Hospital, Nottingham NG7 AIM: To assess the use of the Heidelberg retina tomograph (HRT) in screening for sight threatening diabetic macular oedema in a hospital diabetic clinic, using a new subjective analysis system (SCORE). METHODS: 200 eyes of 100 consecutive diabetic patients attending a diabetologist's clinic were studied, all eyes had an acuity of 6/9 or better. All patients underwent clinical examination by an ophthalmologist. Using the HRT, one good scan was obtained for each eye centred on the fovea. A System for Classification and Ordering of Retinal Edema (SCORE) was developed using subjective assessment of the colour map and the reflectivity image. The interobserver agreement of using this method to detect macular oedema was assessed by two observers (ophthalmic trainees) who were familiarized with SCORE by studying standard pictures of eyes not in the study. All scans were graded from 0-6 and test positive cases were defined as having a SCORE value of 0-2. The sensitivity of SCORE was assessed by pooling the data with an additional 88 scans of 88 eyes in order to reduce the confidence interval of the index. RESULTS: 12 eyes in eight out of the 100 patients had macular oedema clinically. Three scans in three patients could not be analysed because of poor scan quality. In the additional group of scans 76 out of 88 eyes had macular oedema clinically. The scoring system had a specificity of 99% (95% CI 96-100) and sensitivity of 67% (95% CI 57-76). The predictive value of a negative test was 87% (95% CI 82-99), and that of a positive test was 95% (95% CI 86-99). The mean difference of the SCORE value between two observers was -0.2 (95% CI -0.5 to +0.07). CONCLUSIONS: These data suggest that SCORE is potentially useful for detecting diabetic macular oedema in hospital diabetic patients. 42 Nippon Ganka Gakkai Zasshi 2000 Dec;104(12):899-942 New examination methods for macular disorders--application of diagnosis and treatment. Yoshida A. Department of Ophthalmology, Asahikawa Medical College. To establish a diagnosis or evaluate the efficacy of treatment for macular disorders, we need methods to evaluate the anatomical and functional changes of these disorders. In this article, we describe several studies that we have conducted for 2 years. In section 1, we report our new methods for making a diagnosis and evaluating visual function in macular disorders. In section 2, we describe our trials of these examination methods in treatment. Here is the summary of our results. In section 1, to examine the structures of the macular area, we used a retinal thickness analyzer (RTA), a confocal scanning laser ophthalmoscope (Heidelberg Retina Tomograph, HRT), and optical coherence tomography (OCT) to measure retinal thickness and assess retinal microstructures. We compared retinal imaging analysis of various macular diseases obtained with these three instruments. With the RTA, we obtained good three-dimensional macular images displayed on a retinal thickness map, but the retinal thickness map did not demonstrate the thickened retina with dense retinal hemorrhages, and high backscattering from hard exudates might obscure the vitreoretinal interface. The HRT three-dimensional topographic image clearly showed the undulation of the retinal surface. However, it took a relatively long time to obtain the HRT image, and we sometimes could not obtain good topographic images because of fixation movement. Examination with the OCT allows confirmation of the retinal cross-sectional structures, such as retinoschisis or cystoid spaces and the vitreomacular interface, such as vitreous traction, that cannot be detected using other conventional methods with high resolution, but high reflectivity from dense hemorrhages obscured the deeper layers of the retinal structures. Measurement of retinal thickness obtained with both the RTA and OCT is highly reproducible, and there was significant correlation between the retinal thicknesses measured with the two instruments. We believe that these three instruments might contribute significantly to early, accurate diagnosis and better monitoring of the therapeutic effects of vitrectomy for macular diseases. In the future, if these fundus imaging analysis instruments can achieve higher resolution and can analyze three-dimensional retinal images, they will provide better information to clinically evaluate macular diseases. We demonstrated vitreous examination and examination from the retinal surface to the deeper retinal layer at the macular area using a scanning laser ophthalmoscope (SLO). The SLO examination with an argon laser and a large confocal aperture was useful for conducting kinetic examination of the vitreous opacity above the macula. With a diode laser and a ring aperture (dark-field mode), it was possible to examine the retina from the deeper retinal layer to the choroids. On the other hand, the SLO also allows us to conduct a functional examination of fixation. We demonstrated that the referred retinal locus of fixation may change during the follow-up period in patients whose central fixation is impaired due to macular disease, and we showed that the fixation behavior was related to the visual acuity. Therefore, the SLO is an ideal instrument for determining the visual field and the visual acuity before and after treatment in patients with macular disease, because of its precise localization of the examination point by directly observing the fundus and by monitoring fixation behavior. Our new program installed in the SLO allows us to complete the quantitative retinal sensitivity evaluation within 2 minutes, which is difficult to do using a conventional SLO program. Furthermore, we demonstrated for the first time that minute functional changes in the retina can be detected by the SLO under low background illuminance. Such changes cannot be detected under conventional conditions. In addition, the extrafoveal visual acuity of normal subjects and patients with macular disease was studied using this new SLO program. The iso-acuity lines could be illustrated by summarizing these results in normal subjects. The SLO acuity of the horizontal meridian is significantly better than that of the vertical meridian, and even in the nasal area adjacent to the optic disc, an acuity of better than 0.1 could be achieved. To evaluate macular function, we also investigated the blood flow of the choroid (CF), the retina (RF), and the choriocapillaris at the 43 fovea (CCF). We investigated the CF in patients with age-related macular degeneration (AMD) using pulsatile ocular blood flow (POBF) measurements. In patients with exudative AMD, the POBF was significantly lower than in patients with nonexudative AMD or in control subjects. Decreased CF may play a role in the development of choroidal neovascularization in AMD. RF was measured using laser Doppler velocimetry (LDV). Br J Ophthalmol 2000 Oct;84(10):1194-1197 Improvement of reproducibility of macular volume measurements using the Heidelberg retinal tomograph. Ang A, Tong L, Vernon SA. Department of Ophthalmology, Queen's Medical Centre, University Hospital, Nottingham NG7 2UH, UK. AIMS: To develop a more reproducible method of macular volumetric analysis in order to facilitate serial monitoring of changes in retinal oedema with time. METHODS: The Heidelberg retinal tomography (HRT) machine was used to scan the macula of 20 normal subjects and 40 diabetics with macular oedema. The volume above reference plane (VARP) within a 2 mm diameter and 3 mm diameter circle was measured twice in each eye. The position of the circle to be measured was carefully defined relative to major retinal vessels. As a modification to the previously published technique, fluctuation of the height of the contour line relative to the focal plane of the eye is compensated for by an adjustment of the reference plane. The position of the circle was controlled relative to major retinal vessels using an acetate. The reproducibility of VARP measurement was assessed by three variables-the standard error of the difference on two isolated VARP measurements, the standard error of the difference between the average of three readings on two different occasions, as well as the coefficient of variation (COV). RESULTS: Both the 2 mm and 3 mm circles showed good reproducibility in VARP measurements. In normal subjects, the COV of VARP for 2 mm circles and 3 mm circles were 13% and 12% respectively. In patients with macular oedema, the COV of VARP for 2 mm circles and 3 mm circles were 9% and 11% respectively. CONCLUSION: The modification of VARP measurements between scans of the same eye has improved the COV from 31% to 9% in eyes with diabetic macular oedema. Am J Ophthalmol 2000 Jul;130(1):65-75 Three-dimensional observations of developing macular holes. Kishi S, Takahashi H. Department of Ophthalmology, Gunma University School of Medicine, Maebashi, Gunma, Japan. [email protected] PURPOSE: To describe the morphologic features of idiopathic macular holes and vitreous traction during macular hole evolution. METHODS: We prospectively examined 89 eyes of 82 patients with idiopathic macular holes (stage 1, 15 eyes; stage 2, 16 eyes; stage 3, 50 eyes; stage 4, eight eyes) using optical coherence tomography. In addition to optical coherence tomography, scanning laser ophthalmoscopy was performed in all 15 eyes with stage 1 hole, six of 16 eyes with stage 2, and 19 of 50 eyes with stage 3. RESULTS: In stage 1 eyes, optical coherence tomography revealed retinal split or cystic changes at the fovea in 11 of 15 eyes (73%) and foveal retinal detachment in four eyes (27%). Two eyes with foveal cysts progressed to stage 2, and one developed a stage 3 hole. In one eye with retinal detachment, the detached retina thinned and developed dehiscence. Optical coherence tomography showed a vitreous cortex that was detached in the perifoveal area but attached on the fovea in 11 of the 15 stage 1 eyes. In stage 2 macular holes, retinal tissue extending from the perifoveal retina formed a flap. Scanning laser ophthalmoscopy demonstrated intraretinal radiating striae, which corresponded to a foveal cyst or perifoveal cystic changes. CONCLUSIONS: 44 Macular holes start as retinal splits or foveal cysts in most cases. The anterior wall of the cyst serves as a flap in stage 2 and an operculum in stage 3 holes. Radiating striae correspond to retinal splits or cysts and presumably represent an elevation of Henle fiber. In a few macular holes, foveal detachment is the initial change. The detached retina thins and eventually develops a hole. In both courses, anterior traction of the slightly detached vitreous cortex appears to be a major contributing factor to macular hole formation. Graefes Arch Clin Exp Ophthalmol 2000 May;238(5):410-419 Quantitative measurements of changes of idiopathic stage 3 macular holes after vitrectomy using confocal scanning laser tomography. Kobayashi H, Kobayashi K. Department of Ophthalmology, Amagasaki Hospital, Amagasaki, Japan. [email protected] PURPOSE: To perform quantitative three-dimensional analysis of changes of idiopathic fullthickness stage 3 macular holes following vitrectomy and gas tamponade using confocal scanning laser tomography to study the mechanism of repairing the holes and to correlate with visual recovery. METHODS: We studied 44 patients, 10 men and 34 women, aged between 40 and 76 years (mean 65.5 years) with stage 3 macular holes with symptoms of 1-4 months' duration (mean 2.7 months). Using the Heidelberg Retina Tomograph, we measured the macular area within 1 week before surgery (3.5+/-1.6 days), and between 2 and 4 weeks (2.4+/-0.6 weeks) and at least 3 months (3.8+/-00.8 months) after surgery. RESULTS: All 44 eyes showed closure of the holes and flattening of cuff and retinal striae after vitrectomy and gas tamponade. All the eyes showed small flat depressions that corresponded to each macular hole with the area of 0.027-0.184 mm2 (0. 110+/-0.042 mm2). Thirty-nine (89%) of 44 eyes showed large concave depressions that appeared to correspond to the preoperative retinal striae, with areas of 0.844 to 5.563 mm2 (3.688+/-1.263 mm2). The areas of the postoperative small depressions and large depressions were significantly correlated with the area, volume, and depth of the macular holes and the area of the cuff and retinal striae prior to treatment. Postoperative visual acuity showed significant correlations with the areas of the postoperative small depressions and large depressions. CONCLUSIONS: Confocal scanning laser tomography is potentially useful as a noninvasive diagnostic technique for quantitative measurements of changes of macular holes by vitrectomy and gas tamponade. Postoperative small depressions corresponding to the healed macular holes appeared to be caused by gliosis involving sealing of the holes. The large depressions and their concave shape may result from postoperative changes of the retina, including swelling of ganglion cells and loss of outer and inner segments of photoreceptor cells in regions of preoperative cuff and retinal striae. Ophthalmology 2000 Mar;107(3):593-599 Comparison between optical coherence tomography and fundus fluorescein angiography for the detection of cystoid macular edema in patients with uveitis. Antcliff RJ, Stanford MR, Chauhan DS, Graham EM, Spalton DJ, Shilling JS, Ffytche TJ, Marshall J. GKT Department of Ophthalmology, Rayne Institute, St Thomas' Hospital, London, England. PURPOSE: To compare optical coherence tomography (OCT) with fundus fluorescein angiography (FFA) for the detection of cystoid macular edema (CME) in patients with uveitis. DESIGN: Prospective comparative observational series. PARTICIPANTS: One hundred twenty-one eyes of 58 patients with uveitis of varied causes (seven patients were studied twice). TESTING: Patients with suspected CME underwent OCT scanning followed by FFA at the same visit. MAIN OUTCOME MEASURES: Detection and distribution of macular edema. RESULTS: One hundred 45 eight eyes had similar results on both OCT and FFA in that 67 eyes had CME and 41 eyes had no CME. In 10 eyes subretinal fluid was detected on OCT but not FFA. Five of these eyes had CME on FFA but not OCT. Three other eyes had CME that was detected by FFA but not by OCT. Compared with FFA, the OCT sensitivity for detecting CME was 96% (including the eyes with subretinal fluid), and the OCT specificity was 100%. CONCLUSIONS: OCT is as effective at detecting CME as is FFA but is superior in demonstrating axial distribution of fluid. Ophthalmologe 2000 Mar;97(3):173-180 Volume determination of pigment epithelium detachment in AMD by laser scanning tomography. Spital G, Brumm G, Radermacher M, Muller C, Lommatzsch A, Pauleikhoff D. Augenabteilung, St. Franziskus Hospital, Munster. BACKGROUND: The possibility of using 3D mapping of AMD-related RPE detachments by means of laser scanning tomography was evaluated to correlate the fluorescein and tomographic findings. METHODS: Sixty eyes with AMD-related RPE detachments of 55 consecutive patients (19 men, 36 women) between 54 and 87 years of age (mean: 72.2 years) were examined using the Heidelberg Retina Tomograph (HRT). The parameters considered were area, volume, maximal height and 3D configuration of the RPE detachments. The tomographic data were analyzed and correlated with the fluorescein angiographic findings. Follow-up examinations were done at 3 and 6 months later. RESULTS: The mean +/- SD area of elevation was 10.59 +/- 5.51 mm2 (range, 0.9319.73), which correlated well with the angiographic measurements. The mean maximal height was 0.42 +/- 0.19 mm (range, 0.11-0.83), mean volume was 2.55 +/- 1.9 mm3 (range, 0.073-6.63). We found a tendency to grow for untreated RPE detachments, depending on the volume at the first measurement. Three RPE detachments of high volume (mean 0.501 +/- 1.3 mm3) resulted in tearing of the RPE. The angiographic findings of localized neovascularizations in the RPE detachment area (39 of 60 eyes) showed a corresponding irregularity of the surface in most of the correlating 3D HRT figures. CONCLUSIONS: Confocal laser scanning tomography allows analysis of 3D configurations and a quantitative measurement of RPE detachments in AMD. Therefore, this diagnostic technique appears to be useful, especially for differentiated follow-up examinations (as in therapy-control studies). Furthermore, the analysis of 3D configurations seems to be useful to estimate the risk of tearing of the RPE and may help to indicate underlying neovascularizations. Ophthalmic Surg Lasers 1999 Jul;30(7):513-517 Three-dimensional characteristics of macular pseudoholes using confocal laser tomography. Akiba J, Yanagiya N, Konno S, Hikichi T, Yoshida A. Department of Ophthalmology, Asahikawa Medical College, Japan. [email protected] BACKGROUND: Epiretinal membranes with macular pseudoholes are sometimes confused with full-thickness macular holes. Because both the natural course and clinical management of the two differ, an accurate differential diagnosis is needed. PATIENTS AND METHODS: We obtained three-dimensional images of macular pseudoholes in 12 eyes using the Heidelberg retina tomograph (HRT). Another 15 eyes with a full-thickness macular hole were also studied. In addition, we measured the area and the maximum depth of both types of holes. RESULTS: Irregular rippling undulations were frequently observed on the three-dimensional topographic maps around the pseudoholes, whereas elevated cuffs were observed around the full-thickness holes. The maximum depth of the macular pseudoholes (mean, 57 microm) was significantly shallower than that of the full-thickness macular holes (mean, 156 microm; P < 0.01). CONCLUSION: Three-dimensional images obtained by the HRT and the measurement of the maximum depth may be useful in differentiating macular pseudoholes from full-thickness macular holes. 46 Graefes Arch Clin Exp Ophthalmol 1999 Apr;237(4):283-288 Correlation of quantitative three-dimensional measurements of macular hole size with visual acuity after vitrectomy. Kobayashi H, Kobayashi K. Department of Ophthalmology, Amagasaki Hospital, Hyogo, Japan. [email protected] OBJECTIVE: The purpose of the study was to study the relationship of postoperative visual outcome with anatomical parameters of macular holes using confocal scanning laser tomography and to predict the postoperative visual results. DESIGN: Cohort study. INTERVENTION AND PARTICIPANTS: We evaluated the eyes of 44 patients undergoing macular hole surgery (10 men and 34 women aged 40-76 years, mean 59.1 years). All patients showed idiopathic full-thickness stage 3 macular holes. The duration of symptoms was 1-4 months (mean 2.7 months). MAIN OUTCOME MEASURES: The area, volume, mean depth, and maximum depth of the macular holes and the areas of cuff and retinal striae were measured using the Heidelberg Retina Tomograph preoperatively. RESULTS: All 44 eyes showed closure of the holes and flattening of cuff and retinal striae after vitrectomy and gas tamponade. Postoperative visual acuity was significantly correlated with the area (r = 0.822, P<0.0001), volume (r = 0.840, P<0.0001), mean depth (r = 0.842, P<0.0001), and maximum depth (r = 0.831, P<0.0001) of the macular holes, area of cuff (r = 0.625, P<0.0001), and area of retinal striae (r = 0.648, P<0.0001). Multiple regression analysis showed that the combination of the preoperative mean depth of macular holes and logarithm of preoperative visual acuity was the strongest predictor of the postoperative visual acuity. CONCLUSIONS: Postoperative visual results vary significantly with the size of macular holes in patients with stage 3 macular holes of duration 1-4 months. The use of the confocal scanning laser tomography may facilitate the evaluation of macular holes efore surgery. Ability to predict the postoperative visual results would be helpful in treating patients with macular holes. Doc Ophthalmol 1999;97(3-4):349-360 Reproducibility of volumetric macular measurements in diabetic patients with the Heidelberg Retina Tomograph. Zambarakji HJ, Vernon SA, Spencer AF, Amoaku WM. Department of Ophthalmology, Queen's Medical Centre, University Hospital, Nottingham, UK. AIMS: To quantify diabetic macular edema by confocal scanning laser ophthalmoscopy and assess its usefulness by determining the reproducibility of topographic measurements at the macula. METHODS: The volumes above reference plane bound by a 2 mm diameter circle centred on the fovea were measured by two observers. The reference plane was adjusted to the lowest point of the height variation of the contour line. The reproducibility of this technique was assessed in 20 eyes of 20 diabetic patients of which 8 eyes had macular edema. Three HRT scans of each eye were obtained. The measurements of volume above reference plane of each scan were repeated three times. RESULTS: For all diabetic eyes, the intra scan coefficients of variability measured 14.71% to 21.21%, the inter scan coefficient of variability was 30.46%. The average standard deviations were 0.053 mm3 for one examination per scan, 0.047 mm3 for two examinations per scan and 0.044 mm3 for three examinations per scan. Linear regression demonstrated an increase in standard deviation with greater volumetric measurements (p < 0.001). We found good correlation (r = 0.959, p < 0.001) and strong agreement between the two observer's findings for all 20 eyes. For the 8 eyes with macular edema, the coefficients of variability were similar to those calculated for all 20 eyes. The average SD for one examination per scan were 0.078 mm3, 0.069 mm3 for two examinations per scan and 0.062 mm3 for three examinations per scan. We found good correlation (r = 0.945, p < 0.001) and strong agreement between the two observer's findings in eyes with edema. 47 CONCLUSION: The reproducibility of this technique has been demonstrated in diabetic eyes. This may have useful clinical applications for the quantification of diabetic macular edema and monitoring of laser therapy. Ophthalmology 1999 Feb;106(2):274-279 The use of confocal scanning laser tomography in the evaluation of retinal elevation in agerelated macular degeneration. Jaakkola A, Vesti E, Immonen I. Department of Ophthalmology, Helsinki University Central Hospital, Finland. OBJECTIVE: To evaluate the feasibility of using confocal scanning laser tomography in the analysis of macular topography in patients with subfoveal choroidal neovascularization associated with age-related macular degeneration (AMD) and to analyze quantitatively the changes in topography after local strontium-plaque radiation therapy. DESIGN: Prospective case series. PARTICIPANTS: A total of 16 eyes with subfoveal choroidal neovascular membranes (CNVM) treated with strontium-90 (90Sr)-plaque radiation therapy and 16 fellow eyes of 16 patients were examined. INTERVENTION: Confocal scanning laser analysis of macular surface topography before and after irradiation of the macula was performed. MAIN OUTCOME MEASURES: Parameters describing the height and volume of the retinal elevation in the macula were measured. RESULTS: The maximum height of the macular lesion at baseline was 0.25 mm (standard deviation [SD], 0.12 mm) in eyes showing regression of the CNVM during follow-up and 0.34 mm (SD, 0.19 mm) in eyes showing continued growth of the CNVM. During follow-up, a mean decrease in the maximum height of the macular lesion ranging from 0.03 to 0.10 mm occurred in eyes with regression of the CNVM, whereas the mean maximum height increased by 0.07 to 0.15 mm during follow-up visits in eyes with continued growth of the CNVM. All parameters describing the mean height and volume of the lesion also decreased significantly in patients showing angiographic regression, whereas they increased or remained unchanged in patients with continuous growth of the CNVM despite irradiation. The corresponding parameters also were higher in fellow eyes with untreated CNVM than in eyes without exudative AMD. CONCLUSIONS: Confocal scanning laser tomography can be used to monitor the amount of the change in neurosensory detachment in AMD. The parameters obtained by confocal scanning laser tomography correlate with CNVM perfusion after 90Sr-plaque radiation therapy. This technology is a useful tool for objective evaluation of morphologic change after institution of new therapeutic methods for the treatment of AMD. Br J Ophthalmol 1997 Feb;81(2):107-116 Objective morphological assessment of macular hole surgery by scanning laser tomography. Hudson C, Charles SJ, Flanagan JG, Brahma AK, Turner GS, McLeod D. University Department of Ophthalmology, Manchester Royal Eye Hospital. AIM: To assess the morphological change in retinal topography using a scanning laser tomographer following macular hole surgery. To compare the results of scanning laser tomography with clinical evaluation and visual function assessment. METHODS: The sample for this pilot study comprised four eyes exhibiting different stages of macular hole formation preoperatively. Subjects were assessed preoperatively and at 1 and 3 months postoperatively. Each assessment included visual acuity, letter contrast sensitivity, clinical examination (including automated static perimetry), and scanning laser tomography. The Heidelberg retina tomograph (HRT) was used to acquire digitised scanning laser tomography images of the macula (10 degrees and 20 degrees fields). Surgery essentially comprised vitrectomy, peeling of the posterior hyaloid face, if still attached, and intraocular gas tamponade. The magnitude and significance of topographic change were determined 48 postoperatively using the HRT topographic difference facility. RESULTS: Topographic difference analysis of the right and left eyes of case 1 showed a significant reduction in the height of the retina postoperatively. Topographic difference analysis of case 2 showed no significant change in topography. Topographic difference analysis of case 3 showed a significant increase in the height of the retina postoperatively. Scanning laser tomography agreed with clinical assessment based upon fundus biomicroscopy in three of the four eyes studied; the postoperative closure of the stage 2 macular hole (as noted by clinical assessment) proved to be too small to reach statistical significance. Scanning laser tomography agreed with the assessment of visual function in two eyes; the agreement between scanning laser tomography and visual function depends, in part, on the stage of development of the macular hole. CONCLUSION: Scanning laser tomography provides an objective evaluation of the outcome of macular hole surgery. Studies employing larger sample sizes are required to fully determine the clinical worth of the technique. Am J Ophthalmol 1996 Dec;122(6):864-869 Three-dimensional measurements of central serous chorioretinopathy using a scanning laser tomograph. Weinberger D, Stiebel H, Gaton DD, Friedland S, Priel E, Yassur Y. Department of Ophthalmology, Rabin Medical Center, Petah Tiqva, Israel. PURPOSE: To evaluate the topographic three-dimensional mapping of retinal elevation in central serous chorioretinopathy using the Heidelberg Retina Tomograph and to correlate the measured parameters with the fluorescein angiographic findings. METHODS: Seventy-six consecutive patients with central serous chorioretinopathy (63 men, 13 women), between 26 and 54 years of age, were examined to identify areas of neurosensory retinal detachment and fluorescein leakage. In areas of retinal detachment, the parameters measured were the area, volume, maximal height, and diameters of the retinal elevation, which were statistically analyzed, and the correlations between these parameters were evaluated. RESULTS: Mean +/- SD area of elevation was 9.6 +/- 5.22 mm2 (range, 2.7 to 21.5 mm2); mean volume was 1.16 +/- 1.3 mm3 (range, 0.11 to 4.73 mm3); mean maximal height was 238 +/- 108 microns (range, 97 to 450 microns); mean x-axis was 3.4 +/- 1.1 mm (range, 1.6 to 5.6 mm); and mean y-axis was 3.03 +/- 0.98 mm (range, 1.6 to 4.7 mm). Most of the retinal elevations were oval (the x-axis longer than the y-axis); the maximal height was in the geometric center in the smaller blebs and below the geometric center in the larger blebs. There were statistically significant correlations between area, volume, and height of the sensory elevation. No correlation was found between the location and the shape of leakage on fluorescein angiography and the Heidelberg Retina Tomograph measurements. CONCLUSIONS: Confocal laser tomography is potentially useful as a noninvasive diagnostic technique for quantitative measurements of the neurosensory retinal detachment in central serous chorioretinopathy. 49