* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Renal system
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
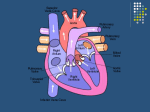
Lectures' headings for dental students: CVS Cardiovascular System: I. Heart -Location of heart (anatomy). -Pericardial layers (one fibrous pericardium and two serous pericardia “parietal pericardium and visceral pericardium”) -Layers of the heart (endocardium, myocardium and epicardium “which is itself the visceral pericardium”) -Chambers of the heart (two atria and two ventricles). -Veins of right atrium a. Superior vena cava return flow from regions superior to diaphragm. b. Inferior vena cava return flow from regions inferior to diaphragm. c. Coronary sinus drain blood from myocardium. -Veins of left atrium are four pulmonary veins from lungs back to heart. -Muscles a. Trabeculae carneae (crossbars). b. Papillary muscles project into heart cavity with a valve function. -Pulmonary trunk routes blood from right ventricle to lungs (pulmonary circulation). Aorta routes blood from left ventricle (systemic circulation). Systemic circulation has five times as much resistance to blood flow than pulmonary circulation due to its longer route. So, left ventricle is much larger and thicker to do more work. -1- Lectures' headings for dental students: CVS Heart Valves A. Atrioventricular (AV) valves are two (right and left) valves between atria and ventricles. They prevent backflow into atria. They are closed during ventricular contraction (systole). -Right AV valve is tricuspid (with three cusps which are reinforced endocardium). -Left AV valve is bicuspid (or mitral valve). Chordae tendineae (heart strings) are collagen cords attached to the cusps to anchor cusps to papillary muscles. During ventricular contraction, intraventricular pressure rises and forces blood against valve flaps. Chordae tendineae anchor flaps in closed position. B. Semilunar valves (SL) are also two. - Aortic valve between left ventricle and aorta. - Pulmonary valve between right ventricle and pulmonary trunk. They open during ventricular contraction (systole). Intraventricular pressure exceeds the blood pressure in aorta and pulmonary trunk. Three crescent shaped cusps open out against arterial walls. C. No valves between atria and venae cavae and pulmonary veins but, atrial contraction compresses venous entry points. -2- Lectures' headings for dental students: CVS Blood Flow to the Heart: The heart requires its own circulatory system and myocardium is too thick to permit diffusion of gases and nutrients. Right and left coronary arteries provide blood supply to the heart (coronary circulation). Blood flow to myocardium occurs only during diastole. Anastomoses allow collateral routes of blood flow. Cardiac veins follow course of coronary arteries and join to form coronary sinus which empties into right atrium. Anterior cardiac veins empty directly into right atrium Pathology A. Angina pectoris: Is a temporary deficient blood flow to the myocardium. Thoracic pain is symptom B. Myocardial infarction (MI) or heart attack: O2 deficiency causes necrosis (cell death). Cardiac cells are amitotic. Cells that die are replaced by non-contractile scar tissue. -3- Lectures' headings for dental students: CVS Cardiac Muscle: Branched, short, and interconnected fibers. It is striated and contracts by sliding filament mechanism. Cardiac muscle fibers are functionally connected by intercalated discs and gap junctions. As a result of gap junctions, entire myocardium acts as a single unit (functional syncytium). Cardiac muscle is self-excitable (i.e., autorhytmic) which initiate action potentials (AP) independent of nervous innervation. Long refractory period after AP prevents tetanic contractions. There are specific noncontractile cardiac cells called pace maker cells that form 1% of heart muscle and depolarize spontaneously to initiate and distribute impulses. Autorhythmic fibers are contractile muscle fibers depolarize in response to pacemaker cell activities. Autorhythmic cells have unstable resting membrane potential which drifts spontaneously towards threshold: 1. Na+ influx (slow) offset by K+ efflux (slow). K+ permeability gradually decreases. 2. Influx of Na+ depolarizes the cardiac cells. Depolarization opens fast Ca2+ channels. Ca2+ influx from extracellular space causes rising phase of action potential. 3. Repolarization causes K+ permeability to increase. K+ channels inactivate. 4. Cycle starts again -4- Lectures' headings for dental students: CVS Location of autorhythmic cells 1. Sinoatrial (SA) node: Has the fastest rate of depolarization. Sinus rhythm is the characteristic rhythm of the heart (gallop rhythm). Located in right atrial wall. After depolarization is initiated, depolarization wave sweeps via gap junctions throughout atria 2. Atrioventricular (AV) node. Depolarization wave initiated by SA node reaches AV node. AV node is located in interatrial septum near tricuspid valve. Diameter of fibers is smaller which slows impulse conduction (0.1 s) to permit completion of atrial contraction. Impulse passes to bundle of His 3. Atrioventricular bundle (bundle of His) permits functional passage of impulse from atria to ventricles. Located in inferior interatrial septum. It is very short and branches to form bundle branches 4. Bundle branches course interventricular septum toward apex of heart 5. Purkinje fibers reach apex then branch superiorly into ventricular walls. Impulses in fibers moves faster than cell to cell contact to ensure greater pumping efficacy -5- Lectures' headings for dental students: CVS Pathology of Intrinsic Conductance System A. Arrhythmias: Uncoordinated contractions of atria and ventricles B. Fibrillation: Rapid, irregular contractions -Atrial fibrillation. -Ventricular fibrillation. C. Ectopic focus: Excitable tissue other than SA node controls heart contractions D. Heart block: Damage to AV node so that impulse cannot reach ventricles Extrinsic control of the heart (brain based control) 1. Cardioaccelatory center in medulla provides sympathetic NS control to innervate SA and AV nodes. 2. Cardioinhibitory center provides parasympathetic NS control via vagus nerve to SA and AV nodes to slow heart rate. Electrocardiography: ECG (EKG) Deflection waves: 1. P wave: Depolarization moving from SA node through atria 2. QRS complex: Ventricular depolarization precedes contraction 3. T wave: Ventricular repolarization occurs more slowly than depolarization so it spreads out much than QRS Intervals: 1. P-R: Interval from beginning of atrial excitation and ventricular excitation. Includes atrial depolarization and contraction and passage of impulse through intrinsic conduction system. It lasts 0.16 sec. 2. Q-T: Interval from ventricular depolarization through repolarization. Includes time of ventricular contraction. -6- Lectures' headings for dental students: CVS Mechanical events during heart contraction: Cardiac cycle includes systole (contraction) and diastole (relaxation) of total 0.8 seconds. Atrial systole lasts 0.1 s and ventricular systole lasts 0.3 s while quiescent period lasts 0.4 s. Mechanical events are: 1. Start point: Atria and ventricles are relaxed in mid-to-late diastole. 2. Ventricular filling: AV valves are open in mid-to-late diastole, semilunar valves are closed, ventricles begin to fill (70% occurs prior to atrial contraction), atrial systole in which atria contract (preceded by P wave) and increased atrial pressure propels blood from atria into ventricles. Atria relax and ventricles depolarize (QRS wave). 3. Ventricular systole: As contraction begins, intraventricular blood pressure increases, AV valves close and semilunar valves are also closed. This is called isovolumetric contraction phase (because volume is constant). Blood pressure in aorta and pulmonary trunk exceeds intraventricular pressure. Pressure in ventricles increases without volume changing. Ventricular ejection phase occurs when intraventricular pressure exceeds pressure in large vessels, semilunar valves open and blood is propelled out of ventricles. Atria begin to fill with blood. 4. Isovolumetric relaxation occurs during early diastole along with T wave. Ventricles relax, intraventricular pressure drops, blood in vessels outside heart begins to flow back into ventricles. Semilunar valves close, aortic pressure increases while AV valves still closed resulting in isovolumetric relaxation. 5. AV valves open when pressure in atria exceeds pressure against AV valves exerted by blood in ventricles. Start of another cycle with quiescent period. -7- Lectures' headings for dental students: CVS Heart Sounds Associated with closing of heart valves (Lub-dub, pause lub-dub, pause, …). Sounds of separate valves can be differentiated. Timing: Mitral then Tricuspid then Aortic semilunar then Pulmonary semilunar. Sound 1: AV valves close, onset of systole, louder and longer than sound 2 Sound 2: Semilunar valves close, beginning of ventricular diastole, short, sharp sound Pause: Quiescent period -8- Lectures' headings for dental students: CVS Cardiac Output (CO) Cardiac Output is the amount of blood pumped by each ventricle per minute. CO = Stroke volume X Heart rate. Stroke volume = volume of blood pumped out of each ventricle per beat. Cardiac output increases or decreases with increases or decreases in either stroke volume or heart rate (HR) Stroke volume (SV) is the difference between end diastolic volume (EDV) and end systolic volume (ESV). Normal EDV = 120 ml and is increased with the increase in length of ventricular diastole and venous pressure and vice versa. Normal ESV = 50 ml and is increased with the increase in arterial pressure and decreased with force of ventricular contraction. Factors that affect stroke volume 1. Preload: Degree of stretch prior to contraction is the most important factor affecting EDV. The greater the stretch of cardiac fibers, the greater the force of contraction. Factors increasing stretch are volume and speed of venous return. In the other hand, increasing heart rate reduces time for filling and decreases stretch. 2. Contractility: Is an increase in contractile strength independent of muscle stretch. Increase Ca2+ into cardiac cells increases contractility and volume ejected from heart and decreases ESV. 3. Afterload: Arterial blood pressure (BP) is the pressure that ventricular contraction must overcome (back pressure in aorta and pulmonary valves). Normal BP = 80 mm Hg (aorta) and 10 mm Hg (pulmonary trunk). It is not normally a factor in healthy individuals but may have an adverse effect in individuals with hypertension. -9- Lectures' headings for dental students: CVS Heart Rate regulation Cardiac output is homeostatically regulated: A. Neural mechanisms B. Chemical mechanisms C. Physical mechanisms - 10 - Lectures' headings for dental students: CVS A. Neural mechanisms: Autonomic nervous system: i. Sympathetic division: Pacemaker cell resting membrane potential is brought closer to threshold (depolarized), increases heart rate, increases Ca2+ influx into contractile cells, decreases ESV. ii. Parasympathetic division: Opposes the effects of sympathetic division, decreases heart rate, mediated by acetylcholine, hyperpolarizes (inhibits) SA node. Vagal tone means that sympathetic and parasympathetic divisions are continuously active. Effect of parasympathetic division predominates. Its effect is reduced activity of AV node (25 beats/min reduction in HR). B. Chemical regulation: 1. Hormones of adrenal medulla: Epinephrine increases HR and contractility (like nor epinephrine). 2. Decreased Ca2+ concentrations cause depressed heart function and increased Ca2+ concentrations cause heart irritability C. Physical factors: 1. Age: Inverse relation. 2. Gender: Female faster. 3. Exercise: Increased HR during exercise, resting rate is lower. SV and muscle mass increased in athlete. 4. Body temperature: HR lowered when cold. - 11 - Lectures' headings for dental students: CVS Cardiovascular System II: Blood Vessels Arterial blood vessels are classified based on size and function into: 1. Elastic (conducting) arteries: Thick-walled, near heart, largest diameter, more elastic and large lumen. They dampen blood pressure (BP) changes associated with heart contraction. This passive accommodation results in smooth flow of blood. Diameter is about 1.0 - 2.5 cm 2. Muscular arteries (distributing arteries): Distal to elastic arteries, deliver blood to specific organs, with thick media layer (i.e. more smooth muscle). Diameter is about 0.3 - 1.0 cm. 3. Arterioles: Determine flow into capillary beds, mostly smooth muscle of about 10 µm-0.3 cm diameter 4. Capillaries: Smallest blood vessels 8 - 10 µm with tunica interna only aid in exchange of materials. Capillaries act as networks (capillary beds) as a microcirculation from arteriole to venule. Types of capillary 1. Continuous: Uninterrupted endothelial cells, incomplete tight junctions with intercellular clefts 2. Fenestrated: Endothelial cells have oval pores (fenestrations=windows) permit greater permeability 3. Sinusoidal: Modified, leaky capillaries that large molecules can pass through Venous System 1. Venules: 8 - 100 µm, characteristics vary with size, little muscle and thin externa 2. Veins: Formed from venules, thinner walls and less muscle than arteries, little muscle in media (mostly elastin) and externa is the thickest wall layer. Veins act as reservoirs with large lumens (capacitance vessels) and low blood pressure allows walls to thin. Venous valves are folds of interna prevent backflow. - 12 - Lectures' headings for dental students: CVS Physiology of Circulation Blood Flow (F) = ∆P/PR Blood flow: Is the volume flowing through a given structure per unit time (ml/min). Blood pressure: Is the force per unit area (mm Hg). Resistance: Is the opposition to flow; generally encountered in the systemic circuit (PR = peripheral resistance) Sources of resistance: i. Blood viscosity: Is the thickness related to formed elements ii. Total vessels length: Longer vessels result in greater resistance iii. Diameter: Flow is inversely related to vessels diameter; larger diameter results in less resistance (1/r4). In healthy humans, diameter is the greatest source of resistance Systemic blood pressure: Heart pumping generates blood flow. Pressure results when flow opposed by resistance. Blood flows along a pressure gradient from higher to lower pressure. It is highest in aorta and lowest in right atrium. - 13 - Lectures' headings for dental students: CVS Factors affecting arterial pressure near heart: a. Stretching of arteries: Compliance or distensibility. b. Volume of blood forced into the arteries. Changes associated with systole: Aorta is stretched by kinetic energy of blood leaving left ventricle. Blood moves toward periphery because peripheral pressure is lower than aortic pressure (systolic blood pressure SBP = 120 mm Hg). Changes associated with diastole: Semilunar valve closes, aorta recoils and pressure is maintained by reducing volume (diastolic blood pressure DBP = 70 - 80 mm Hg). Pulse pressure(PP) = SBP minus DBP. Mean arterial pressure (MAP) = DBP + 1/3 PP. Capillary blood pressure is 40 mm Hg entering and 20 mm Hg exiting while venous blood pressure relatively steady throughout cardiac cycle (20 mm Hg) with gradient from venules to vena cava. Venous pressure is too low to promote adequate return so, it needs additional functional modifications. These functional modification are: a. Respiratory pump: Abdominal (ventral body cavity) pressure increases squeeze local veins while backflow is prevented by valves. So, blood is forced toward the heart. At the same time, chest cavity pressure decreases and thoracic veins expand. So, blood enters right atrium. b. Muscular pump (more important): Contraction of skeletal muscle surrounding veins compress vein and, again, backflow is prevented by valves. So, blood moves in direction of heart. Regulation of Blood Pressure Blood pressure = Cardiac output X Peripheral resistance Factors that enhance CO are: 1. Reduced parasympathetic (vagal) control: HR increases 2. Increased sympathetic activity: Increases contractility of heart, reduces ESV and increases stroke volume. Sympathetic activity releases epinephrine (EPI) into blood stream from adrenal medulla which increases heart rate 3. Increased activity of respiratory and muscular pumps: Increases venous return, EDV and stroke volume - 14 - Lectures' headings for dental students: CVS Neural control of blood pressure (short-term mechanisms): Nervous control of peripheral resistance alter blood distribution and/or alter blood vessel diameter via vasomotor center, baroreceptors and chemoreceptors: -Vasomotor center in medulla oblongata regulates blood vessel diameter. Vasomotor fibers are sympathetic efferents that innervate smooth muscle of blood vessels (mainly arterioles) releasing nor-epinephrine (NE) which is a strong vasoconstrictor. Vasomotor tone is a tonic vasoconstriction. -Baroreceptors: Are pressure sensitive mechanoreceptors located in carotid sinuses, aortic arch and walls of all large vessels and detect changes in arterial blood pressure. When BP rises, receptors are stretched and stretching increases signaling to vasomotor center which inhibits vasomotor center causing dilation of arteries and veins. Arteriole dilation reduces peripheral resistance while venodilation shifts blood to venous reservoirs so that venous return decreases and hence, cardiac output declines. Baroreceptors also send efferent signals to cardiac centers in the medulla which inhibit sympathetic NS and stimulate parasympathetic NS. So, HR and contractile force decrease. Baroreceptors respond to acute changes in blood pressure. Carotid sinus reflex protects blood supply to brain and aortic reflex maintains supply to systemic circuit. -Chemoreceptors: Are located in carotid and aortic arch and carotid sinus and respond to changes in O2 and CO2 concentrations and pH. They are primarily involved in control of respiratory rate and depth. - 15 - Lectures' headings for dental students: CVS Chemical control of blood pressure(short term mechanisms) a. Adrenal medulla hormones: NE and EPI. NE is a vasoconstrictor. EPI increase cardiac output by increasing cardiac muscle contractility b. Atrial natriuretic peptide (ANP): Atrial peptide hormone reduces blood pressure by antagonizing aldosterone. It increases water excretion from kidney. c. Antidiuretic hormone (ADH): Is a posterior pituitary hormone increases blood pressure by increasing water absorption by distal tubule. At high concentrations, it causes vasoconstriction d. Angiotensin II: Mediated by release of renin by JGA of kidney tubule. When amount of blood entering kidney tubule is too low, renin is released. Renin catalyzes the conversion of angiotensinogen into angiotensin II. Angiotensin II causes vasoconstriction of systemic arterioles. It increases BP and also causes release of aldosterone from adrenal cortex and aldosterone in turn increases absorption of water by kidney tubules e. Endothelium-derived factors: Endothelin and prostaglandin are vasoconstrictors and nitrous oxide (NO) is a fast acting local vasodilator f. Inflammatory chemicals (vasodilators): e.g. histamine increases capillary permeability g. Alcohol: reduces blood pressure, inhibits ADH release (increases loss of water in urine) and increases vasodilation (skin) by depressing vasomotor center - 16 - Lectures' headings for dental students: CVS Renal regulation of blood pressure (long-term mechanisms for blood pressure regulation) -Kidney controls blood volume by regulating water loss in urine. -Blood volume affects cardiac output via venous pressure, venous return, EDV and stroke volume. -Blood pressure change parallels change in blood volume. Kidney responds by eliminating water to reduce volume or by absorbing water to increase volume. -Direct action of the kidney is the alteration to rate of fluid filtration from blood stream to kidney tubules. Increased BP increases amount of filtrate entering tubules. Filtrate entering is greater than the amount that can be processed. Fluid leaves body in the form of urine. Blood volume decreases and therefore BP also decreases. -Indirect renal mechanisms: Renin-angiotensin mechanism. Aldosterone also causes Post. Pituitary to release ADH which promotes water reabsorption by kidney. - 17 - Lectures' headings for dental students: CVS Tissue Perfusion Blood flow is distributed to body tissue in an exacting fashion. At rest, brain receives13%, heart 4%, kidneys 20% and abdominal organs 24%. While during exercise, blood flow to the skin, muscles and heart increase and remaining tissues either remains the same or decreases. Blood flow velocity is inversely proportionate to cross-sectional area of blood vessels to be filled. Aorta has a cross-sectional area (2.5 cm2) and an average velocity of 40-50 cm/s. Capillaries have a total cross-sectional area of 4500 cm2 and a very slow flow (0.03 cm/s). Blood flow through individual organs is intrinsically controlled (i.e., autoregulation). Diameter of arterioles feeding a given organ is controlled by that organ. The intrinsic control mechanisms are metabolic controls and myogenic controls. In metabolic controls, levels of nutrients, particularly oxygen, act as autoregulation stimuli. In myogenic controls, excessive or inadequate blood pressure stimulate myogenic responses otherwise they can damage or cause the death of an organ. - 18 -