* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Herpes Simplex Virus Blepharoconjunctivitis
Transmission (medicine) wikipedia , lookup
Public health genomics wikipedia , lookup
Compartmental models in epidemiology wikipedia , lookup
Canine parvovirus wikipedia , lookup
Marburg virus disease wikipedia , lookup
Focal infection theory wikipedia , lookup
Infection control wikipedia , lookup
Index of HIV/AIDS-related articles wikipedia , lookup
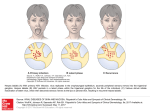
Herpes Simplex Virus Blepharoconjunctivitis Deborah Gill, MD; Todd P. Margolis, MD, PhD—Guest Authors Rosalyn Stewart, MD, MS, FAAP, FACP Leonard Feldman, MD—Column Editors Herpes simplex virus (HSV) blepharoconjunctivitis is characterized by a vesicular rash, tender preauricular adenopathy, and follicular conjunctivitis. It is important to realize that the classic vesicular rash is frequently crusted over by the time the patient is evaluated. The clinical findings may be much more subtle than those seen in Figure 1. Figure 1. HSV corneal infection most commonly presents as a dendriform epithelial keratitis. Fluoresceine dye reveals the extent of the corneal surface affected (Figure 2) whereas Rose Bengal (or lissamine green) identifies actively infected epithelial cells at the leading edge of the infection. Sensation is usually markedly reduced in the affected portion of the cornea. Figure 2. HSV infection of the corneal stroma (stromal keratitis) is the most common cause of infectious corneal blindness in the United States (Figure 3). Because this disease can present in a number of different patterns and without a prior history of HSV ocular disease, clinicians must have a high index of suspicion that any form of corneal inflammation or scarring may be due to HSV. Figure 3. Patients with a history of atopy appear to have a greater risk for Figure 4. Figure 5. recurrent and severe herpes simplex virus (HSV) ocular disease, and this severity may manifest in different forms (Figures 4 and 5). Furthermore, these patients often require more aggressive antiviral therapy than do patients without atopic disease. Antiviral agents are used to treat HSV lid disease, conjunctivitis, and epithelial keratitis. Systemic medications, such as acyclovir (400 mg by mouth, 5 times/day), are as effective as topical agents and are generally better tolerated. Stromal keratitis and iritis also require the use of topical corticosteroids, which should never be used without antiviral coverage. Because HSV keratitis can lead to blindness, all patients with any manifestation HSV infection in or around the eye should be promptly referred to an ophthalmologist. Dr Gill is a clinical and research fellow with the Proctor Foundation and Department of Ophthalmology. Dr Margolis is Professor of Ophthalmology, University of California, and Director of the F. I. Proctor Foundation, San Francisco, California. Dr Stewart is Assistant Professor, Department of Medicine, Division of General Internal Medicine, Johns Hopkins University, Baltimore, Maryland. Dr Feldman is Instructor of Medicine, Department of Medicine, Division of General Internal Medicine-Hospitalist Service; Assistant Program Director, Osler Medical Residency; Director, Comprehensive General Medicine Consult Service, Johns Hopkins Hospital, Johns Hopkins University, Baltimore, Maryland. Johns Hopkins Advanced Studies in Medicine 289