* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 1. Syphilis
Microbicides for sexually transmitted diseases wikipedia , lookup
Toxoplasmosis wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Herpes simplex wikipedia , lookup
West Nile fever wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Onchocerciasis wikipedia , lookup
Tuberculosis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Marburg virus disease wikipedia , lookup
Trichinosis wikipedia , lookup
Leptospirosis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Hepatitis B wikipedia , lookup
Hepatitis C wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Sarcocystis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Schistosomiasis wikipedia , lookup
Neonatal infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Tuskegee syphilis experiment wikipedia , lookup
History of syphilis wikipedia , lookup
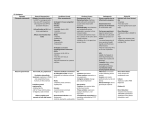
Go Back to the Top Chapter 27 To Order, Visit the Purchasing Page for Details Sexually Transmitted Diseases Diseases whose main transmission route is sexual intercourse or sexual activity are generically called sexually transmitted diseases (STD). Syphilis, chancroid, lymphogranuloma venereum, and gonorrhea, as well as genital herpes, condyloma acuminatum, scabies and pediculosis pubis are the most common STDs. The rapidly increasing number of STD cases has become a serious social issue. This chapter introduces the STDs that are not discussed in other chapters, such as syphilis, chancroid and lymphogranuloma venereum. 1. Syphilis Outline ● The causative bacterium is the spirochete Treponema pallidum. ● The various mucocutaneous symptoms include ulceration in the genitalia and eruptions on the whole body. ● In primary syphilis (that in the first 3 months after infection), primary lesions in the genitalia, ulcerative hard chancre and regional lymph node enlargement occur. ● In secondary syphilis (that up to 3 years after infection), syphilitic roseola, papular syphilide, condylomata lata and syphilitic alopecia occur. ● Secondary syphilis recurs every several months, with asymptomatic intermissions (latent syphilis). ● In tertiary syphilis (that more than 3 years after infection), syphilis nodosa and gumma occur in the skin. As systemic symptoms, neurological and cardiovascular symptoms occur. ● There is no primary syphilis in congenital syphilis (transplacental infection). ● Diagnosis is made by detection of the pathogenic microbe and serologic test. Penicillin antibiotics are useful for treatment. Classification, Pathogenesis Syphilis is caused by the spirochete Treponema pallidum. The route is contact infection (acquired syphilis) or intrauterine infection (congenital syphilis). Acquired syphilis is caused by sexual activity in most cases; however, it may be transmitted in healthcare workers non-sexually through work. In rare cases, syphilis may be transmitted by transfusion or by mother-to-child transmission from birth canal infection or breast feeding. Clinical features Syphilis is divided into manifest syphilis and asymptomatic syphilis. In manifest syphilis, lesions occur on the skin and mucosa membranes. Asymptomatic syphilis progresses gradually 493 27 494 27 Sexually Transmitted Diseases Primary Secondary/Latent Primary syphilis Tertiary Secondary syphilis Tertiary syphilis 3 months ②hard chancre Asymptomatic period ( Serological test (+) ①fever, fatigue ②syphilitic roseola ③papular syhilide ④condylomata lata (mucous lesion) ↑ ③cardiovascular syphilis ④neurosyphilis Serological (+) 3 months 6 weeks 3 weeks infection ②gumma 10 years ∼ Serological (-) ①syphilis nodosa Recurring secondary syphilis and latent syphilis every several months. 3 years ③bubo indolenta ∼ Incubation (asymptomatic) period ( 3 weeks) ︶ ①primary lesion Fig. 27.1 Clinical course of syphilis. and symptoms are not apparent. The course of syphilis is divided into four stages: primary, secondary, latent and tertiary (Fig. 27.1). Primary syphilis is highly infectious; tertiary syphilis is not. Congenital syphilis has a specific course. Syphilis was thought to occur as manifest syphilis in various degrees in all syphilis-infected individuals; however, the infection remains latent in many cases. Clinical images are available in hardcopy only. Fig. 27.2 Primary lesion. A firm, asymptomatic papule with a diameter of 2 cm occurred on the border of the glans penis and foreskin. 1) Primary syphilis After the initial incubation period of 3 weeks, a firm papule of 1 cm to 2 cm in diameter occurs at the site invaded by the spirochete (Fig. 27.2), gradually ulcerating into a hard chancre. Numerous Treponema pallidum organisms are observed on the surface of the hard chancre by microscopy. Several days after the primary chancre, firm painless enlargement of the regional lymph node occurs, which is called bubo indolenta. These asymptomatic changes often go unnoticed by the patients. The eruption heals spontaneously in about 3 weeks, after which is no skin manifestation for 2 to 6 weeks until occurrence of an eruption in secondary syphilis. 2) Secondary syphilis 27 The period from the third month (to the third year) after infection is secondary syphilis. The Treponema pallidum organisms that have proliferated in the regional lymph node at primary syphilis disseminate hematogenously to the whole body, leading 495 1. Syphilis to various asymptomatic eruptions. Antibody titer becomes highest at this stage and decreases thereafter. The eruptions recur and disappear repeatedly for several years. Although eruptions first occur symmetrically on the whole body, they gradually become localized asymmetrically. The main symptoms of the secondary syphilis are the following. ① Syphilitic roseola Multiple, asymptomatic, light pink erythema of 5 mm to 20 mm in diameter occur on the whole body surface, markedly on the palms and soles (Fig. 27.3). These are accompanied by slight fever and systemic fatigue. The skin lesion disappears in several days. ② Papular syphilide Two to 3 weeks after the onset of syphilitic roseola, multiple, vivid red papules of 5 mm to 10 mm in diameter appear, most frequently on the trunk (Fig. 27.4), and most severely on the palms and soles. It is asymptomatic. ③ Papulosquamous eruption (Syphilitic psoriasis) Localized psoriasis-like eruptions occur on the palms and soles; they are highly diagnostic for syphilis. ④ Condylomata lata Highly infectious, moist, flatly elevated papules with a dirty appearance appear on the intertriginous areas of the anus, genitalia, axillary fossae and inframammary region (Fig. 27.5). Treponema pallidum organisms are observed in high concentration in the lesions. a ⑤ Pustular syphilide Multiple pustules occur. Papular syphilide may progress to pustular syphilis in some cases. Immunocompromised patients are most likely to be affected. ⑥ Syphilitic leukoderma It is vaguely demarcated, incompletely hypopigmented leukoderma. It occurs in patients who have darkly pigmented skin. ⑦ Syphilitic paronychia This paronychia is associated with syphilis. There are no clinically characteristic findings in syphilitic paronychia. ⑧ Syphilitic alopecia Six months after infection, multiple patches of hair loss of 5 mm to 20 mm in diameter appear and spread gradually on the entire scalp. It should be differentiated from alopecia areata. ⑨ Syphilitic angina A highly infectious mucosal lesion accompanied by tonsillitis occurs in the oral cavity (Fig. 27.6). Clinical images are available in hardcopy only. a b c d e f g h h i Clinical images are available in hardcopy only. b c d e f g Fig. 27.3 Syphilitic roseola. a: Erythema up to 1 cm in diameter that is slightly infiltrative at the edge, on the palms. b: Closeup of lesion in another case. The erythema is partially infiltrative. Both cases are secondary syphilis. 3) Latent syphilis Untreated secondary syphilis may resolve in 3 to 12 weeks, leaving the patient asymptomatic. Diagnosis can be made by a positive serology test without any clinical evidence of treponemal infection. Latent syphilis is divided into an early latent stage (within 1 year after onset of disease) and a late latent stage (1 year after onset of disease). 27 496 27 Sexually Transmitted Diseases 4) Tertiary syphilis Clinical images are available in hardcopy only. Clinical images are available in hardcopy only. In tertiary syphilis, Treponema pallidum is difficult to detect during the period of 3 to 10 years after infection. Multiple, copper-colored nodules of several centimeters in diameter appear on the face at the early stage of tertiary syphilis and heal with scarring in several months (syphilis nodosa). A few subcutaneous nodules occur, soften and rupture, forming ulcers (gumma). These eruptions are rarely seen today, thanks to improved treatments using antibiotics. After 10 years or more of infection, eruptions are no longer seen. However, the heart, blood vessels and central nervous system become involved (metasyphilis). The main symptoms are myocarditis, aortic aneurysm, myelophthisis and general paresis. Syphilis today rarely progresses to this stage. 5) Congenital syphilis Fig. 27.4 Syphilis papulosa. Multiple, bright red papules of 5 mm to 10 mm occur. They are accompanied by infiltration. Clinical images are available in hardcopy only. Treponema pallidum passed through the placenta from the mother infects the child. Intrauterine infection in early pregnancy may result in stillbirth or miscarriage. Therefore, congenital syphilis is usually caused by infection after the first trimester, when the placenta is completely formed. The infection is systemic and hematogenous; congenital syphilis begins with secondary syphilis and without primary syphilis. Within 6 months after birth, symptoms of secondary syphilis appear (early congenital syphilis). Symptoms of tertiary syphilis appear after late childhood (late congenital syphilis). In early congenital syphilis, premature facial aging, radial scarring around the mouth called Parrot’s furrow, syphilitic nephritis, and pseudoparalysis from the sharp pain of osteochondritis (Parrot’s pseudoparalysis) are present. In late congenital syphilis, Hutchinson’s triad (dental abnormality, ocular interstitial keratitis, impairment of vestibulocochlear nerve) becomes pronounced. Pathology Swelling and proliferation of the vascular endothelium and perivascular infiltration of plasma cells and lymphocytes are observed by skin biopsy of a syphilitic eruption. Central caseation necrosis of the eruption and granulomatous infiltration are found after second syphilis. Fig. 27.5 Condylomata lata. Multiple, flatly elevated infiltrative eruptions, these coalesce in some areas. 27 Laboratory findings, Diagnosis Treponema pallidum is investigated by microscopy and serologic test. Because Treponema pallidum cannot be cultured, specimens are collected and directly investigated by microscopy from moist lesions such as a hard chancre, condylomata lata, enanthema in the oral cavity, or pustules. Treponema pallidum stains bluish black in parker ink and shines in dark-field examination. Serological test is useful for finding, screening and judging the progression of syphilis. Nevertheless, the test is negative in the 2. Chancroid 4th to 6th week after infection. The main examinations are serologic test for syphilis (STS) using lipid antigen (cardiolipin), treponemal hemagglutination (TPHA) test, and fluorescent treponemal antibody absorption test (FTA-ABS). The STS results show positive at the early stages of infection, and the elevation of antibody titer closely relates to the disease progression. STS is effective for screening and is used as an index of therapeutic performance. However, STS may show false positive in patients with other disorders, such as collagen disease. Called biological false positive (BFP), it is useful for diagnosis of lupus erythematosus and antiphospholipid syndrome. Because of its high specificity, TPHA and FTA-ABS are used to confirm the diagnosis for individuals who show positive by STS screening. STS and TPHA are compared in Table 27.1. The incidence and progression of syphilis are determined by the combination of TPHA and FTA-ABS. 497 Clinical images are available in hardcopy only. Fig. 27.6 Syphilitic angina. Treatment Penicillin antibiotics are the first-line treatment. Penicillin-resistant strains have not been found so far. In the late stages of syphilis, the same treatments for early syphilis are repeated every 6 months; nonetheless, the disease tends to be intractable at that stage. Macrolide or tetracycline drugs are given to patients with penicillin hypersensitivity. Although administration of antibiotics at the early stage kills Treponema pallidum quickly and effectively, the residue of dead Treponema pallidum may cause toxic reaction; within several hours of drug intake, a fever of about 40˚C occurs and the syphilis eruptions aggravate (Jarisch-Herxheimer reaction). NSAIDs are administered for this phenomenon. Aqueous penicillin administered by large-bore IV is recommended for neurological syphilis, because oral and intramuscular administration of penicillin fail to reach the cerebrospinal fluid in sufficient concentration. For the reason that HIV carriers may fail to respond well to treatment, larger doses of drugs based on the same treatment for neurological syphilis may be necessary for a prolonged period. Reinfection of Treponema pallidum may occur in some cases. Serologic test for syphilis MEMO (STS) As described in the text, STS is a nontreponemal screening test using cardiolipin. Several tests have been used which are categorized into STS. ・Glass slide test (venereal disease research laboratory (VDRL)) ・Rapid plasma reagin card test (RRR) ・Complement fixation test ・Wassermann test ・Kahn’s test 2. Chancroid Pathogenesis, Epidemiology Chancroid is an infection caused by the Streptobacillus Haemophilus ducreyi and transmitted by sexual activity. This Gram-negative bacillus stains well in Unna-Pappenheim. Chancroid is most common in tropical and subtropical countries. Clinical features Two to three days after infection, a red papule occurs on the coronal sulcus, foreskin, labium or vaginal opening and becomes pustular, leading to ulceration. The ulcer is accompanied by severe pain and a pustular coat in the center. The ulcer is soft to the Go Back to the Top MEMO Sexually transmitted superinfection of HIV and syphilis has been increasing. Syphilis patients who are immunocompromised from HIV infection are prone to severe symptoms of secondary syphilis. Those cases are often difficult to cure by the usual syphilis treatments. The spread of neurologic syphilis in HIV-positive patients has become a serious problem. HIV-positive patients may have atypical clinical findings of syphilis, serological findings and response to treatments. HIV and syphilis To Order, Visit the Purchasing Page for Details 27