* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download MR guidance in radiotherapy
Survey
Document related concepts
Transcript
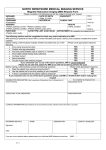
Home Search Collections Journals About Contact us My IOPscience MR guidance in radiotherapy This content has been downloaded from IOPscience. Please scroll down to see the full text. 2014 Phys. Med. Biol. 59 R349 (http://iopscience.iop.org/0031-9155/59/21/R349) View the table of contents for this issue, or go to the journal homepage for more Download details: IP Address: 176.9.124.142 This content was downloaded on 21/10/2014 at 14:06 Please note that terms and conditions apply. Institute of Physics and Engineering in Medicine Phys. Med. Biol. 59 (2014) R349–R369 Physics in Medicine & Biology doi:10.1088/0031-9155/59/21/R349 Topical Review MR guidance in radiotherapy Jan J W Lagendijk, Bas W Raaymakers, Cornelis A T Van den Berg, Marinus A Moerland, Marielle E Philippens and Marco van Vulpen Department of Radiotherapy, University Medical Centre Utrecht, Heidelberglaan 100, Utrecht, The Netherlands Received 7 February 2014, revised 20 May 2014 Accepted for publication 28 July 2014 Published 16 October 2014 Keywords: MRI, radiotherapy, adaptive, imaging (Some figures may appear in colour only in the online journal) 1. Introduction The use of modern MRI technology in radiotherapy is fast growing. MRI is entering all facets of radiotherapy. This review will start with a very short overview of the newest developments in MRI technology after which it will cover, in separate paragraphs, the various radiotherapy related topics: •Developments MRI technology •Tumour visualisation, characterization and response assessment for Radiotherapy •Treatment simulation •MRI guidance for brachytherapy •MRI guidance for external beam radiotherapy This review will serve as a short introduction to this wide field. The focus will lie on the new development of MRI guidance of the actual therapy. 2. Developments MRI technology Magnetic resonance imaging (MRI) has become, over the last 30 years, one of the main pillars of modern diagnostic imaging, which is widely used for many clinical problems. One of the reasons for its success is the high level of technical innovation which has turned modernday MRI into a versatile medical imaging modality (Haacke et al 1999). MRI stands out in terms of soft tissue visualization. MRI does not require ionizing radiation. In addition, it provides several functional imaging modalities for measuring biological function and physiology. Throughout its relatively short history the strive for higher magnetic field strength has been a constant factor from 0.5 T MR scanners in the eighties to 1.5 and 3 T MR scanners in current clinics. A higher magnetic field strength is favourable as it leads to higher signal-to-noise 0031-9155/14/21R349+22$33.00 © 2014 Institute of Physics and Engineering in Medicine Printed in the UK & the USA R349 Topical Review Phys. Med. Biol. 59 (2014) R349 ratios that can be traded off for higher spatial resolution or imaging speed. In addition, various functional imaging contrasts such as Blood Oxygen Level Dependence (BOLD) are augmented by the higher magnetic field strength (Ogawa et al 1993, Donahue et al 2011). At the moment, 7 T MRI forms the forefront of this quest for higher field strength and recently 7 T neuro-imaging has produced remarkable results, which provide new insight into brain anatomy and function (van Veluw et al 2013). Another technological aspect that has played a key role in the advancement of MRI is the use of multi-detector receive. While in the early days, a single surface loop was used for signal reception, a modern MR scanner employs 32 or even 64 receive channels connected to dedicated multi element detectors (receive coil arrays) geometrically tailored to the scanned body part. A phased array operation of such a multi-channel detector allows for maximum signal reception and minimization of noise contamination of the signal (Roemer et al 1990). A very recent trend is digitalization of the signals on the detector, which are then passed to the image reconstructor by optical fibres minimizing electronic distortions and RF loss (Possanzini et al 2011). Vendors have integrated this digital technology into new generation 1.5 and 3 T MR scanners with greater bore sizes going from 60–70 cm bore diameter. This is relevant for radiotherapy purposes and the extra space allows scanning patients in radiotherapy treatment postures. Although MRI cannot yet compete with multi-detector CT imaging, in terms of acquisition speed, it has made vast progress in image acceleration. The above mentioned development of parallel imaging technology was a key step and allows for sub-Nyquist undersampling of k-space by exploiting the different receive sensitivity patterns of the receive channels to unfold the otherwise aliased images of the different channels into one unfolded image (Sodickson et al 2005, Pruessmann 2006). A more recent trend to accelerate image acquisition is the use of compressed sensing methodology, which has been very successful when applied to various MR imaging techniques (Lustig et al 2007). Today, very rapid advancements are being achieved in functional imaging of the brain where new multi-slice, multi-band imaging technology allows high resolution, whole brain images in a few seconds (Larkman et al 2001, Breuer et al 2005). Neuro-science is the main driver behind the development of various new MR imaging technologies. MR imaging of the brain is relativity easy due to minimal motion compared to thoracic, abdominal and pelvic organ sites. Abdominal and thoracic MR imaging faces more severe challenges due to cardiac and respiratory induced motion that can result in a variety of artefacts. Especially cardiac MR imaging, which played a pioneering role in the development of strategies to mitigate or correct patient motion (Lanzer et al 1984). Navigator echo techniques were developed to reduce such artefacts allowing for the monitoring and correcting of motion during MR acquisitions by tracking the movement of objects in real time (Ehman and Felmlee 1989, Stam et al 2012). Other acquisition strategies to address patient motion include the use of breath holds and gated acquisitions (Runge et al 1984). By gating the MR acquisition on the ECG or respiratory signal, artefact free MR images can be made of several phases of the cardiac and respiratory cycle (Ehman et al 1984, Lewis et al 1986). Such sequences allow for new detailed imaging of body locations like the oesophagus, pancreas and kidneys (figure 1). 3. Tumour visualisation, characterization and response assessment for radiotherapy In radiology the diagnostic performance of an imaging method is leading. In contrast, for radiotherapy treatment planning accurate tumour delineation is the most important factor. Therefore, first robust imaging with high resolution and high contrast between tumour and surrounding normal tissue is required. R350 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 1. Example MRI oesophagus tumour, improvement image quality using cardiac triggering and breath hold (reproduced with permission from van Rossum et al 2013). Since all directions, left–right, anterior–posterior and cranial–caudal are equally important for treatment planning and delivery, spatial resolution is important and preferably isotropic, 3-dimensional (3D) MR images should be used. An additional advantage of 3D MRI is the improved signal to noise ratio. However, this is generally at the cost of increased motion sensitivity and increased acquisition time. Steady state free precession (SSFP) acquisition methods are most appropriate for fast, high resolution acquisition and are geometrically robust (Patz and Hawkens 1986). The disadvantage is that these sequences show a mixed T1 and T2 contrast and are susceptible to magnetic field (B0) inhomogeneities, which may lead to banding artefacts (Hargreaves 2012). Fast spin echo methods show a better defined contrast, are intrinsically corrected for B0 inhomogeneities, but are more time consuming and sensitive to blurring due to long decaying echo trains (Reichenbach et al 1997, Markl and Leupold 2012). A special acquisition method is the echo planar imaging (EPI) read out. This acquisition method is the workhorse for fMRI brain studies and diffusion weighted imaging, allowing very fast data collection with excellent SNR performance (Bammer 2003). The application in radiotherapy, however, is far from ideal due to its extreme sensitivity to B0 inhomogeneities, causing large geometric distortions, especially in areas with air-tissue contrasts, such as head and neck (Le Bihan et al 2006, Schakel et al 2013). For abdominal and thoracic organs, respiratory induced motion deteriorates MR images and imaging motion artefacts have to be resolved for accurate tumour visualization. The simplest method is to apply breath-holds. However, breath-holds elongate measurement time and restrict image resolution due to the limited acquisition time available per breath hold (Low 2007, Wielpütz and Kauczor 2012). Further, breath-hold positions are poorly reproduced, which will lead to discontinuities in the image. A more patient friendly approach is to apply respiratory triggering either using MR navigators or with an external respiratory pressure belt (Oechsner et al 2009). This enables data acquisition in a consistent phase of the breathing cycle and prevents motion artefacts in the images. Using these techniques, tumours in the pancreas, liver and stomach are imaged successfully (Marin et al 2010). A comparable procedure, using cardiac triggering, can be applied to correct for cardiac motion while measuring thoracic lesions, like the oesophageal cancer or mediastinal lymph nodes (Riddell et al 2007) Besides high resolution, high tumour-background contrast is also needed to accurately delineate tumour volumes. Figure 2 gives a visualization example of a Gd-enhanced T1-weighted MRI of a hypopharyngeal carcinoma. The strength of MRI is that different R351 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 2. Computed tomography image (left) of a patient with a T2N2bM0 hy- popharyngeal carcinoma, compared with a Gd-enhanced T1-weighted MR image (right) at the same location (reproduced with permission from Verduijn et al 2009). endogenous contrasts can be created by manipulation of the pulse sequences parameters (Plewes and Kucharczyk 2012). The most important independent contrast mechanisms are T1 and T2 relaxation and water diffusion (Bottomley et al 1987). Both native T1 and T2 contrasts are useful to distinguish solid tumours from normal tissue, depicting water content and chemical environment. The additional contrast is apparent between water and fat containing tissues, which helps to define tumour boundaries. In the head and neck, squamous cell carcinoma appear slightly darker on a T1 weighted image (Becker et al 2008a). For oesophageal and rectal tumours, T2 weighted images are vry useful to distinguish the tumour from normal rectal, oesophageal tissue surrounding fat (Beets-Tan and Beets 2012). Tumours can be surrounded by oedema due to peritumoral inflammation or due to restricted venous and lymph drainage (Becker et al 2008b). This effect is apparent in head and neck tumours, where the area with high signal on T2 is, for the most part, largely overestimating the gross tumour volume (Caldas-Magalhaes et al 2012). Another endogenous contrast is T2*, which reflects the induced (microscopic) field inhomogeneities due to e.g. deoxyhemoglobin. BOLD imaging is based on this mechanism where deoxyhemoglobin causes a decrease in T2*. Since the amount of deoxyhemoglobin is dependent on the amount of blood and the oxygenation of blood, BOLD MRI might indicate the oxygenation status of a tumour (Hoskin et al 2007). Improved estimation of the oxygenation status can be achieved using D(C)O2E MRI which requires respiratory challenges of CO2 and O2 (Rijpkema et al 2002). An important physiological characteristic of most tumours is the impaired vasculature due to imbalanced angiogenesis. To measure altered micro-vascular parameters, an exogenous contrast agent is injected and its tissue uptake monitored by (repeated) imaging, which results in information on blood volume and flow. Commonly, gadolinium chelates contrast agents are used. These contrast agents decrease the T1 relaxation of water protons and thereby affect T1 based contrast in blood and in tissue due to contrast agent leakage (Padhani and Dzik-Jurasz 2004). An alternative technique used to assess blood volume and flow is Arterial Spin Labelling (ASL), which is conceptually based on the flow of magnetically labelled blood. This has a subtle effect on the signal intensity of the tissue where the blood arrives. The main advantage of this technique is that it does not require any contrast agent injection (Petersen et al 2006). However, its sensitivity compared to contrast enhanced techniques is considerably lower. R352 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 3. An example of a prostate cancer patient. (a) T2w image, (b) ADC map and (c) Ktrans map of a prostate cancer patient (d) GTV areas by threshold combinations of the ADC and Ktrans maps. The overlap volume increases for increasing ADC thresholds and decreasing Ktrans thresholds. However, a complete overlap between thresholded ADC and thresholded Ktrans regions was not found for any of the threshold combinations (reproduced with permission from Groenendaal et al 2010b). Despite the improved contrast, accurate tumour definition is still difficult and generally tumour volume is largely overestimated due to tumour induced tissue alterations around the gross tumour volume (Daisne et al 2004). Diffusion tensor imaging has been proposed as a novel tool for improved distinction of the CTV (Price et al 2006). Poor tumour delineation is a major source of inaccuracies in radiotherapy treatment. To improve this, (semi)automatic segmentations based on multi-parameter quantitative MRI might be helpful. Dynamic enhanced MRI (DCE-MRI) and diffusion weighted MRI (DWI) are two widely used quantitative MRI methods (van der Heide et al 2012). DCE MRI provides information on micro-vascular properties like vessel permeability, blood flow, and extra-cellular space which are altered in tumour tissue due to presence of angiogenesis (Cao et al 2011). The application of pharmo-kinetic analysis on signal enhancement curves on a voxel basis, allows the generation of quantitative parameter maps e.g. so-called Ktrans maps are frequently used for GTV delineation in prostate cancer reflecting a mix of blood flow and vessel permeability (Groenendaal et al 2010b). The apparent diffusion coefficient (ADC) derived from DWI reflects the microscopic water mobility, which is related to the structural microenvironment (Padhani et al 2009). For automatic assignment of tumour voxels, a high specificity per voxel is needed. Different parameters generally do not indicate that the same voxels are tumours (Groenendaal et al 2010b). Therefore, probability mapping using combined parameter classifiers is applied, as is shown in prostate cancer (figure 3) (Groenendaal et al 2012). A drawback of multiparameter mapping is the time consuming imaging acquisition. Recently, Ma et al introduced MRI fingerprinting, which is a conceptually new, quantitative image acquisition and processing method (Ma et al 2013) which promises fast, repeated, quantitative MRI. Recently, the need for better lymph node imaging has been emphasized. As local tumour treatment improves, recurrences in lymph nodes become apparent (Nomden et al 2013). Conventionally lymph node imaging is based on T1 contrast. The identification of metastasized lymph nodes is a challenging task. Generally they are diagnosed based on size criteria, but both false positive and false negative lymph nodes are frequently found. In head and neck, DWI showed a high sensitivity and specificity for sub-centimetre positive lymph nodes to help in this distinction (Vandecaveye et al 2009). However, in the pelvic area, compared to conventional MRI, DWI did not add any additional diagnostic value (Klerkx et al 2012). Most promising results were achieved using ultra-small super-paramagnetic iron oxide (USPIO) R353 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 4. Example dedicated diffusion weighted T2-FFE scan with fat, blood and mus- cle suppression for MRI lymph node detection in the neck area (reproduced with permission from Philippens et al 2012). in breast and prostate cancer (Harisinghani et al 2006, Barentsz et al 2007). USPIO particles collect in negative lymph nodes, because they are incorporated by macrophages. Due to the iron loading, the MR signal of normal lymph nodes will disappear about 24 h after contrast administration, while a minimal MR signal change will occur in metastatic nodes due to much lower iron uptake. Despite the promising results and the need for accurate lymph node diagnosis, no approval for use of USPIO from the Food and Drug Agency has been released yet. Apart from the diagnosis of positive lymph nodes, elective radiotherapy of lymph nodes in high risk areas is common practice. CT is the conventional modality for the definition of these regions, but the smaller lymph nodes are not visible on CT. Therefore, anatomical boundaries are defined where most of the lymph nodes will be found. MRI might visualize lymph nodes with a higher sensitivity due to the improved contrast. To distinguish lymph nodes from the surrounding tissue suppression of fat, blood and muscle tissue is required. This is achieved by designing a pulse sequence with intrinsic diffusion weighting in a T2 weighted water only scan, as is used in neurography (Zhang et al 2008, Philippens et al 2012) (figure 4). Moreover, USPIO enhanced MRI has shown that a substantial number of positive lymph nodes in prostate cancer were not located in the routine surgical areas or in the axillary region defined by delineation guidelines (Heesakkers et al 2009, MacDonald et al 2010). The above mentioned MR imaging procedures can also be used for treatment response assessment. As an example, the response of chemoradiotherapy for rectal cancer must be quantified to decide in which patients surgery may be omitted (Solanki et al 2013). The difference in ADC seems to be a powerful tool for predicting pathologic complete response early in the treatment course (Lambrecht et al 2012, Bäuerle et al 2013, Intven et al 2013). Only FDG-PET seems insufficient for prediction response in clinical practice, e.g. in the treatment of patients with rectum cancer (Guillem et al 2013). Not all tumours show a response during treatment, which can lead to a decision to differentiate or change dose. In prostate cancer, changes in ADC are not observed during treatment (Foltz et al 2013). However, diffusion weighted imaging can be used to define the exact location of recurrences of prostate tumours (van Vulpen et al 2009), providing essential feedback on treatment choices. In prostate cancer a higher dose is required in areas with more aggressive tumour cells and with more tumour cells (van Vulpen et al 2009). R354 Topical Review Phys. Med. Biol. 59 (2014) R349 4. Treatment simulation The definition of irradiation fields requires a geometrically accurate dataset, acquired with the patient in a fixed radiotherapy position. Both conditions need attention since MRI is prone to geometry and intensity distortions (Moerland et al 1995) and current MR scanners with hollow couches and different types of RF coils attached to the patient’s body, may conflict with the radiotherapy position (Devic 2012). Instead of using MRI alone for radiotherapy planning, the use of registered MRI and CT datasets is a possible approach. The advantages of this approach is that CT provides geometric accuracy with a large field of view and delivery of tissue electron densities for dose calculation, while the MRI may zoom in on the tumour volume and provides detailed delineation and characterization information. Whatever approach is chosen, insight into the origin and impact of MR image distortions is needed before introducing MRI in radiotherapy treatment planning. MR images can be acquired with a variety of pulse sequences. The occurrence and severity of MR image distortions depends on the type of pulse sequence and on the object. Investigations on MR image distortions date back from the 80s when Lerski (1988) observed machine dependent geometric distortions up to 13 mm in a European multi-centre investigation. Geometric distortion in MR imaging predominantly arises from the inhomogeneity of the static magnetic field and the nonlinearity of the gradients. Bakker et al (1992) investigated system related imperfections by systematic variation of the strength, direction, and polarity of the read-out gradient in imaging experiments on a grid of cylindrical sample tubes. For the 1.5 T Philips Gyroscan system used in this study, static field related errors up to 7 mm and gradient related errors up to 4 mm were observed (midcoronal plane, FOV 400 mm, read out gradient between 0.5 and 3.0 mT m−1). It was also shown that in spin echo and gradient echo imaging, both gradient errors and static field inhomogeneity can lead to image distortions in the direction of the frequency encoding gradient, whereas in the phase encoding gradient image distortions are solely caused by gradient errors. System related distortions caused by imperfections in the static magnetic field and gradients can be readily corrected for and nowadays this is available on most modern MR scanners as a post-processing tool (Doran et al 2005). Gradient and static field distortions grow toward the periphery of the imaging field. Old MRI radiotherapy simulation systems, like the Panorama 0.23 T (Philips), have such a small field of view that peripheral distortions are uncontrolled (Mah et al 2002). In most clinical situations the tumour will be positioned in close proximity to the isocentrec and system related distortions will be minimised, in modern MRI systems, to the sub-millimetre range. B0 magnetic field errors mainly stem from imperfections of the MR scanner, which can be corrected as indicated above, but B0 magnetic field errors also originate from the patient. Since the human body susceptibility distribution is a major factor perturbing the magnetic field, those geometrical distortions become patient anatomy dependent. Due to the relatively large susceptibility difference between tissue and air, the image distortions are expected to be largest at tissue–air interfaces. Magnetic field distributions and image distortions for simple objects, such as cylinders and spheres, have been solved analytically (Chu et al 1990). For the magnetic field in and around the patient, numerical methods have to be applied. Bhagwandien et al (1994) developed a method to calculate the magnetic field distribution in and around a 3D object using a technique based on the finite difference method and applied it to the human body. Indeed, field perturbations were largest at the tissue–air interfaces, between −5–6 ppm outside the head and between −6 and 5 ppm inside the head near the sinuses. Resulting image distortions depend on the strength of the read out gradient, e.g. between −5 and 5 mm for a typical read out gradient strength (1.5 mT m−1 at 1.5 T). Those susceptibility related errors are inversely proportional to gradient strength, whereas gradient related errors turned out to be R355 Topical Review Phys. Med. Biol. 59 (2014) R349 independent of gradient strength. It is therefore recommended to apply the strongest available read-out gradients when geometric fidelity is given preference to signal-to-noise considerations, making 1.5 T systems easier to handle compared to 3.0 T systems. Undistorted images may be acquired with pulse sequences that only apply phase encoding of the MR signal using so-called single point imaging (SPI) (Gruwel et al 2007, Crijns et al 2012a). However, phase encoding is time consuming and usually not applied for clinical MR imaging. Compressed sensing can accelerate SPI and make the method suitable for QA purposes (Crijns et al 2012a). Another approach is to measure the magnetic field error and use it for correcting the MR image (Baldwin et al 2009, Crijns et al 2011a). For all normal imaging applications, susceptibility related errors can be minimised to sub-mm level (Stanescu et al 2012). There is an exception for special DWI sequences used for functional imaging (Embleton et al 2010). DWI is typically based on EPI sequences, which are highly sensitive for susceptibility errors due to the low pixel-bandwidth in the phase encode direction, with errors running up to the cm scale. Careful mapping of the magnetic field must be applied to correct these distortions. For the moment the University Medical Centre Utrecht has chosen to use CT as a geometry master for Radiotherapy Treatment Planning (RTP) and to register the high resolution and often zoomed MR images, used for delineation, with this CT. Scan protocols generally contain T2 weighted 2D multiple slice turbo spin echo (TSE) sequences and high resolution 3D steady state free precession (SSFP) sequences with relatively high bandwidth and sequences for functional imaging (DCE-MRI and DWI). Tumour delineation is saved on the high resolution SSFP image set, which is registered with the CT data used for setting up the irradiation beams. Image co-registration is possible in many ways and is becoming a separate profession (Devic 2012). It is essential that the delineation from the MRI is transferred from the MRI to the CT. Mis-registration may introduce a systemic error. To minimise the introduction of new errors it is essential that the structures and/or fiducial markers used in the position verification process are registered correctly. Focus on the registration of tumour contours may be considered to be an erroneous approach. Using only the MRI for delineation, without the CT information, may prevent this error. The fundamental problem of registering different images will only be solved if the fiducials used for position verification are clearly visible on the MRI (Kapanen et al 2012) or if direct MRI is available at the treatment itself. Those systems will be discussed in the chapter on MRI guidance for external beam radiotherapy. Like 4D CT, MRI can supply information on organ movements (McBain et al 2009, Chan et al 2008). Cine MRI can easily supply breathing related information at a sub-second scale without any radiation dose involved. These conventional techniques use binning techniques and thus provide 4D information by post-processing. Modern techniques try to acquire MRI data real time in 2D (Bauer et al 2013) and recently even in 3D (Kim et al 2013, Niebergall et al 2013) and thus provide the data needed for margin assessment (Paulson et al 2011, see example in figure 5) and treatment guidance (Stemkens et al 2013). A new development is the use of MRI-only for generating the Hounsfield data required for treatment planning. This area of generating synthetic CT data from MRI is stimulated by the introduction of integrated MRI/PET systems. Hounsfield data can be obtained via image segmentation from the MRI or via direct visualization of the bony structures using UTE sequences (Hsu et al 2013, Korhonen et al 2014), figure 6). 5. MRI guidance for brachytherapy The value of MRI guidance for brachytherapy has been proven for patients with cervix cancer (Jürgenliemk-Schulz et al 2009, Pötter et al 2011, Nomden et al 2013). Guidelines were R356 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 5. An example of a 2D FLASH cine MRI (3 Hz) to measure GTV displacement (red contours) and corresponding percent change in GTV area (b,d) during one resting (a,b) and one swallowing event (c,d) for a H/N patient with a supraglottic tumor (reproduced with permission from Paulson et al 2011). Figure 6. An example of a pseudo-CT image (b) generated from T1/T2* MR images by using a HU conversion technique with the original MR image (a) from which the pseudo-CT image was constructed. (c) shows the corresponding transverse standard CT slice (reproduced with permission from Korhonen et al 2014). developed for the imaging and delineation of cervix cancer (GTV, high risk CTV, intermediate risk CTV) and for dose prescription (Haie-Meder et al 2005). It was observed that standard tandem/ovoid and tandem/ring applicator dose distributions from the radiograph/CT era did not cover the target in many instances and special applicators were developed to increase target coverage and to increase local control of the tumour (Jürgenliemk-Schulz et al 2009). R357 Topical Review Phys. Med. Biol. 59 (2014) R349 At the University Medical Centre Utrecht delineation of tumour volumes and OAR’s as well as the reconstruction of applicators is performed on axial, coronal and sagittal T2 weighted images. The accuracy of applicator reconstruction is in the order of pixel size, usually 1–2 mm, for plastic and titanium applicators at 1.5 T (De Leeuw et al 2009, Haack et al 2009). Titanium applicators and needles may cause susceptibility and RF artefacts, especially in 3 T MR images (Kim et al 2011). At higher field strengths, a potential hazard for interventional applications is the heating of devices, due to resonating electromagnetic RF waves along the conducting structure (Yeung et al 2007, van den Bosch et al 2010a). Other applications of MRI guided brachytherapy under development are focal HDR brachytherapy for patients with localized prostate cancer or recurrent localized prostate cancer, where tumour localization is based on multi-parametric imaging using T2w, DCEMRI, DWI and biopsy findings (Groenendaal et al 2010a, Moman et al 2010). In current MRI guided prostate implantation procedures the patient is moved in and out of the MR scanner between needle insertion, imaging and irradiation due to restricted access to the MR scanner and lack of MRI compatible brachytherapy afterloaders (Susil et al 2004). Several groups are developing MR compatible robotic devices for prostate implant procedures inside a cylindrical bore MR scanner and to reduce prostate deformations, due to the intervention the needle is inserted by tapping (Lagerburg et al 2006, van den Bosch et al 2010b) or shooting (Muntener et al 2008). Prostate brachytherapy is developing towards single-fraction HDR monotherapy and if early data are confirmed with longer follow-up, it may become the treatment of choice for many men with localised prostate cancer (Morton and Hoskin 2013). To deliver single fraction HDR monotherapy in a safe manner, the use of an MRI compatible afterloader and the monitoring of the source position in relation to the target and organs at risk may be of great value. De Leeuw et al (2013) have shown that with special MR sequences and reconstruction algorithms HDR source position verification on MRI is feasible in real time. 6. MRI guidance for external beam radiotherapy The excellent soft-tissue contrast of MRI, combined with its real-time/cine capacities, while using harmless radiofrequency instead of ionizing radiation, theoretically allows direct target visualization for treatment guidance. It allows patient set-up based on the actual position, shape and motion characteristics, but also actual motion tracking during irradiation. Motion tracking can be used for real-time treatment guidance and adaptation, but also for recording anatomical changes for dose reconstruction and dose accumulation, thus providing unique positioning and dose certainty in the treatment process. To achieve this hybrid MRI, a radiotherapy technology is required, developed and under varying stages of construction. A first, moderate step, which does not require integration of the MRI and radiotherapy system, is presented by Karlsson et al (2009). They presented a next door MRI configuration where the patient is scanned prior to irradiation and then brought on the same table top and a dedicated trolley to the radiotherapy treatment room. No technical modifications are required to either system to facilitate the use of MRI for the determination of the actual anatomy, however, clearly no intra-fraction motion can be detected, and the patient transport introduces potential shifts in anatomy. The IMRIS system (Varian press release Oct 5 2010) offers a similar solution; it consists of a radiotherapy accelerator and an MRI that can be brought into the treatment room for scanning prior to treatment. This reduces the patient transport, but comes at the price of moving the MRI system on rails in and out of the room. A prototype system is currently under construction in Princess Margaret Hospital, Canada. R358 Topical Review Phys. Med. Biol. 59 (2014) R349 For an MRI during treatment itself, a more integrated solution is required. UMC Utrecht, the Netherlands, have together with Elekta AB, Stockholm, Sweden and Philips, Best, The Netherlands, pioneered such integration (Lagendijk et al 2002, Lagendijk et al 2008) with a 1.5 T MRI and a 6 MV accelerator. In the Cross Cancer Institute a prototype integrated 0.2 T MRI and a 6 MV radiotherapy accelerator has been developed and built (Fallone et al 2009). A commercial alternative is the combined 0.35 T MRI and 60Cobalt radiotherapy system being developed by Viewray, OH, U.S.A. 6.1. UMC Utrecht MRI accelerator The present prototype system comprises of a modified 1.5 T Achieva Philips MRI and an Elekta 6 MV accelerator in a ring in the mid-transversal plane around the MRI. The three main technical hurdles to allow both systems to operate unhampered are the magnetic interference, the radio-frequency interference and the beam transmission through the MRI. The active magnetic shielding of the MRI is modified to create a low field toroid in the transversal mid-plane to magnetically decouple the MRI and the accelerator (Overweg et al 2009), this way the accelerator still operates, although it is in the vicinity of the MRI and the MRI is not perturbed by the presence of ferrous accelerator components. The radio-frequency (RF) interference between the accelerator components and the MRI acquisition system cope because of the redesign of the Faraday cage. Conventionally the MRI is placed inside a Faraday cage to prevent interference with the outer world. For the hybrid MRI accelerator, the aluminium cryostat wall is part of the Faraday cage and therefore, the accelerator is positioned outside the cage. Another modification is for the beam transmission, to minimize beam absorption and heterogeneity a homogeneous, circumferential beam portal in the mid plane is made to allow beam passage (Overweg et al 2009). The proof of concept of the system for a static configuration was given in 2009 (Raaymakers et al 2009). Simultaneous irradiation and MRI was shown to be feasible. As designed, both systems operate independent of each other. Since then the system is being upgraded with a ring mounted accelerator which allows continuous rotation in either direction (figure 7). At the same time the system is equipped with a MLC. This technical prototype has been used to demonstrate MRI based gating and tracking on moving phantoms (Crijns et al 2012b). 1D MRI navigators where used to follow the moving phantom and with a latency of less than 200 ms the radiation could be gated or the beam could be moved along with the phantom. Additionally, the MRI could be used to reconstruct the dose on the moving phantom (Crijns et al 2012b), which is crucial for establishing precise dose response relationships. 6.2. Renaissance system of Viewray Viewray, OH, USA is a start-up company from the University of Florida and has developed and built a hybrid 0.35 T MRI and Cobalt-60 radiotherapy system, the Renaissance, see1 (figure 8). Three Cobalt-60 units equipped with MLC are positioned in a ring in the midtransversal plane of the double donut, so open, MRI system and can rotate 120° to allow radiation delivery from each gantry position. Obviously, the radio-active sources are not affected by the magnetic stray field and the open MRI design facilitates beam transmission, also RF interference is limited due to the use of radio-active sources. The potential impact of the ring mounted radiation units on the MRI performance is not reported on yet. The first non-clinical systems are installed and imaging and dosimetric studies are underway. 1 www.viewray.com R359 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 7. Photograph of the MRI linac experimental prototype system UMC Utrecht. Figure 8. Schematic drawing ViewRay renaissance system (courtesy ViewRay). 6.3. The Cross Cancer Institute system The system at the Cross Cancer Institute is a bi-planar, 0.2 T MRI system with a 27 cm gap integrated with a 6 MV accelerator (Fallone et al 2009). The accelerator is positioned laterally to the MRI, so the beam enters through the open side of the magnet, facilitating beam transmission. The magnetic interference in this system is solved by passively shielding the accelerator. This passive shielding on its turn perturbs the main magnetic field; therefore the main magnetic field is shimmed for the presence of the passive accelerator shielding. As a consequence, the geometry of accelerator and MRI must be fixed since shimming is done R360 Topical Review Phys. Med. Biol. 59 (2014) R349 Figure 9. Phase II linac-MR system (6 MV linac, 0.6 T MR system, and 60 cm bore) at the Cross Cancer Institute, University of Alberta, Edmonton2. The magnet is a high temperature superconductor. Currently building Phase III with 85 cm bore. Figure 10. Schematic drawing of the MRI linac design by Paul Keall for investigating the magnetic field orientation according to the beam (reproduced with permission from Constantin et al 2011). specifically for one position of the accelerator. To allow irradiation from multiple beam angles the accelerator has to rotate together with the MRI around the target in order to maintain the same geometrical relation between MRI and accelerator. Fallone et al demonstrated simultaneous MRI and irradiation using this system in 2008 (Fallone et al 2009). A human sized prototype is under construction comprising a 0.6 T MRI and a 6 MV accelerator. In addition, the orientation of the accelerator and the MRI can be changed in that system. The accelerator can be positioned either laterally to the MRI, so the beam enters through the gap, or on top of the MRI, where a dedicated hole in the MRI allows the beam to enter from the top (Keyvanloo et al 2012) (figure 9). The reason for doing so is that in this orientation the central radiation beam line is parallel with the magnetic field, reducing the impact of the magnetic field on the dose distribution, this will be discussed in more detail in section ‘Impact of the magnetic field on the dose distribution’. To investigate the orientation of the beam according to the magnetic field Keall and co-workers are developing a comparable system (Constantin et al 2011, Oborn et al 2012) (figure 10). 2 www.mp.med.ualberta.ca/linac-mr/photo_gallery.html R361 Topical Review Phys. Med. Biol. 59 (2014) R349 6.4. Consequences of magnetic field strengths The B0 magnetic field strength for the various designs ranges from 0.2 T–1.5 T. A higher field strength yields a higher signal to noise ratio (SNR) and in MRI SNR it can be traded off against temporal or spatial resolution and improve contrast. So higher field strengths yield more versatile MRI and with that improved image guidance scenarios. However, an increased B0 strength also yields increased susceptibility artefacts, which much be countered with increased gradient strengths. These artefacts need to be resolved before MRI can be used to guide radiation delivery as discussed above in section ‘MRI simulation’. So specifically for hybrid MRI radiotherapy systems dedicated MRI correction schemes are investigated to obtain geometrically correct MRI during treatment (Baldwin et al 2009, Crijns et al 2011b, 2012b). More related to the hybrid MRI radiotherapy systems, the main magnetic field strength is affecting the radiation dose distribution as well as radiation detectors. 6.5. Impact of the magnetic field on the dose distribution All systems treat with a photon beam, and a photon beam is unaffected by a magnetic field. However, secondary electrons are affected. The magnitude of this effect is determined by the magnetic field strength and the orientation of the incident beam relative to the magnetic field. For a transverse magnetic field relative to the beam a decreased built-up distance and a-symmetrical penumbra is seen, while the magnitude of this effect depends on the magnetic field strength (Raaymakers et al 2004, Raaijmakers et al 2008). Most striking is the impact at a tissue–air interface; without a magnetic field electrons would scatter away from such interface along with the incident radiation beam, with a magnetic field, these electrons will return, due to the Lorentz force, to the existing surface yielding a local dose increase (Raaijmakers et al 2005). This so called Electron Return Effect (ERE) manifests itself in a different way for different radiation field sizes, magnetic field strengths and surface orientations (Raaijmakers et al 2008). Opposing beams do, in the first order, cancel the ERE effect as shown by Raaijmakers et al (2005) and when using multi-beam (so approximately multiple opposing beams) IMRT the effect can be entirely compensated (Raaijmakers et al 2007). To do so, the magnetic field has to be accounted for in the dose calculations, which at this stage means a Monte Carlo approach is required. The impact of the magnetic field is also dependent on the orientation relative to the incident radiation beam. For a parallel configuration with the beam along the magnetic field lines, the impact for tissue–air interfaces is smaller (St Aubin et al 2010). However, in such a configuration, the contamination electrons from the radiation source and air column travelled, are captured in the photon beam by the parallel magnetic field and potentially increase the dose at the entrance side of the beam (Oborn et al 2012). For realistic MRI stray fields this effect may be limited (Keyvanloo et al 2012) but have to be investigated further. 6.6. Radiation dosimetry in magnetic fields Beside an altered patient dose distribution in the presence of a magnetic field, also radiation detectors can be affected. This is clear particularly for ionization chambers, which are basically an air cavity in a water-like environment and thus the response will be affected. Similar to the ERE discussed above, the response is likely to be dependent on the orientation of the chamber relative to the magnetic field. This was demonstrated experimentally and by R362 Topical Review Phys. Med. Biol. 59 (2014) R349 Monte Carlo simulations for the NE2571 Farmer-type chamber (Meijsing et al 2009). The response could vary up to 11% depending on the orientation for a 1.5 T magnetic field. 6.7. Impact of MRI radiofrequency coils In MRI the signal is typically picked up by a RF antenna positioned on the patient. The optimal position for this antenna is inevitably in the radiation field. Fortunately, the receiving antenna can be made to be thin enough to yield a negligible attenuation to the beam. This was demonstrated already for a hybrid 0.5 T MRI kV fluoroscopy system (Fahrig et al 2001), where the MRI coil was optimised for beam transmission and made transparent for kV beams. For MV radiation therapy beams, even non-optimised RF coils can be suitable as shown by Hoogcarspel et al (2013). Another impact of the RF coil is the potential image degradation due to the irradiation of the antenna loop. Because the copper loop has a different density to the surrounding tissue, an electron dis-equilibrium can occur in the RF antenna, with a Radiation Induced Current as a consequence (Burke et al 2012). This effect has been demonstrated experimentally for low magnetic field strength and thus a relatively low RF frequency of 9 MHz (Burke et al 2012). At 1.5 T (64 MHz), the impact of irradiating the RF coil did not result in the degradation of SNR (Hoogcarspel et al 2013). 6.8. MRI guided proton therapy The promise of real-time anatomical feedback is appealing for photon radiotherapy, but even more so for proton therapy. There, the strong dose gradient from the Bragg peak demands high precision image guidance to fully exploit the proton beam advantages. At present the range uncertainty is countered by additional margins and limited IMRT modulation (McGowan et al 2013). So far, investigations into such hybrid system are limited to the impact on dosimetry. As the proton beam itself consists of charged particles, the beam trajectory will be affected by the magnetic field. This deflection can be analytically calculated (Wolf et al 2012). The impact of the magnetic field on the secondary electrons is negligible (Raaymakers et al 2008). This is due to the low energy of the secondary electrons in proton therapy relative to those with photon therapy. 7. Conclusion It may be clear from this review that the impact of modern MRI on the radiotherapy process is growing fast. MRI based treatment simulation combined with tumour characterization is becoming part of the daily routine in clinics. The impact of MRI on brachytherapy cannot be underestimated; MRI is making brachytherapy a quantitative therapy and reduces the operator dependency. Seeing what you treat, bringing certainty and quantification in the treatment process, is essential for brachytherapy, but will also have a huge impact on external beam radiotherapy, making radiotherapy more of an interventional radiology process. References Bakker C J, Moerland M A, Bhagwandien R and Beersma R 1992 Analysis of machine-dependent and object-induced geometric distortion in 2DFT MR imaging Magn. Reson. Imag. 10 597–608 Baldwin L N, Wachowicz K and Fallone B G 2009 A two-step scheme for distortion rectification of magnetic resonance images Med. Phys. 36 3917–26 R363 Topical Review Phys. Med. Biol. 59 (2014) R349 Bammer R 2003 Basic principles of diffusion-weighted imaging Eur. J. Radiol. 45 169–84 Barentsz J O, Fütterer J J and Takahashi S 2007 Use of ultrasmall superparamagnetic iron oxide in lymph node MR imaging in prostate cancer patients Eur. J. Radiol. 63 369–72 Bauer R W, Radtke I, Block K T, Larson M C, Kerl J M, Hammerstingl R, Graf T G, Vogl T J and Zhang S 2013 True real-time cardiac MRI in free breathing without ECG synchronization using a novel sequence with radial k-space sampling and balanced SSFP contrast mode Int. J. Cardiovasc. Imag. 29 1059–67 Bäuerle T et al 2013 Diffusion-weighted imaging in rectal carcinoma patients without and after chemoradiotherapy: a comparative study with histology Eur. J. Radiol. 82 444–52 Becker M, Burkhardt K, Dulguerov P and Allal A 2008a Imaging of the larynx and hypopharynx Eur. J. Radiol. 66 460–79 Becker M, Zbären P, Casselman J W, Kohler R, Dulguerov P and Becker C D 2008b Neoplastic invasion of laryngeal cartilage: reassessment of criteria for diagnosis at MR imaging Radiology 249 551–9 Beets-Tan R G and Beets G L 2011 Local staging of rectal cancer: a review of imaging J. Magn. Reson. Imag. 33 1012–9 Bhagwandien R, Moerland M A, Bakker C J G, Beersma R and Lagendijk J J W 1994 Numerical analysis of the magnetic field for arbitrary magnetic susceptibility distributions in 3D Magn. Reson. Imag. 12 101–7 Bottomley P A, Hardy C J, Argersinger R E and Allen-Moore G 1987 A review of 1H nuclear magnetic resonance relaxation in pathology: are T1 and T2 diagnostic? Med. Phys. 14 1–37 Breuer F A, Blaimer M, Heidemann R M, Mueller M F, Griswold M A and Jakob P M 2005 Controlled aliasing in parallel imaging results in higher acceleration (CAIPIRINHA) for multi-slice imaging Magn. Reson. Med. 53 684–91 Burke B, Wachowicz K, Fallone B G and Rathee S 2012 Effect of radiation induced current on the quality of MR images in an integrated linac-MR system Med. Phys. 39 6139–47 Caldas-Magalhaes J, Kasperts N, Kooij N, van den Berg C A, Terhaard C H, Raaijmakers C P and Philippens M E 2012 Validation of imaging with pathology in laryngeal cancer: accuracy of the registration methodology Int. J. Radiat. Oncol. Biol. Phys. 82 e289–98 Cao Y 2011 The promise of dynamic contrast-enhanced imaging in radiation therapy Semin. Radiat. Oncol. 21 147–56 Chan P, Dinniwell R, Haider M A, Cho Y B, Jaffray D, Lockwood G, Levin W, Manchul L, Fyles A and Milosevic M 2008 Inter—and intrafractional tumor and organ movement in patients with cervical cancer undergoing radiotherapy: a cinematic-MRI point-of-interest study Int. J. Radiat. Oncol. Biol. Phys. 70 1507–15 Chu S C, Xu Y, Balschi J A and Springer C S Jr 1990 Bulk magnetic susceptibility shifts in NMR studies of compartmentalized samples: use of paramagnetic reagents Magn. Reson. Med. 13 239–62 Constantin D E, Fahrig R and Keall P J 2011 A study of the effect of in-line and perpendicular magnetic fields on beam characteristics of electron guns in medical linear accelerators Med. Phys. 38 4174–85 Crijns S P M, Kok J G, Lagendijk J J W and Raaymakers B W 2011a Towards MRI-guided linear accelerator control: gating on an MRI accelerator Phys. Med. Biol. 56 4815–25 Crijns S P, Raaymakers B W and Lagendijk J J 2011b Real-time correction of magnetic field inhomogeneity-induced image distortions for MRI-guided conventional and proton radiotherapy Phys. Med. Biol. 56 289–97 Crijns S P M, Bakker C J G, Seevinck P R, de Leeuw H, Lagendijk J J W and Raaymakers B W 2012a Towards inherently distortion-free MR images for image-guided radiotherapy on an MRI accelerator Phys. Med. Biol. 57 1349–58 Crijns S P M, Raaymakers B W and Lagendijk J J W 2012b Proof of concept of MRI-guided tracked radiation delivery: tracking 1D motion Phys. Med. Biol. 57 7863–72 Daisne J F, Duprez T, Weynand B, Lonneux M, Hamoir M, Reychler H and Grégoire V 2004 Tumor volume in pharyngolaryngeal squamous cell carcinoma: comparison at CT, MR imaging, and FDG PET and validation with surgical specimen Radiology 233 93–100 De Leeuw A A, Moerland M A, Nomden C, Tersteeg R H, Roesink J M and Jürgenliemk-Schulz I M 2009 Applicator reconstruction and applicator shifts in 3D MR-based PDR brachytherapy of cervical cancer Radiother. Oncol. 93 341–6 de Leeuw H, Moerland M A, van Vulpen M, Seevinck P R and Bakker C J 2013 A dual-plane co-RASOR technique for accurate and rapid tracking and position verification of an Ir-192 source for single fraction HDR brachytherapy Phys. Med. Biol. 58 7829–39 R364 Topical Review Phys. Med. Biol. 59 (2014) R349 Devic S 2012 MRI simulation for radiotherapy treatment planning Med. Phys. 39 6701–11 Donahue M J, Hoogduin H, van Zijl P C, Jezzard P, Luijten P R and Hendrikse J 2011 Blood oxygenation level-dependent (BOLD) total and extravascular signal changes and ΔR2* in human visual cortex at 1.5, 3.0 and 7.0 T NMR Biomed. 24 25–34 Doran S J, Charles-Edwards L, Reinsberg S A and Leach M O 2005 A complete distortion correction for MR images: I. Gradient warp correction Phys. Med. Biol. 50 1343–61 Ehman R L and Felmlee J P 1989 Adaptive technique for high definition MR imaging of moving structures Radiology 173 255–63 Ehman R L, McNamara M T, Pallack M, Hricak H and Higgins C B 1984 Magnetic resonance imaging with respiratory gating—techniques and advantages Am. J. Radiol. 143 1175–82 Embleton K V, Haroon H A, Morris D M, Ralph M A and Parker G J 2010 Distortion correction for diffusion-weighted MRI tractography and fMRI in the temporal lobes Hum. Brain Mapp. 31 1570–87 Fahrig R, Butts K, Rowlands J A, Saunders R, Stanton J, Stevens G M, Daniel B L, Wen Z, Ergun D L and Pelc N J 2001 A truly hybrid interventional MR/x-ray system: feasibility demonstration J. Magn. Reson. Imag. 13 294–300 Fallone B G, Murray B, Rathee S, Stanescu T, Steciw S, Vidakovic S, Blosser E and Tymofichuk D 2009 First MR images obtained during megavoltage photon irradiation from a prototype integrated linac-MR system Med. Phys. 36 2084–8 Foltz W D et al 2013 Changes in apparent diffusion coefficient and T2 relaxation during radiotherapy for prostate cancer J. Magn. Reson. Imag. 37 909–16 Groenendaal G, Borren A, Moman M R, Monninkhof E, van Diest P J, Philippens M E, van Vulpen M and van der Heide U A 2012 Pathologic validation of a model based on diffusion-weighted imaging and dynamic contrast-enhanced magnetic resonance imaging for tumor delineation in the prostate peripheral zone Int. J. Radiat. Oncol. Biol. Phys. 82 e537–44 Groenendaal G, Moman M R, Korporaal J G, van Diest P J, van Vulpen M, Philippens M E P and van der Heide U A 2010a Validation of functional imaging with pathology for tumor delineation in the prostate Radiother. Oncol. 94 145–50 Groenendaal G, van den Berg C A, Korporaal J G, Philippens M E, Luijten P R, van Vulpen M and van der Heide U A 2010b Simultaneous MRI diffusion and perfusion imaging for tumor delineation in prostate cancer patients Radiother. Oncol. 95 185–90 Gruwel M L H, Latta P, Tanasiewicz M, Volotovskyy V, Sramek M and Tomanek B 2007 MR imaging of teeth using a silent single point imaging technique Appl. Phys. A 88 763–7 Guillem J G et al 2013 Neither FDG-PET nor CT can distinguish between a pathological complete response and an incomplete response after neoadjuvant chemoradiation in locally advanced rectal cancer: a prospective study Ann. Surg. 258 289–95 763–7 Haack S, Nielsen S K, Lindegaard J C, Gelineck J and Tanderup K 2009 Applicator reconstruction in MRI 3D image-based dose planning of brachytherapy for cervical cancer Radiother. Oncol. 91 187–93 Haacke E M, Brown R W, Thompson M R and Venkatesan R 1999 Magnetic Resonance Imaging: Physical Principles and Sequence Design (New York: Wiley-Liss) Haie-Meder C et al 2005 Recommendations from Gynaecological (GYN) GEC ESTRO Working Group (I): concepts and terms in 3D image-based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV Radiother. Oncol. 74 235–45 Hargreaves B A 2012 Rapid gradient-echo imaging J. Magn. Reson. Imag. 36 1300–13 Harisinghani M G, Saksena M A, Hahn P F, King B, Kim J, Torabi M T and Weissleder R 2006 Ferumoxtran-10-enhanced MR lymphangiography: does contrast-enhanced imaging alone suffice for accurate lymph node characterization? AJR Am. J. Roentgenol. 186 144–8 Heesakkers R A, Jager G J, Hövels A M, de Hoop B, van den Bosch H C, Raat F, Witjes J A, Mulders P F, van der Kaa C H and Barentsz J O 2009 Prostate cancer: detection of lymph node metastases outside the routine surgical area with ferumoxtran-10-enhanced MR imaging Radiology 251 408–14 Hoogcarspel S J, Crijns S P, Lagendijk J J, van Vulpen M and Raaymakers B W 2013 The feasibility of using a conventional flexible RF coil for an online MR-guided radiotherapy treatment Phys. Med. Biol. 58 1925–32 Hoskin P J et al 2007 Hypoxia in prostate cancer: correlation of BOLD-MRI with pimonidazole immunohistochemistry—initial observations Int. J. Radiat. Oncol. Biol. Phys. 68 1065–71 R365 Topical Review Phys. Med. Biol. 59 (2014) R349 Hsu S H Cao Y, Huang K, Feng M and Balter J M 2013 Investigation of a method for generating synthetic CT models from MRI scans of the head and neck for radiation therapy Phys. Med. Biol. 58 8419–35 Intven M, Reerink O and Philippens M E 2013 Diffusion-weighted MRI in locally advanced rectal cancer: pathological response prediction after neo-adjuvant radiochemotherapy Strahlenther. Onkol. 189 117–22 Jürgenliemk-Schulz I M, Tersteeg R J, Roesink J M, Bijmolt S, Nomden C N, Moerland M A and de Leeuw A A 2009 MRI-guided treatment-planning optimisation in intracavitary or combined intracavitary/interstitial PDR brachytherapy using tandem ovoid applicators in locally advanced cervical cancer Radiother. Oncol. 93 322–30 Kapanen M, Collan J, Beule A, Seppälä T, Saarilahti K and Tenhunen M 2012 Commissioning of MRIonly based treatment planning procedure for external beam radiotherapy of prostate Magn. Reson. Med. Ahead of print Karlsson M, Karlsson M G, Nyholm T, Amies C and Zackrisson B 2009 Dedicated magnetic resonance imaging in the radiotherapy clinic Int. J. Radiat. Oncol. Biol. Phys. 74 644–51 Keyvanloo A, Burke B, Warkentin B, Tadic T, Rathee S, Kirkby C, Santos D M and Fallone B G 2012 Skin dose in longitudinal and transverse linac-MRIs using Monte Carlo and realistic 3D MRI field models Med. Phys. 39 6509–21 Kim Y C, Lebel R M, Wu Z, Ward S L, Khoo M C and Nayak K S 2013 Real-time 3D magnetic resonance imaging of the pharyngeal airway in sleep apnea Magn. Reson. Med. 71 1501–10 Kim Y C, Muruganandham M, Modrick J M and Bayouth J E 2011 Evaluation of artefacts and distortions of titanium applicators on 3.0 T MRI: feasibility of titanium applicators in MRI-guided brachytherapy for gynecological cancer Int. J. Radiat. Oncol. Biol. Phys. 80 947–55 Klerkx W M et al 2012 The value of 3.0 T diffusion-weighted MRI for pelvic nodal staging in patients with early stage cervical cancer Eur. J. Cancer 48 3414–21 Korhonen J, Kapanen M, Keyrilainen J, Seppala T and Tenhunen M 2014 A dual model HU conversion from MRI intensity values within and outside of bone segment for MRI-based radiotherapy treatment planning of prostate cancer Med. Phys. 41 011704 Lagendijk J J W, Raaymakers B W, Raaijmakers A J E, Overweg J, Brown K J, Kerkhof E M, van der Put R W, Hårdemark B, van Vulpen M and van der Heide U A 2008 MRI/linac integration Radiother. Oncol. 86 25–9 Lagendijk J J W, Raaymakers B W, Van Der Heide U A, Topolnjak R, Dehnad H, Hofman P, Nederveen A J, Schulz I M, Welleweerd J and Bakker C J G 2002 MRI guided radiotherapy: MRI as position verification system for IMRT Radiother. Oncol. 64 224 (suppl 1) (Czech Republic European Society for Therapeutic Radiation Oncology) Lagerburg V, Moerland M A, van Vulpen M and Lagendijk J J W 2006 A new robotic needle insertion method to minimise attendant prostate motion Radiother. Oncol. 80 73–7 Lambrecht M, Vandecaveye V, De Keyzer F, Roels S, Penninckx F, Van Cutsem E, Filip C and Haustermans K 2012 Value of diffusion-weighted magnetic resonance imaging for prediction and early assessment of response to neoadjuvant radiochemotherapy in rectal cancer: preliminary results Int. J. Radiat. Oncol. Biol. Phys. 82 863–70 Lanzer P et al 1984 Cardiac imaging using gated magnetic resonance Radiology 150 121–7 Larkman D J, Hajnal J V, Herlihy A H, Coutts G A, Young I R and Ehnholm G 2001 Use of multicoil arrays for separation of signal from multiple slices simultaneously excited J. Magn. Reson. Imag. 13 313–7 Le Bihan D, Poupon C, Amadon A and Lethimonnier F 2006 Artifacts and pitfalls in diffusion MRI J. Magn. Reson. Imag. 24 478–88 Lerski R A, McRobbie D W, Straughan K, Walker P M, de Certaines J D and Bernard A M 1988 Multicenter trial with protocols and prototype test objects for the assessment of MRI equipment. EEC concerted research project Magn. Reson. Imag. 6 201–14 Lewis C E, Prato F S, Drost D J and Nicholson R L 1986 Comparison of respiratory triggering and gating techniques for removal of respiratory artifacts in MR imaging Radiology 160 803–10 Low R N 2007 Abdominal MRI advances in the detection of liver tumours and characterisation Lancet Oncol. 8 525–35 Lustig M, Donoho D and Pauly J M 2007 Sparse MRI: the application of compressed sensing for rapid MR imaging Magn. Reson. Med. 58 1182–95 Ma D J, Gulani V, Seiberlich N, Liu K, Sunshine J L, Duerk J L and Griswold M A 2013 Magnetic resonance fingerprinting Nature 495 187–92 R366 Topical Review Phys. Med. Biol. 59 (2014) R349 MacDonald S M, Harisinghani M G, Katkar A, Napolitano B, Wolfgang J and Taghian A G 2010 Nanoparticle-enhanced MRI to evaluate radiation delivery to the regional lymphatics for patients with breast cancer Int. J. Radiat. Oncol. Biol. Phys. 77 1098–104 Mah D, Steckner M, Palacio E, Mitra R, Richardson T and Hanks G E 2002 Characteristics and quality assurance of a dedicated open 0.23 T MRI for radiation therapy simulation Med Phys. 29 2541–7 Marin D, Husarik D B, Boll D T and Merkle E M 2010 Abdominal magnetic resonance imaging at 3 T: oncological applications Top. Magn. Reson. Imag. 21 149–56 Markl M and Leupold J 2012 Gradient echo imaging J. Magn. Reson. Imag. 35 1274–89 McBain C A, Khoo V S, Buckley D L, Sykes J S, Green M M, Cowan R A, Hutchinson C E, Moore C J and Price P M 2009 Assessment of bladder motion for clinical radiotherapy practice using cinemagnetic resonance imaging Int. J. Radiat. Oncol. Biol. Phys. 75 664–71 McGowan S E, Burnet N G and Lomax A J 2013 Treatment planning optimisation in proton therapy Br. J. Radiol. 86 20120288 Meijsing I, Raaymakers B W, Raaijmakers A J E, Kok J G, Hogeweg L, Liu B and Lagendijk J J W 2009 Dosimetry for the MRI accelerator: the impact of a magnetic field on the response of a Farmer NE2571 ionization chamber Phys. Med. Biol. 54 2993–3002 Moerland M A, Beersma R, Bhagwandien R, Wijrdeman H K and Bakker C J G 1995 Analysis and correction of geometric distortions in 1.5 T magnetic resonance images for use in radiotherapy treatment planning Phys. Med. Biol. 40 1651–4 Moman M R, van den Berg C A, Boeken Kruger A E, Battermann J J, Moerland M A, van der Heide U A and van Vulpen M 2010 Focal salvage guided by T2-weighted and dynamic contrast-enhanced magnetic resonance imaging for prostate cancer recurrences Int. J. Radiat. Oncol. Biol. Phys. 76 741–6 Morton G C and Hoskin P J 2013 Brachytherapy: current status and future strategies—can high dose rate replace low dose rate and external beam radiotherapy? Clin. Oncol. (R. Coll. Radiol.) 25 474–82 Muntener M, Patriciu A, Petrisor D, Schär M, Ursu D, Song D Y and Stoianovici D 2008 Transperineal prostate intervention: robot for fully automated MR imaging—system description and proof of principle in a canine model. Radiology 247 543–9 Niebergall A, Zhang S, Kunay E, Keydana G, Job M, Uecker M and Frahm J 2013 Real-time MRI of speaking at a resolution of 33 ms: undersampled radial FLASH with nonlinear inverse reconstruction Magn. Reson. Med.69 477–85 Nomden C N, de Leeuw A A, Roesink J M, Tersteeg R J, Moerland M A, Witteveen P O, Schreuder H W, van Dorst E B and Jürgenliemk-Schulz I M 2013 Clinical outcome and dosimetric parameters of chemo-radiation including MRI guided adaptive brachytherapy with tandem-ovoid applicators for cervical cancer patients: a single institution experience Radiother. Oncol. 107 69–74 Oborn B M, Metcalfe P E, Butson M J, Rosenfeld A B and Keall P J 2012 Electron contamination modeling and skin dose in 6 MV longitudinal field MRIgRT: impact of the MRI and MRI fringe field Med. Phys. 39 874–90 Oechsner M, Pracht E D, Staeb D, Arnold J F, Köstler H, Hahn D, Beer M and Jakob P M 2009 Lung imaging under free-breathing conditions Magn. Reson. Med. 61 723–7 Ogawa S, Menon R S, Tank D W, Kim S G, Merkle H, Ellermann J M and Ugurbil K 1993 Functional brain mapping by blood oxygenation level-dependent contrast magnetic resonance imaging. A comparison of signal characteristics with a biophysical model Biophys. J. 64 803–12 Overweg J, Raaymakers B W, Lagendijk J J W and Brown K 2009 System for MRI guided radiotherapy Proc. Int. Soc. Mag. Reson. Med. 17 594 Padhani A R and Dzik-Jurasz A 2004 Perfusion MR imaging of extracranial tumor angiogenesis Top. Magn. Reson. Imag. 15 41–57 Padhani A R et al 2009 Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations Neoplasia 11 102–25 Patz S and Hawkes R C 1986 The application of steady-state free precession to the study of very slow fluid flow Magn. Reson. Med. 3 140–5 Paulson E S, Bradley J A, Wang D, Ahunbay E E, Schultz C and Li X A 2011 Internal margin assessment using cine MRI analysis of deglutition in head and neck cancer radiotherapy Med. Phys. 38 1740–7 Petersen E T, Zimine I, Ho Y C and Golay X 2006 Non-invasive measurement of perfusion: a critical review of arterial spin labelling techniques Br. J. Radiol. 79 688–701 Philippens M, Bongard H, Asselen B, van Ulpen M and Lagendijk J 2012 New high resolution T2-FFE MR imaging of axillary lymph nodes for real time radiation treatment guidance Med. Phys. 39 3889 Plewes D B and Kucharczyk W 2012 Physics of MRI: a primer J. Magn. Reson. Imag. 35 1038–54 R367 Topical Review Phys. Med. Biol. 59 (2014) R349 Pötter R et al 2011 Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer Radiother. Oncol. 100 116–23 Possanzini C, Van Liere P, Roeven H, Den Boef J, Saylor C, Van Eggermond J, Harvey P and Moore E 2011 Scalability and channel independency of the digital broadband dStream architecture Proc. of Annual meeting of the International Society on Magnetic Resonance in Medicine. abstract 5103 (Montreal, Canada) Price S J, Jena R, Burnet N G, Hutchinson P J, Dean A F, Peña A, Pickard J D, Carpenter T A and Gillard J H 2006 Improved delineation of glioma margins and regions of infiltration with the use of diffusion tensor imaging: an image-guided biopsy study AJNR Am. J. Neuroradiol. 27 1969–74 Pruessmann K P 2006 Encoding and reconstruction in parallel MRI NMR Biomed. 19 288–99 Raaijmakers A J, Hårdemark B, Raaymakers B W, Raaijmakers C P and Lagendijk J J 2007 Dose optimization for the MRI-accelerator: IMRT in the presence of a magnetic field Phys. Med. Biol. 52 7045–54 Raaijmakers A J E, Raaymakers B W and Lagendijk J J W 2005 Integrating a MRI scanner with a 6 MV radiotherapy accelerator: dose increase at tissue-air interfaces in a lateral magnetic field due to returning electrons Phys. Med. Biol. 50 1363–76 Raaijmakers A J E, Raaymakers B W and Lagendijk J J W 2008 Magnetic-field-induced dose effects in MR-guided radiotherapy systems: dependence on the magnetic field strength Phys. Med. Biol. 53 909–23 Raaymakers B W et al 2009 Integrating a 1.5 T MRI scanner with a 6 MV accelerator: proof of concept Phys. Med. Biol. 54 N229–37 Raaymakers B W, Raaijmakers A J E, Kotte A N T J, Jette D and Lagendijk J J W 2004 Integrating a MRI scanner with a 6 MV radiotherapy accelerator: dose deposition in a transverse magnetic field Phys. Med. Biol. 49 4109–18 Raaymakers B W, Raaijmakers A J E and Lagendijk J J W 2008 Feasibility of MRI guided proton therapy: magnetic field dose effects Phys. Med. Biol. 53 5615–22 Reichenbach J R, Venkatesan R, Yablonskiy D A, Thompson M R, Lai S and Haacke E M 1997 Theory and application of static field inhomogeneity effects in gradient-echo imaging J. Magn. Reson. Imag. 7 266–79 Riddell A M, Davies D C, Allum W H, Wotherspoon A C, Richardson C and Brown G 2007 Highresolution MRI in evaluation of the surgical anatomy of the esophagus and posterior mediastinum AJR Am. J. Roentgenol. 188 W37–43 Rijpkema M, Kaanders J H, Joosten F B, van der Kogel A J and Heerschap A 2002 Effects of breathing a hyperoxic hypercapnic gas mixture on blood oxygenation and vascularity of headand-neck tumors as measured by magnetic resonance imaging Int. J. Radiat. Oncol. Biol. Phys. 53 1185–91 Roemer P B, Edelstein W A, Hayes C E, Souza S P and Mueller O M 1990 The NMR phased array Magn. Reson. Med. 16 192–225 Runge V M, Clanton J A, Partain C L and James A E Jr 1984 Respiratory gating in magnetic resonance imaging at 0.5 T Radiology 151 521–3 Schakel T, Hoogduin J M, Terhaard C H, Philippens M E 2013 Diffusion weighted MRI in head-andneck cancer: geometrical accuracy Radiother. Oncol. 109 394–7 Sodickson D K et al 2005 Rapid volumetric MRI using parallel imaging with order-of-magnitude accelerations and a 32-element RF coil array: feasibility and implications Acad. Radiol. 12 626–35 Solanki A A, Chang D T and Liauw S L 2013 Future directions in combined modality therapy for rectal cancer: reevaluating the role of total mesorectal excision after chemoradiotherapy Onco Targets Ther. 6 1097–110 St Aubin J, Santos D M, Steciw S and Fallone B G 2010 Effect of longitudinal magnetic fields on a simulated in-line 6 MV linac Med. Phys. 37 4916–23 Stam M K, Crijns S P M, Zonnenberg B A, Barendrecht M M, van Vulpen M, Lagendijk J J W and Raaymakers B W 2012 Navigators for motion detection during real-time MRI-guided radiotherapy Phys. Med. Biol. 57 6797–805 Stanescu T, Wachowicz K and Jaffray D A 2012 Characterization of tissue magnetic susceptibilityinduced distortions for MRIgRT Med. Phys. 39 7185–93 Stemkens B, Tijssen R H, Van den Berg C A T, Lagendijk J J W, Moonen C T W, Ries M and Denis de Senneville B 2013 Optical flow analysis on undersampled radial acquisitions for real-time tracking of the pancreas in MR guided radiotherapy Proc. ISMRM (Salt lake City) R368 Topical Review Phys. Med. Biol. 59 (2014) R349 Susil R C, Camphausen K, Choyke P, McVeigh E R, Gustafson G S, Ning H, Miller R W, Atalar E, Coleman C N and Ménard C 2004 System for prostate brachytherapy and biopsy in a standard 1.5 T MRI scanner Magn. Reson. Med. 52 683–7 Vandecaveye V, De Keyzer F, Vander Poorten V, Dirix P, Verbeken E, Nuyts S and Hermans R 2009 Head and neck squamous cell carcinoma: value of diffusion-weighted MR imaging for nodal staging Radiology 251 134–46 van den Bosch M R, Moerland M A, Lagendijk J J W, Bartels L W and van den Berg C A T 2010a New method to monitor RF safety in MRI-guided interventions based on RF induced image artefacts Med. Phys. 37 814–21 van den Bosch M R, Moman M R, van Vulpen M, Battermann J J, Duiveman E, van Schelven L J, de Leeuw H, Lagendijk J J W and Moerland M A 2010b MRI-guided robotic system for transperineal prostate interventions: proof of principle Phys. Med. Biol. 55 N133–40 van der Heide U A, Houweling A C, Groenendaal G, Beets-Tan R G and Lambin P 2012 Functional MRI for radiotherapy dose painting Magn. Reson. Imag. 30 1216–23 van Rossum P S, van Hillegersberg R, Lever F M, Lips I M, van Lier A L, Meijer G J, van Leeuwen M S, van Vulpen M and Ruurda J P 2013 Imaging strategies in the management of oesophageal cancer: what’s the role of MRI? Eur. Radiol. 23 1753–65 van Veluw S J, Zwanenburg J J, Engelen-Lee J, Spliet W G, Hendrikse J, Luijten P R and Biessels G J 2013 In vivo detection of cerebral cortical microinfarcts with high-resolution 7 T MRI J. Cereb. Blood Flow Metab. 33 322–9 van Vulpen M, van den Berg C A, Moman M R and van der Heide U A 2009 Difficulties and potential of correlating local recurrences in prostate cancer with the delivered local dose Radiother. Oncol. 93 180–4 Verduijn G M, Bartels L W, Raaijmakers C P, Terhaard C H, Pameijer F A and van den Berg C A 2009 Magnetic resonance imaging protocol optimization for delineation of gross tumor volume in hypopharyngeal and laryngeal tumors Int. J. Radiat. Oncol. Biol. Phys. 74 630–6 Wielpütz M and Kauczor H U 2012 MRI of the lung: state of the art Diagn. Interv. Radiol. 18 344–53 Wolf R and Bortfeld T 2012 An analytical solution to proton Bragg peak deflection in a magnetic field Phys. Med. Biol. 57 N329–37 Yeung C J, Karmarkar P and McVeigh E R 2007 Minimizing RF heating of conducting wires in MRI Magn. Reson. Med. 58 1028–34 Zhang Z, Meng Q, Chen Y, Li Z, Luo B, Yang Z, Mao L and Lin E 2008 3 T imaging of the cranial nerves using 3D reversed FISP with diffusion-weighted MR sequence J. Magn. Reson. Imag. 27 454–8 R369