* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Approach to Arrhythmias
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
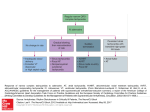
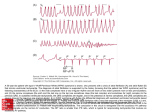
Approach to Arrhythmias Armed Forces Academy of Medical Sciences When to Suspect an Arrhythmia Symptoms variable and depend on rate of ventricular response, overall condition of patient, presence of structural heart disease Palpitations (regular vs. irregular, onset/offset) Chest pressure Dyspnea Lightheadedness, presyncope, syncope Triggers Termination maneuvers: especially vagal First Question Stable vs. Unstable Unstable: hypotensive, syncope, imminent death Unstable: revert to ACLS algorithm DC Cardioversion Most likely ventricular arrhythmia Stable Symptoms but not life threatening Differentiate wide complex from narrow complex Initial Evaluation of Stable Arrhythmias History Physical exam EKG (sinus rhythm, tachycardia) Twelve lead ECG with and without symptoms Narrow complex: likely a superventricular tachycardia (SVT) Wide complex Ventricular arrhythmia SVT with aberrant conduction Echo if structural heart disease suspected SVTs Any tachycardia requiring the atrium or the AVN for its perpetuation Common arrhythmia with an incidence of 2.5/1000 Twice as common in women Three primary etiologies AVNRT (most common) AVRT Atrial tachycardia (least common in absence of structural heart disease) Rare: IST, SNRT, junctional tachycardia SVTs Continued Can present at any age, first symptoms occur from 12 to 30 years AVNRT: middle to older age AVRT: adolescence Usually occurs in absence of structural heart disease Exceptions: Ebstein’s anomaly, familial preexcitation with hypertrophy, atrial tachycardia Classification of SVTs AV node dependent vs. independent AT: independent AVNRT, AVRT: dependent Short RP vs. Long RP Short RP (RP<PR): typical AVNRT, AVRT Long RP (PR<RP): AT, atypical AVNRT, rare forms of AVRT Regular vs. irregular Regular: AVNRT, AVRT, AT, AFL Irregular: AF, AT, AFL Paroxysmal Supraventricular Tachycardias: Short RP vs. Long RP no p-wave - AV node reentry AVNRT AT RP < PR - AV node reentry - AV reentry using an accessory pathway AVRT RP > PR - Atrial tachycardia - AV reentry using a decremental AP ex. PJRT - AV node reentry atypical/uncommon form Differential Diagnosis of NCT AVNRT Most common form of Paroxysmal SVT 50-60% of regular, narrow complex tachycardias Usual rate: 150-250 bpm Prototypic patient: young to middle age, healthy female with no Structural Heart Disease Palpitations with sudden onset/offset, may be terminated by maneuvers that lead to AVN block Vagal maneuvers Adenosine AVNRT Mechanism: Reentry Required substrate: dual AV nodal physiology At least 2 separate pathways provide input into the AVN Fast pathway: rapid conduction, slower recovery Slow pathway: slow conduction, rapid recovery Typical form: short RP P waves not seen due to simultaneous A and V activation P waves distort terminal QRS pseudo r’ in v1, pseudo S waves in inferior leads Reentry in AVNRT A: slow B: fast 3 prerequisites 2 anatomically or functionally distinct conduction pathways Unidirectional block in 1 pathway Slowed conduction down second pathway Sinus Rhythm PAC Reentry 42 yo female with sudden onset palpitations, no PMHx Typical AVNRT AVNRT Acute Management Hemodynamically unstable Very rare with AVNRT Use ACLS algorithm Vagal Maneuvers Adenosine Hemodynamically stable 99% of all AVNRT cases Vagal maneuvers, adenosine, verapamil, diltiazem (Class 1) BB, digoxin, amiodarone (Class 2b) * Digoxin may be ineffective because its pharmacologic effects can be overridden by enhanced sympathetic tone AVNRT Chronic Management Determined by tolerance and frequency Well tolerated, spontaneous or easy termination Lifestyle modification, vagal maneuvers More frequent or bothersome attacks Pharmacotherapy-prophylactic, overall efficacy 30-65% Slow AVN conduction BB, verapamil, diltiazem, digoxin* Antiarrhythmic agents: Class Ic (no SHD) , III Daily therapy Pill-in-the-pocket (infrequent, prolonged, well-tolerated): flecainide, diltiazem + propranolol Frequent attacks despite prophylactic therapy Catheter ablation: slow pathway 90-95% success, 1% risk of permanent AV block AVRT Accounts for 30% of regular, NCTs More common in males Presents at younger age than AVNRT Extranodal accessory pathway connects myocardium of atrium to ventricle May exhibit antegrade (orthodromic) and retrograde conduction (antidromic) Antegrade conduction results in delta wave on surface EKG Incidence is 0.1 to 0.3% in general population Classified based on location along the TV or MV annulus Degree of preexcitation determined by relative conduction to ventricle over the AVN vs. AP Minimal preexcitation: latent Preexcitation Pattern Types of AVRT Antegrade / Orthodromic Retrograde / Antidromic AVNRT Conduction down accessory pathway is usually rapid, nondecremental During tachycardia if action potential conducted down accessory pathway can have 1:1 conduction Atrial fibrillation or flutter could lead to ventricular tachycardia 18 year old male with palpitations 18 year old male with palpitations AV Reentry - retrograde accessory pathway conduction p p Sinus rhythm - antegrade accessory pathway conduction delta -wave AVRT Acute Management Orthodromic (NCT)-same as AVNRT Antidromic (WCT)-goal: slow AP conduction Unless there is strong evidence supporting AVN dependence, adenosine, non-DHP CCB should be avoided Ventricular rate may increase in WCT due to AT or AFL with AP bystander conduction AVN blocking agents ineffective in AP-AP tachycardias Adenosine may produce AF with rapid ventricular rate Procainamide, ibutilide IV are agents of choice Pre-excited atrial fibrillation: slow AP conduction, convert AF Procainamide, ibutilide IV, DCCV if unstable AVRT-Antidromic 25 yo with a long history of tachypalpitations Preexcited Atrial Fibrillation Unstable: DCCV IV: procainamide, ibutilide Avoid agents that slow AV nodal conduction EPS/RFA AVRT Chronic Management Management guided by presence of pre-excitation, arrhythmia tolerance Concealed AP: pharmacologic management same as for AVNRT Pharmacologic therapy AVN blocking agents Verapamil, diltiazem, digoxin contraindicated with manifest pre-excitation Slow AP conduction-Class 1c,III antiarrhythmics Catheter ablation: Class 1 for manifest preexcitation with symptoms, poorly tolerated AVRT with concealed AP 95% success, 5% recurrence (higher for right-sided and septal APs) Risk location dependent: AV block, perforation, embolism Overall major complication rate should be <3% Focal Atrial Tachycardia Uncommon SVT in structurally normal hearts, common with SHD (atrial scarring) Clinical forms Incessant: tachycardia-induced cardiomyopathy Paroxysmal Nonsustained (very common on holters) Mechanisms: triggered activity, enhanced automaticity, reentry (micro) Rapid spread of activation from focal site Atrial rates 100 to 250bpm (rarely up to 300 bpm) Isoelectric baseline usually present between p waves Distinguishes focal AT from AFL AV blocks occurs AVN and ventricle are not required PR/RP interval depend on AV nodal conduction properties Long RP tachycardia-most common P wave morphology depends on site of origin in atrium P wave often obscured by T wave 62 year old female with occasional palpitations P Waves in Atrial Tachycardia V1 AVL SVC Left atrium Lateral Left Atrium Right Atrium IVC Septal: narrow p wave Cranial: (+) in inferior leads Caudal: (-) in inferior leads Tang et al JACC 1995 Focal Atrial Tachycardia: Sites of Origin RA: 75-85% SVC -Crista terminalis -TVA Other: 5-10% X RA App -CS os (7%) LA -SVC -RAA X LA: 10-15% -PVs (deep) -IVC -MVA -Vein of Marshall -PV ostia -CS muscle RA -LAA *can be generators for AF IVC Atrial Tachycardia Acute Treatment Hemodynamically unstable (rare): DCCV Terminates microreentry, triggered activity Hemodynamically stable Response/efficacy depends on mechanism Adenosine (2a) Termination: triggered activity Persistence with AV block: microreentry Transient atrial slowing: automaticity IV beta-blockers, CCB Termination (2a) Rate control through AV block (1) Second line: Ia, Ic, III AAD (2a) for direct suppression Focal Atrial Tachycardia: Chronic Management AT Pharmacologic Beta-blockers CCBs Class Ia, Ic, or III antiarrhythmic drugs Catheter Ablation: Efficacy: 80%-85% acute Drug refractory or incessant -tachycardia-induced CMP Problems: Inability to induce tachycardia Multiple tachycardias (10%) Nonsustained tachycardia Recurrence (8-10%) Focal Atrial Tachycardia Middle-aged women with palpitations Multifocal Atrial Tachycardia Differential Diagnosis of Wide-Complex Tachycardia VT SVT with aberrancy (atrial fibrillation/flutter) Antidromic AV reentry via WPW accessory pathway Atrial fibrillation, atrial flutter, atrial tachycardia, or AV nodal reentry in setting of WPW with rapid conduction down accessory pathway Bundle branch reentry Key ECG Signs Atrial activity Width of QRS QRS Axis QRS Configuration Identifying Atrial Activity P wave morphology relationship between P and QRS Capture beats AV Dissociation a Hallmark, yet VA conduction may be present Physical Exam- JVP, S1, SBP, Response to carotid sinus message QRS Width QRS width Wellens. Heart 2001;86:579-585 Site of origin- lateral wall vs. near septum Scar tissue, LVH, HCM >140ms in RBBB, >160ms LBBB; likely VT Septal origin may be narrower VT likely if width narrower than with sinus rhythm QRS Axis Assists in differentiation, localization and assessing etiology Inferior Axis- Basal origin Superior Axis- Apical origin Wellens et al. (Am J Med 1978)- RBBB with superior axis strongly suggests VT LBBB with inferior axis argues for RVOT tachycardia Wellens. Heart 2001;86:579-585 QRS Configuration Capture and Fusion Beats Leads V1 and V6 QRS intervals Concordance QR complexes Capture and Fusion Beats Capture Fusion Wellens. Heart 2001;86:579-585 A-V Dissociation, Fusion, and Capture Beats in VT V1 E ECTOPY F C FUSION Fisch C. Electrocardiography of Arrhythmias. 1990;134. CAPTURE Concordanc e Precodial leads share the same axis positive or negative Wellens. Heart 2001;86:579-585 Summary ECG Distinctions of VT from SVT with Aberrancy Favors VT Duration RBBB: LBBB: QRS > 0.14 sec. QRS > 0.16 sec. Axis QRS axis -90° to ±180° Favors SVT with Aberrancy < 0.14 sec. < 0.16 sec. Normal Summary ECG Distinctions of VT from SVT with Aberrancy Favors VT Favors SVT with Aberrancy Morphology Precordial concordance If LBBB: R V1 duration > 30 ms S wave > 70 ms S wave notched or slurred V6: qR or QR R wave monophasic If RBBB: V1: monophasic R wave qR If triphasic, R > R1 V6: R < S R < R1 Additional Features Left axis deviation >-30 useful Right axis deviation >+90 w/ LBBB pattern R to S nadir >100ms in 1 or more precordial leads QR complexes