* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Objectives - Contemporary Forums
Management of acute coronary syndrome wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Atrial septal defect wikipedia , lookup
Congenital heart defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
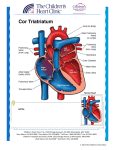
Speaker Potential Conflicts CONGENITAL HEART DEFECTS Pathophysiology, Hemodynamics and Clinical Recognition Mary Fran Hazinski, RN, MSN, FAAN, FAHA, FERC Compensated Senior Science Editor for Emergency Cardiovascular Care Programs, American Heart Association Professor, Vanderbilt University School of Nursing Nashville, TN CHD: For Additional Reading Please refer to detailed WORD handout provided on CF conference website Hazinski MF, Nieves J, Fosse G, Rummell M and others: Cardiovascular Problems, In Hazinski MF (Ed), Nursing Care of the Critically Ill Child, ed 3, Saint Louis, 2013, Mosby, an imprint of Elsevier If you don’t understand the child’s CHD Ask cardiologist to draw a picture Ask surgeon to draw a picture Keep references at hand to create pictures Objectives Provide framework and overview of the major classifications of defects and their hemodynamic consequences – Describe perinatal circulatory changes – Describe factors increasing and decreasing pulmonary vascular resistance – Provide overview of hemodynamic principles Highlight defects most common congenital heart Congenital Heart Defects CONGENITAL HEART DISEASE DEFINITION: Defect in heart or great vessels present from birth INCIDENCE: 8-10/1,000 live births (0.8-1.0% of all life births) Most multifactorial in origin May be part of genetic disease or syndrome (if so, look for other associated problems) May be isolated defect Often of multi-factorial inheritance with genetic predisposition See Fosse, G. Etiologies of Congenital Heart Disease; Non-Inherited and Genetic Factors, In Cardiovascular Problems chapter, In Hazinski, MF Nursing Care of Critically Ill Child ed 3, Saint Louis, 2013, Mosby. Fetal Circulation—Web figure Fetal circulation and perinatal circulatory changes Fetus: High pulmonary vascular resistance PERINATAL CHANGES Placental to pulmonary oxygenation Pulmonary blood flow increases, pulmonary vascular resistance falls Fetal shunts close Systemic vascular resistance rises Postnatal Circulation—© Ross Labs Reactive pulmonary vasoconstriction Postnatal Circulation: Pulmonary vascular resistance falls PULMONARY VASOCONSTRICTORS 4 H’S (Alveolar) Hypoxia Hydrogen ion (acidosis) Hyperdistension of alveoli Hypothermia PULMONARY VASODILATORS 6 A’S Alveolar oxygenation Alkalosis Appropriate tidal volume and temperature Analgesia Avoidance of stimulation ALSO: Administered nitric oxide and other vasodilators CHF: Causes in Neonatal Period CHD causing L heart/aortic obstruction Large shunt causing increased PBF Any large shunting lesions Pulmonary venous obstruction Cor pulmonale Uncommon causes Hemodynamic Principles “Happy heart” with normal pressure, flow and resistances Pressure This = Flow X Resistance copyrighted figure removed at request of speaker Effect of Increased Resistance Hemodynamic Principles—cont’d For Blood Right to left shunt CONGENITAL HEART DEFECTS Classification flow to remain unchanged, driving pressure must increase This copyrighted cartoon removed at request of the speaker Resistance to flow through pulmonary outflow tract must be greater than that through aortic outflow tract This copyrighted figure removed at request of speaker will flow in path of least resistance Acyanotic defects producing increased pulmonary blood flow or pulmonary obstruction Defects producing hypoxemia Defects resulting in left heart or aortic obstruction CONGENITAL HEART DEFECTS Classification Atrial Septal Defect—U Kansas fig Acyanotic defects producing increased pulmonary blood flow or pulmonary obstruction Defects producing hypoxemia Defects resulting in left heart or aortic obstruction Atrial septal defects--types Ventricular Septal Defect—U Kansas fig From: Kambam J, ed. Cardiac Anesthesia for Infants and Children. St Louis, Mosby, 1994 High pulmonary blood flow under high pressure = CHF Netter—CIBA illustration --copyrighted Ventricular Septal Defect with pulmonary vascular disease © MF Hazinski—do not reproduce without permission Patent ductus arteriosis ©U Kansas Atrioventricular Septal Defect U of Kansas figure AVSD—Complete Canal Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 AVSD—Complete Canal Repair Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 Double-Outlet RV --wth SubAo VSD, no PS—VSD type Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 SubPulm VSD without PS—TGA type Double-Outlet RV --wth SubAo VSD and PS—Tetralogy type Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 Pulmonary Valve Stenosis U Kansas figure Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 Pulmonary valve stenosis angiogram—©MF Hazinski Pulmonary valvuloplasty—cath From: Kambam J, ed. Cardiac Anesthesia for Infants and Children. St Louis, Mosby, 1994 CONGENITAL HEART DEFECTS Classification Pulmonary valvotomy Acyanotic defects producing increased pulmonary blood flow or pulmonary obstruction Defects producing hypoxemia Defects resulting in left heart or aortic obstruction HYPOXEMIA of Cardiac Origin PaO2 < 80 mmHg when patient breathing room air at sea level Central cyanosis (vs peripheral) Generally does not respond to O2 CHD: TGA, tetralogy, pulmonary atresia, truncus arteriosus, tricuspid atresia, single ventricle, TAPVC Newborn Hyperoxia Test Obtain baseline PaO2 from RIGHT radial artery Administer 100% oxygen for 10-15 minutes Obtain “post oxygenation” arterial sample from RIGHT radial artery – PaO2 <50mm Hg = probable cyanotic CHD, administer prostaglandins – PaO2 50-250 mm Hg = possible cyanotic CHD (consider prostaglandins) – PaO2 >250 mm Hg= cyanotic CHD unlikely Cyanotic Heart Disease Hypoxemia PaO2) (low Arterial oxygen content may be near normal (depends on [Hbg]) DO NOT ALLOW AIR TO ENTER ANY IV CATHETER Copyrighted cartoon removed at request of the speaker Tetralogy of Fallot—U Kansas fig Tetralogy of Fallot--surgery Palliative shunt to increase pulmonary blood flow Correction Tetralogy of Fallot Surgical Correction Truncus Arteriosus--I U Kansas figure Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 Truncus arteriosus repair— Modified Rastelli Figure © Hazinski, Nursing Care of Critically Ill Child, ed 3 Pulmonary atresia with VSD U Kansas figure Pulmonary atresia with intact ventricular septum—©U Kansas Pulmonary atresia with intact ventricular septum--Chest x-ray © Mary Fran Hazinski Pulmonary atresia with IVS RV sinuisoids Tricuspid atresia with VSD U Kansas figure In Kambam J, ed. Cardiac Anesthesia for Infants and Children. St Louis, Mosby, 1994 Bidirectional Glenn (SVC-PAs) © Nichols D (Ed), Critical heart disease in infants and children, Edition 3, Saint Louis, 2008 Mosby. Fontan—original procedure Fontan—extracardiac Fontan Transposition of the Great Arteries—U Kansas figure Sidebotham D, McKee A, Gillham M, and others. Cardiothoracic Critical Care. Philadelphia, Butterworth Heinemann/Elsevier, 2007 Transposition—parallel circulations Transposition—Arterial switch (Jatene procedure) From Kambam J. Transposition of the great arteries. In Kambam J, ed.., Cardiac Anesthesia for Infants and Children. St Louis, Mosby, 1994 From Kambam J Transposition of the great arteries In Kambam J ed CONGENITAL HEART DEFECTS Classification Acyanotic defects producing increased pulmonary blood flow or pulmonary obstruction Defects producing hypoxemia Defects resulting in left heart or aortic obstruction Coarctation of the Aorta U of Kansas figure angio © MF Hazinski Aortic Stenosis Copyrighted cartoon removed at request of the speaker Hypoplastic Left Heart Syndrome © MFHazinski art Hypoplastic Left Heart Syndrome If too much pulmonary blood flow CHF Poor systemic perfusion High SaO2 (>80%) © Nichols D (Ed), Critical heart disease in infants and children, Edition 3, Saint Louis, 2008 Mosby. Norwood Procedure—his art from NEJM PULMONARY VASOCONSTRICTORS 4 H’S (Alveolar) Hypoxia Hydrogen ion (acidosis) Hyperdistension of alveoli Hypothermia Hypoplastic Left Heart Syndrome If too little pulmonary blood flow Severe hypoxemia Adequate systemic perfusion Low SaO2 (<70%) © Nichols D (Ed), Critical heart disease in infants and children, Edition 3, Saint Louis, 2008 Mosby. PULMONARY VASODILATORS 6 A’S Alveolar Alkalosis Appropriate framework and overview of the major classifications of defects and their hemodynamic consequences – Describe perinatal circulatory changes – Describe factors increasing and decreasing pulmonary vascular resistance – Provide overview of hemodynamic principles Highlight defects most common congenital heart Avoidance Allen HD, Driscoll DJ, Feltes TF, Shaddy RE, eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents, Including the Fetus and Young Adult, ed 7. Philadelphia, Lippincott Williams & Wilkins, 2008 (see specific defects and Cardiac Intensive Care chapters in this excellent text). Castaneda Ar, Jonas RA, Mayer JE, and Hanley FL: Cardiac surgery of the Neonate and Infant, Philadelphia, 1994, WB Saunders. Chang AC, Hanley FL, Wernovsky G, Wessel DL, eds. Pediatric Cardiac Intensive Care. Baltimore, Williams & Wilkins, 2008. Hazinski MF (Ed), Cardiovascular disorders (with additional authors), In Hazinski MF (Ed), Nursing Care of the critically ill child, edition 3, Saint Louis 2013, Mosby. Hazinski MF: Cardiovascular disorders, In Hazinski MF (Ed), Manual of Pediatric Critical Care, Saint Louis, 1999, Mosby Year Book. Wilson W, Taubert KA, Gewitz M, and others. Prevention of Infective Endocarditis Guidelines From the American Heart Association: A Guideline From the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 2007;116:1736-1754. of stimulation ALSO: Administered nitric oxide and other vasodilators References Hazinski MF, Nieves J, Fosse G, Rummell M and others. Cardiovascular problems, In Hazinski MF (Ed), Nursing Care of the Critically Ill Child, ed 3, Saint Louis, Mosby, In Press. Nichols DG, Cameron DE, Greeley WJ, Lappe DG, Ungerleider RM and Wetzel RC: Critical heart disease in infants and children, Edition 3, Saint Louis, 2008, Mosby Year-Book. The Society of Thoracic Surgeons. STS Congenital Heart Surgery Data Summary, 2006-2010 Procedures, All Patients. Available at: http://sts.org/sites/default/files/documents/STSCONGAllPatientsSummary_Fall2010.pdf Accessed 03/28/11. Wernovsky G, Chang AC, Wessel DL, Ravishankar C. Cardiac intensive care. In Allen HD, Driscoll DJ, Feltes TF, Shaddy RE eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents, Including the Fetus and Young Adult, ed 7. Philadelphia, Lippincott Williams & Wilkins, 2008. OXYGEN DELIVERY References--additional tidal volume and temperature Analgesia Objectives Provide oxygenation Arterial Oxygen Content: ([Hgb]X sat’n X1.34 ml/Gm)+0.003 X PaO2 Oxygen Delivery: O2 Content X C.O./C.I X 10 CYANOTIC CHD Potential Complications Polycythemia, thromboembolic events Hypercyanotic episodes Coagulopathies Brain abscesses HYPERCYANOTIC EPISODES: Characteristics Hyperpnea Irritability Prolonged crying Increasing cyanosis Profound hypoxemia, acidosis Ultimate loss of consciousness HYPERCYANOTIC EPISODES: Treatment Place infant in knee-chest position Administer oxygen Administer morphine sulfate Consider sodium bicarbonate or propranolol Urgent surgical intervention NORWOOD STAGE I FOR HLHS: Goals Establish permanent, unobstructed communication between right ventricle and aorta/systemic circulation Limit pulmonary blood flow Provide adequate intraatrial communication PROSTAGLANDIN E1 Preparation of Infusion 0.3 mg/100 cc =300 mcg/100 cc (3 mcg/cc) 1.0 ml/kg/hr= 0.05 mcg/kg/min Titrate to effect (improved pulmonary or systemic blood flow) NORWOOD STAGE II FOR HLHS: Goals Separation of pulmonary and systemic circulations Assurance of unimpeded pulmonary venous return and pulmonary and systemic blood flow I