* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CASE 1: IMPETIGO
Marburg virus disease wikipedia , lookup
Gastroenteritis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Leptospirosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Foodborne illness wikipedia , lookup
Sarcocystis wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Onchocerciasis wikipedia , lookup
Mycoplasma pneumoniae wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Anaerobic infection wikipedia , lookup
Schistosoma mansoni wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Listeria monocytogenes wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Neonatal infection wikipedia , lookup
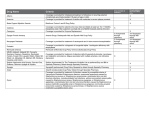
CASE 1: IMPETIGO What could be the culprit? Based on the signs and symptoms that Stephanie presents with, particularly the characteristic red sores found around her mouth and nose as well as her rash and lack of fever (afebrile), she potentially has a skin disease called impetigo (Figure 1A).[1][2] Certain groups within a population are especially more likely to develop this disease, including children who are aged two to six.[6] Stephanie falls into this category as well. The two bacterial pathogens that are most commonly identified in clinical isolates from patients afflicted with impetigo are 1) Streptococcus pyogenes (or Group A Streptococcus) (Figure 1B) and 2) Staphylococcus aureus.(Figure 1C)[3] A) B) C) Figure 1- Presentation of Impetigo and Causative Agents A) A child with the characteristic red sores in the perioral region[34]. B) Streptococcus pyogenes or Group A Streptococcus[35] C) Staphylococcus aureus[36] Bacterial Pathogenesis I. ENCOUNTER Streptococcus pyogenes: Geographical Distribution and Mechanisms for Survival S. pyogenes is a prevalent human specific pathogen that exists around the world.[7] It has been estimated that this bacterium is responsible for more than 600 million cases of throat-related infections and more than 100 million cases of skin diseases in children in developing countries annually.[8] It can be found in both temperate and warm/humid climates, but more specifically, manifestations of disease differ from country to country depending on these conditions.[4][5] It is more common to find streptococcal pharyngitis in temperate areas and impetigo in warm and humid areas.[5] Additionally, there are seasonal differences in some countries, whereby pharyngitis predominates during the wintertime and impetigo emerges during the summer.[7] Survival of S. pyogenes outside of the host and in the environment is likely in part facilitated by the presence of a bacterial capsule (it is a gram positive bacterium).[9] It was initially believed that this bacterium rapidly dies once it is no longer in contact with the human host as a result of desiccation and rapid loss of infectivity.[10] Of note, it has been found that it has the ability to form a biofilm outside of the host, allowing for the bacterium to remain viable for extended periods of time, while remaining infectious.[10] This was not the case when the bacteria were in a planktonic state, where they rapidly loss viability on both biotic (hands) and abiotic (plastic) surfaces.[10] Staphylococcus aureus: Geographical Distribution and Mechanisms for Survival S. aureus is a bacterial pathogen not limited to humans that has a global distribution.[11] It is one of the most common sources of skin and soft-tissue infections.[11] To put this in perspective, it is believed that roughly 20% of people are considered persistent carriers of this bacterium (with children being more likely to belong to this category) and 60% are considered intermittent carriers.[11] Although incidence is increasing, methicillin-resistant S. aureus is less prevalent than methicillin-susceptible S. aureus.[12] The presence of a bacterial capsule likely enhances survival outside of the host (the bacterium is gram positive).[13] Streptococcus pyogenes: Normal Host Tissue Residence and Mechanisms for Survival S. pyogenes does not normally reside on the skin.[14] The throat and skin are the primary reservoirs of S. pyogenes.[7] Additionally, S. pyogenes can also exist in asymptomatic carriers in a quiescent commensal-like state in the throat.[7] As an example, it can be found in the throat of 15% of school-aged children.[14] Other locations where these bacteria can be found in a carrier state include the vagina and the anus.[5] Staphylococcus aureus: Normal Host Tissue Residence and Mechanisms for Survival S. aureus is a commensal of the human body, whereby it is believed that close to 30% of the human population is colonized with it.[16] As an opportunistic bacterium, S. aureus may transiently colonize the skin of certain susceptible populations such as newborns.[14] It typically resides on skin surfaces of the body, especially openings.[15] Some examples of such locations include the nose, the mouth, the genitals, and the rectum.[15] Streptococcus pyogenes: Transmission S. pyogenes is a microbe that is highly communicable and people can come in contact with it in many different ways. Bacteria can be spread through contact with mucus originating from the nose or throat of someone who is infected on both biotic and abiotic surfaces.[17] Additionally coming in contact with infected wounds or sores also has a similar effect.[17] Methods in which the skin is broken allows the bacterium to enter the body and these include animal bites, insect bites, and trauma to the skin.[6][18] Waterborne and foodborne transmission has also been reported.[19] Generally, hygiene is a very important issue and fingernails and the perianal region have been cited as a common way of dissemination.[19] Staphylococcus aureus: Transmission The most common way that S. aureus is transmitted is by coming in contact with people who have contaminated hands.[20] This bacterium is also a cause of food poisoning through the secretion of enterotoxins into food and its subsequent ingestion.[21] Touching infected lesions or a carrier of the bacteria can facilitate transmission between people.[11] Chances for exposure are increased in environments or communities that are unsanitary and crowded.[11] II. ENTRY Streptococcus pyogenes: Adhesion, Invasion, and Site Specificity S. pyogenes expresses various virulence factors anchored to the cell wall in order to facilitate their attachment to human epithelial cells of the pharynx and skin and subsequent invasion (Figure 2).[22] This includes fimbrial-like proteins, fimbrial-like proteins that bind to extracellular matrix proteins such as fibronectin, laminin, and collagen, and M proteins (which are used as a diagnostic for identifying specific strains).[22][23][24][25] It was also reported that different M serotypes of S. pyogenes corresponded to the tendency to cause infection in the throat or the skin and not often simultaneously.[7][26] More specifically, the M protein has been shown to interact with glycosaminoglycans found on the host cell surface and extracellular matrix, which promotes adhesion.[32] This bacterium is a predominantly extracellular pathogen and certain serotypes also encode protein F1 (PrtF1/Sfbl), which not only aids in adhesion, but also inhibits the deposition of C3 (a complement component) and prevents phagocytosis.[25] Despite this, when it does get phagocytosed, many proteins involved in adherence such as the M protein allows the bacterium to persist and survive intracellularly.[25] Figure 2- Virulence Factors of Group A Streptococcus Schematic representation of some of the virulence factors that GAS uses and for what purpose in the environment of the pharynx. Figure adapted from (Olsen, 2009)[25]. Staphylococcus aureus: Adhesion, Invasion, and Site Specificity S. aureus employs various molecules to facilitate its adhesion and invasion of host epithelial cells (Figure 3).[27] Of note, teichoic acids aid the binding of nasal epithelial cells and fibronectin.[14] Virulence factors that mediate the adherence to the extracellular matrix are collectively organized under the term MSCRAMM (microbial surface components recognizing adhesive matrix molecules).[14] Within this term, many proteins have been suggested to play important roles for S. aureus adhesion, but the two most notable ones are clumping factor B and the above mentioned teichoic acid.[27] It is believed that this bacterium survives well both intracellulary and extracellularly.[27] Specifically, upon activation of the immune response, the bacterium upregulates multiple virulence factors such as clumping factor A on its surface capsule, which functions to inhibit opsonization and phagocytosis.[27] It has also been shown that S. aureus infection can occur post-viral infection with influenza, which damages the mucosal lining of the upper airway, resulting in a predisposition to S. aureus pneumonia.[27] This damaging likely exposes extracellular matrix components to which the bacteria can bind. Figure 3- Virulence Factors of Staphylococcus aureus Schematic representation of some of the virulence factors employed by S. aureus and their purpose. Figure adapted from (Todar, n.d.).[30] III. MULTIPLICATION AND SPREAD Streptococcus pyogenes: Multiplication and Spread Starting as a superficial infection of the skin or the throat, S. pyogenes can spread into deeper tissue.[28] This can result in necrotizing fasciitis.[28] Other complications/secondary sites of infection include examples such as sepsis, pneumonia, and meningitis.[28] More specifically, the colonization of the upper respiratory tract or pharynx, may result in spreading to other locations of the respiratory tract both upper and lower, which can ultimately cause infections of the middle ear, sinuses, and lungs.[29] Meningitis can be a result of the spread of the bacterium from middle ear or sinus infection or by way of the blood stream after pneumonia.[29] As mentioned above, S. pyogenes generally stays extracellularly, but in some serotypes, the bacterium has the ability to successfully persist and survive intracellularly.[25] Staphylococcus aureus: Multiplication and Spread Once in the host, S. aureus has to fight the immune response and it normally does this with a relatively high amount of difficulty.[30] As a result of this, in humans, infection by this bacterium is generally localized at the site of entry.[30] One of the main and most serious complications/secondary site of infection to infection is bacteremia, whereby the bacteria enter the bloodstream and this can be potentially fatal.[30] As previously mentioned, this S. aureus can successfully survive both intracellularly and extracellularly once it has properly colonized.[27] IV. BACTERIAL DAMAGE TO THE HOST Streptococcus pyogenes: Damage to the Host Extracellular products and toxins produced by S. pyogenes play a major role in cytotoxicity and the inflammatory response.[19] These can be broadly categorized into hemolysins, pyrogenic exotoxins, nucleases, and other products.[19] The two main hemolysins include Streptolysin S and Streptolysin O.[19] Streptolysin S is oxygen-stable leukocidin that functions to damage polymorphonuclear leukocytes and organelles, but is not in itself immunogenic.[19][29] Streptolysin O is an oxygen-labile leukocidin, which is cytotoxic to various cell types including the myocardium and is highly immunogenic.[19][29] Reactivity to the myocardium has implications in the generation of non-rheumatic myocarditis.[31] S. pyogenes possess four main progenic exotoxins called streptococcal pyorgenic exotoxins A, B, C, and F (SPE A, B, C, F).[19] These exotoxins are the main cause of the rash present in scarlet fever (and potentially impetigo).[19] SPE A, C, and F also have the ability to be superantigens, resulting in febrile symptoms, induced T cell proliferation, and induced cytokine production (including IL-1β, IL-6, and TNF).[19] It has been suggested that this is potentially due to their ability to bind both the T cell receptor and MHC-II.[19] S. pyogenes also has four nucleases (A, B, C, and D), which function in the liquefaction of pus in order to generate substrates for growth.[19] Finally, this bacterium also has the leukotoxic NADase, hyaluronidase (which can degrade both its own hyaluronan capsule as well as the host connective tissue), streptokinase (which acts in fibrinolysis), and Streptodornases A, B, C, and D, which are deoxyribonucleases.[19][29] Proteases also play a key role in the generation of soft tissue necrosis and toxic shock syndrome.[29] Of note, proteolysis of the epidermis and subepidermal layers of the skin is the main mechanism in which the bacteria employs to spread along skin layers, resulting in the characteristic blisters and pus-containing lesions in impetigo.[19] Staphylococcus aureus: Damage to the Host In general, many toxins secreted by S. aureus are potentially the cause of symptoms.[13] A variety of mechanisms are behind this, which are mainly as a result of the release of toxins and this includes the following: disruptions to cellular membranes, toxin-mediated septic shock, and toxin-mediated toxic shock.[13] More specifically, the membrane damaging toxins include the α-toxin, β-toxin, δ-toxin, γ-toxin, and leukocidin.[13] α-toxin forms a pore in target cells allowing cations to enter.[13] Platelets and monocytes are especially susceptible to α-toxin as a result of possessing high affinity sites.[13] This specific targeting then results in the release of eicosanoids and cytokines and ultimately he generation of the symptoms associated with septic shock.[13] γ-toxin and Pantan and Valentine (PV) leukocidin act as a two-component toxin system, which damages host cell membranes.[13] Three subunits come from the γ-toxin, namely A, B, and C, with B and C forming a leukotoxin that is weakly hemolytic, and A and B forming a hemolysin that is weakly leukotoxic.[13] On the other hand, the PV leukocidin is potently leukotoxic, but non-hemolytic.[13] PV leukocidin plays a major role in necrotizing fasciitis.[13] S. aureus also produces a variety of superantigens including enterotoxins (of which there are six serotypes, A, B, C, D, E, and G) and toxic shock syndrome toxin (TSST-1).[13] The enterotoxins are one of the main causes of staphylococcal food poisoning and the resulting diarrhea and vomiting.[13] When systemically expressed, toxic shock syndrome can result.[13] TSST-1 is the primary cause of toxic shock syndrome (at 75% of cases) and this is the result of the lack of specific host neutralizing antibodies.[13] These superantigens may stimulate T cells non-specifically by binding to both the T cell receptor and MHCII, resulting in massive cytokine release and the subsequent symptoms of toxic shock syndrome.[13] This bacterium can also produce epidermolytic (exfoliative) toxin (ET), which results in blistering and the loss of epithelium.[13] Two distinct forms of the toxin exist, namely ETA and ETB.[13] Bullous impetigo is mainly caused by these two toxins.[33] They cause the loss of adhesion between the cells of the superficial dermis, resulting in blisters and skin being sloughed off.[33] References: 1. Mayo Clinic Staff. (2013, May 15). Disease and Conditions- Impetigo. Symptoms. Retrieved from http://www.mayoclinic.org/diseasesconditions/impetigo/basics/symptoms/con-20024185 2. Bacterial Skin Infections: Impetigo and MRSA. (2011, February). Retrieved from https://www.health.ny.gov/diseases/communicable/athletic_skin_infections /bacterial.htm 3. Ibrahim F., Khan T., & Pujalte G. G. A. (2015). Bacterial Skin Infections. Primary Care Dermatology, 42, 485-499. doi:10.1016/j.pop.2015.08.001 4. Parker M.T. (1967). International Survey of the Distribution of Serotypes of Streptococcus pyogenes (Group A Streptococci). Bulletin of the World Health Organization, 37, 513-527. 5. Public Health Agency of Canada. (2010). Streptococcus Pyogenes. Retrieved from http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/streppyogenes-eng.php 6. Martel J. (2012, June 25). Impetigo. Who Gets Impetigo? Retrieved from http://www.healthline.com/health/impetigo#RiskFactors3 7. Bessen D.E. & Lizano S. (2010). Tissue tropisms in group A streptococcal infections. Future Microbiology, 5, 623-638. doi: 10.2217/fmb.10.28 8. Carapetis J.R., Steer A.C., Mulholland E.K., & Weber M. (2005). The global burden of group A streptococcal diseases. The Lancet: Infectious Diseases, 5, 685-694. doi:10.1016/S1473-3099(05)70267-X 9. Patterson MJ. Streptococcus. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 13. Available from: http://www.ncbi.nlm.nih.gov/books/NBK7611/ 10. Marks L.R., Reddinger R.M., & Hakansson A.P. (2014). Biofilm Formation Enhances Fomite Survival of Streptococcus pneumonia and Streptococcus pyogenes. Infection and Immunity, 82, 1141-1146. doi:10.1128/IAI.01310-13 11. Public Health Agency of Canada. (2012). Staphylococcus Aureus. Retrieved from http://www.phac-aspc.gc.ca/lab-bio/res/psdsftss/staphylococcus-aureus-eng.php#footnote3 12. Grundmann H., Aanensen D.M., van der Wijngaard C.C., Spratt B.G., Harmsen D., & Friedrich A.W. (2010). Geographic Distribution of Staphylococcus aureus Causing Invasive Infections in Europe: A Molecular-Epidemiological Analysis. PLOS Medicine, 7, e1000215. doi: 10.1371/journal.pmed.1000215 13. Patterson MJ. Streptococcus. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 12. Available from: http://www.ncbi.nlm.nih.gov/books/NBK7611/ 14. Chiller K, Selkin B.A., & Murakawa G.J. (2001). Skin Microflora and Bacterial Infections of the Skin. Journal of Investigative Dermatology Symposium Proceedings, 6, 170-174. doi:10.1046/j.0022202x.2001.00043.x 15. Human Diseases and Conditions Forum. (n.d.). Staphylococcal Infections. Retrieved from http://www.humanillnesses.com/Infectious-Diseases-SkZ/Staphylococcal-Infections.html 16. Tong S.Y.C., Davis J.S., Eichenberger E., Holland T.L., & Fowler Jr. V.G. (2015). Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clinical Microbiology Reviews, 28, 603-661. doi: 10.1128/CMR.00134-14 17. Center for Disease Control. (2014). Group A Streptococcal (GAS) Disease. Retrieved from http://www.cdc.gov/groupastrep/about/faqs.html 18. Moskowitz R.J. (2014). Impetigo. Retrieved from https://www.nlm.nih.gov/medlineplus/ency/article/000860.htm 19. Khan Z.Z. (2015). Group A Streptococcal Infections. Retrieved from http://emedicine.medscape.com/article/228936-overview#a4 20. Minnesota Department of Health Fact Sheet. (2010). Staphylococcus aureus. Retrieved from http://www.health.state.mn.us/divs/idepc/diseases/staph/basics.html 21. Le Loir Y., Baron F., & Gautier M. (2003). Staphylococcus aureus and food poisoning. Genetics and Molecular Research: GMR, 2, 63-76. 22. Terao Y. (2012). The virulence factors and pathogenic mechanisms of Streptococcus pyogenes. Journal of Oral Biosciences, 54, 96-100. doi:10.1016/j.job.2012.02.004 23. Terao Y., Kawabata S., Kunitomo E., Nakagawa I., & Hamada S. (2002). Novel laminin-binding protein of Streptococcus pyogenes, Lbp, is involved in adhesion to epithelial cells. Infection and Immunity, 70, 993-997. doi: 10.1128/IAI.70.2.993-997.2002 24. Podbielski A., Woischnik M., Leonard B.A.B., & Schmidt K-H. (1999). Characterization of nra, a global negative regulator gene in group A streptococci. Molecular Microbiology, 31, 1051-1064. doi:10.1046/j.13652958.1999.01241.x 25. Olsen R.J., Shelburne S.A., & Musser J.M. (2009). Molecular mechanisms underlying group A streptococcal pathogenesis. Cellular Microbiology, 11, 1-12. doi:10.1111/j.1462-5822.2008.01225.x 26. Wannamaker L.W. (1970). Difference between Streptococcal Infections of the Throat and of the Skin. New England Journal of Medicine, 282, 23-31. doi:10.1056/NEJM197001012820106 27. Liu G.Y. (2009). Molecular Pathogenesis of Staphylococcus aureus Infection. Pediatric Research, 65, 71R-77R. doi:10.1203/PDR.0b013e31819dc44d 28. Cunningham M.W. (2000). Pathogenesis of Group A Streptococcal Infections. Clinical Microbiology Reviews, 13, 470-511. doi:10.1128/CMR.13.3.470-511.2000 29. Todar K. (n.d.). Streptococcal pyogenes and Streptococcal Disease. Retrieved from http://textbookofbacteriology.net/streptococcus_2.html 30. Todar K. (n.d.) Staphylococcus. Retrieved from http://textbookofbacteriology.net/staph_2.html 31. Calabrese F. & Thiene G. (2003). Myocarditis and inflammatory cardiomyopathy: microbiological and molecular biological aspects. Cardiovascular Research, 60, 11-25. doi:http://dx.doi.org/10.1016/S00086363(03)00475-9 32. Frick I.M., Schmidtchen A. & Sjobring U. (2003). Interactions between M proteins of Streptococcus pyogenes and glycosaminogylcans promote bacterial adhesion to host cells. European Journal of Biochemistry, 270, 2303-2311. doi:10.1046/j.1432-1033.2003.03600.x 33. Lewis L.S. (2015). Impetigo. Retrieved from http://emedicine.medscape.com/article/965254-overview#a3 34. Impetigo. (2015). Retrieved from http://www.medicinenet.com/impetigo/article.htm 35. Kuehn B.M. (2013). Limited Access to Critical Antibiotic Leaves Patients in Many Parts of the World Vulnerable to Rheumatic Fever. news@JAMA. Retrieved from http://newsatjama.jama.com/2013/09/26/limited-access-tocritical-antibiotic-leaves-patients-in-many-parts-of-the-world-vulnerable-torheumatic-fever/ 36. Methicillin-Resistant Staphylococcus Aureus. (n.d.). Retrieved from http://www.bacteriainphotos.com/MRSA_images.html