* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download - Wiley Online Library
Survey
Document related concepts
Transcript
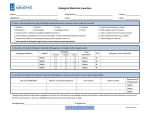
v?&&J IMMUNOLOGY AND MEDICAL MICROBIOLOGY ELSEVIER FEMS Immunology and Medical Microbiology I3 ( 1996) 8 l-86 Coagulase-negative staphylococci isolated from two cases of toxic shock syndrome lack superantigenic activity, but induce cytokine production G. Lina ‘. *, A. Fleer b, J. Etienne ‘, T.B. Greenland ” lGpl,nrtmrrtt de Rrcherchr en BactCriologie Midicale (UPR ES). Faclrlti dr MCdrcine ‘, F. Vandenesch Akis Carrel. Rue G~ti//awne a Porndin. 69372 LJY~ Cede.r 08, Frcm1.e ’ Eijhman- Wirzkler Laboratoy ’ Lrrboratoire d’bnmuwlo~ie of Medical et Biologic Microbiology and Wilhelmina 3501 CA Utrecht. The Nrther1and.s Pulmantrire. HGpitcd Curdiologiyw Received 25 May 1995; revised I9 September Chiidrerz ‘5 Hospital, PO Bar IXOOY. Lo~tis Prtrdel. BP L,wm Cedes 03. Frtrncu 1995: accepted 19 September 1995 Abstract Two strains of Sruph$ococ~rcs epidernzidis isolated from patients with toxic shock symptoms have been reported to carry genes related to S. uurer~s enterotoxins B and C by dot-blot hybridisation, although the corresponding superantigenic toxins were not detected immunologically. We here show that these strains produce no superantigens capable of stimulating proliferation of human mononuclear leukocytes or rabbit splenocytes, and that no DNA homologous to the seb or set genes can be detected by PCR. However, stimulation of human monocytes by whole killed bacteria induced dose-dependent production of the cytokines TNFcr. IL-I /3 and IL-6. which may be responsible for the clinical symptoms in these patients. Keword.s: Tumor necrosis factor-m: Interleukin- 1p: Interleukin-6: Staph$ocowu.s 1. Introduction Coagulase-negative staphylococci are increasingly being recognised as important pathogens, especially for patients in surgical, haemato-oncological or intensive care units [I]. Stuphvlococcu.s epidermidis is frequently responsible for nosocomial infections and can cause shock symptoms which are clinically se- Corresponding author. Present address: Laboratoire Central de Microbiologic. BItiment 10, Hapital Edouard Herriot. Place d’Arsonva1, 69437 Lyon Cedex 03. France. Tel.: +33 72 1 I 07 62: Fax: +33 72 11 07 64. 09X%8244/96/$1 5.00 Q 1996 Federation SSDI 09’8.8244(95)00087-9 of European Microbiological epidermidk vere [X] in up to 30% of patients with bacteraemia; half of these patients die [3]. Shock may be induced by several distinct mechanisms. Cases associated with Gram-negative bacteria result from the overstimulation of macrophages by lipopolysaccharide (LPS) present in the outer membrane. The activated macrophages produce excessive amounts of cytokines such as tumor necrosis factor alpha (TNFcx) and interleukins 1p and 6 (IL- 1 p; IL-6) [4] which contribute to the shock symptoms. Certain Gram-positive bacteria can induce shock through a similar mechanism where peptidoglycan and teichoic acid cell wall components stimulate cytokine production by monocytes. The shock thus Societies. All rights reserved G. Lina et al. / FEMS Immunology 82 and Medical produced by S. aureus and S. epidermidis in experimental animals closely resembles that induced by Escherichia coli [5,6]. Other Gram-positive bacteria induce shock through the production of extracellular toxins with superantigenic properties. These induce polyclonal MHC-dependent T cell proliferation with, again, release of TNFo, IL-l p, IL-6 and y-interferon, generally accounting for the observed symptoms of toxic shock syndrome (TSS) [7,8]. Two strains of S. epidermidis isolated from patients whose symptoms fitted the CDC definition for toxic shock syndrome (TSS) induced by superantigen [9] gave a positive signal on dot-blot hybridisation with oligoprobes recognising S. aureus genes coding for enterotoxins -B and -C (SEB and SEC), but antisera to SEB or SEC failed to recognise components in the culture supematants [lo]. An antigenitally novel, but genetically related toxin was envisaged. In this paper we re-examine the evidence for toxin production by these two S. epidennidis strains, and test the alternative hypothesis of cytokine induction in macrophages through cell wall components. 2. Materials and methods 2.1. Bacterial strains S. epidennidis strains N860094 and N900057 derive from blood cultures of two patients with TSS symptoms (fever, hypotension, rash and multiple organ failure leading to death in one case); strain 354 was used as an unrelated control. Defined strains of S. aureus were used to evaluate enterotoxin production: RN450 (sea - , seb - , set - 1; FRIS6 (sea - , seb + , set-1); FR1137 (sea-, seb-, secf). Strains were stored at - 80°C until used. 2.2. PCR amplification of seb and set Genomic DNA was extracted from staphylococcal cultures [ll] and used as template for amplification using primers previously shown to be specific for seb and set [ 12,131. Seb 1 (5’~GAGAGTCAACCAGATCCTAAACCAG-3’1, seb2 (5’-ATACCAAAAGCTATTCTCATTTTCT-3’1, set 1 (5’- Microbio1og.v 13 119961 RI -86 GACATAAAAGCTAGGAATTT-3’) and sec2 (5’AAATCGGATTAACATTATCC-3’1 were synthesised on a Applied Biosystems 39 1 DNA synthesiser (Perkin-Elmer, Montagny-le-Bretonneux, France). After amplification for 30 cycles (1 min denaturation at 94°C 1 min annealing at 55°C and 1 min extension at 72°C) the products were analysed by electrophoresis through 1% agarose gels (Sigma, Saint Quentin Fallavier, France). 2.3. Mitogenic natants actioity qf staphylococcal super- Exoproteins were prepared from overnight cultures of staphylococci in brain-heart infusion by precipitation with 5 ~01s. of 98% ethanol for 2 days at 4°C. After drying at 2O”C, the precipitate was resuspended in l/50 vol. pyrogen-free distilled water, filtered through Ultrafree UFCCTHK (100 kDa cutoff) cartridges and concentrated on MC UFC3LGC (10 kDa cutoff) filters (both from Millipore, Molstein, France). Human peripheral blood mononuclear cells were prepared from blood of healthy donors (Centre de Transfusion, Lyon. France) on Ficoll Hypaque (Lymphoprep, Nycone, Norway) gradients [ 141 and resuspended in RPM1 1640 medium (Gibco, Grand Island, NY) supplemented with 10% heat-inactivated foetal calf serum at lo5 cells ml-‘. Individual wells of 96-well microtitre plates were seeded with 100 ~1 of cell suspension and 100 ~1 of staphylococcal supernatant to give final concentrations of 0, 1/ 100, l/10 and l/l relative to the initial staphylococcal culture. After incubation for 48 h at 37°C in humidified 5% CO? in air, I &i of [3H]thymidine (1 Ci mM_‘; CEA, Saclay, France) in 10 ~1 was added to each well and the culture was continued for 24 h. Cells were harvested on glass-fibre filters and their radioactivity was evaluated in a Packard scintillation counter. Results are expressed as cpm k standard error of the mean in triplicate cultures. Alternatively, splenocytes were prepared by gently teasing apart spleens aseptically removed from New Zealand rabbits (ESD, ChPtillon sur Chalaronne, France). After removal of aggregates by passage through nylon wool, the suspensions were adjusted to 10’ cells ml-’ and incubated with staphylococcal supematant as described above. G. Lina et al. / FEMS Immunology 2.4. Cytokine production after staphylococcal lation of human monocytes and Medical 3. Results PCR amplification from bacterial DNA of the two S. epidetmidis strains associated with TSS using primers specific for the seb and set genes from S. epidermidis Brain heart solution S. epidermidis N900057 S. epidermidis N870094 S. artreu.~ FRIS6 S. rrureus RN420 undiluted l/100 l/10 undiluted l/l00 l/10 undiluted l/100 l/10 undiluted l/100 l/IO undiluted Measures are the mean of three determinations. set seb Fig. I. PCR amplification of staphylococcal toxin genes srb and SYCfrom S. rpidermidis isolated from TSS patients and S. ~II~~IL~ reference strains. Lanes A. S. aureus RN450 (srh - : SK - ): Lanes 3, S. aure~.< FRIS6 (seh + : src - 1: Lanes C, S. (twe~s FRI 137 ( seb - ; WC+ ): Lanes D. S. epidennidis N900057; Lanes E, S. epidermidis N870094. seb: amplification using primers seb 1 and seb 2: SK: amplification using primers set I and set 2. aureus produced no detectable signal, whereas the control S. aureus strains gave a clearly positive result (Fig. I). This is in contradiction with observations that DNA from the S. epidermidis strains can hybridise with oligonucleotide probes for these genes [lo]. We attempted amplifications where one of the PCR primers for each gene was replaced by an oligonucleotide previously used as probe, and amplifications using lower annealing temperatures but no positive signals were obtained (data not shown). Mutations in the gene regions corresponding to the primers could nevertheless have prevented amplification, so we tested the biological activity of culture supematants from the two strains of S. epidermidis. incorporation by rabbit splenocytes or human monocytes isolated from TSS patients or S. awew reference strains Stimulant added 83 13 f 19Y6181-86 stimu- S. epidermidis colonies were freshly inoculated into Muller-Hinton broth and incubated at 37°C for 18 h. Harvested cells were washed X 3 in phosphate-buffered saline, pH 7.4, counted spectrometrically and inactivated by heating at 60°C for 30 min. Suspensions for stimulation of human monocytes were adjusted to the equivalent of 5 X 10’” CFU ml-‘. Incubation on blood agar plates confirmed the absence of living bacteria in the heated suspensions. Human peripheral blood monocytes were prepared and incubated with the killed bacteria as described in [6]. Briefly, 100 ~1 of bacteria1 suspension at the indicated concentrations was added to IO6 adherent monocytes in 96-well flat-bottomed culture plates. After 18 h incubation, the supernatants were removed and centrifuged, then cytokine concentrations were evaluated by enzyme immunoassay as described in [14]. Measurements are expressed as ng ml-’ of cytokine. Table I [‘H]Thymidine Microbinlq~y (PBMC) incubated with supernatants from cultures Rabbit splenocytes (cpm f SEM ) PBMC (cpm & SEM) 667 i 109 889 i 358 750 + 363 724 f 92 903 of- 62 837 + J8 775 + 94 5241 + 418 16217 + 510 24915 + 396 967 + 102 672 f 50 334+ 6 I81 + 21 168+ 9-8 208 f 8 224 + 6 191 + 16 119+ 109 22s+ 17 1’67 f I87 8570 + 596 15395 * 1831 1x2+ lh 15x+ II 214+ 16 cpm. counts per minute: SEM. standard error of the mean. Strains: a\ in Fig. I of S. G. Linn et al. / FEMS Immunology and Medical Micmbiologv I3 f 1996) 81-86 84 Table 2 Induction of TNFa, IL-lb and IL-6 expression incubation with killed S. epidermidis Medium 199 S. epidemidis 354 S. epidemidis N900057 S. epidemidis N870094 1x104 1 x 105 IX lob IX 107 IX 101 IX 105 1 x IOh I x 10’ 1XlOl 1 x 105 IX IO6 IX IO’ by PBMC TNF IL- I IL-6 < < 0.2 2.3 4.8 10.7 15.6 2.0 3.6 7.1 15.7 2.3 4.0 7.7 15.0 0.3 16.3 26.1 34.3 36.7 19.8 25.4 32.0 36.8 23.0 7.0 31.2 36.2 0.2 8.2 8.2 13.2 15.7 7.6 8.5 13.3 18.3 5.6 13.6 12.7 13.6 on Data are expressed in ng ml-’ as determined by enzyme immunoassay. Strains as in Fig. 1; S. epidermidis 354 is a reference strain. Superantigen expression leads to proliferation of human peripheral blood monocytes or of rabbit splenocytes. When tested in these systems the S. epidemidis supematants, at any concentration, caused no mitogenic response in the cells over controls. S. atireus FRIS6, as expected, produced a vigourous proliferative response, while S. aureus RN450 which does not produce superantigen, was inactive (Table 1). We conclude that strains N900057 and N860094 of S. epidermidis do not produce superantigens or mitogenic exotoxins. Possible induction of cytokine expression in monocytes by components of the bacterial cell wall was therefore investigated by incubating human monocytes with suspensions of killed washed S. epidermidis. Table 2 shows that both TSS associated strains and a control strain (354) of S. epidermidis induce a dose-dependent release of TNFcu, IL- 1p and IL-6 into the supematant by human monocytes. Very similar levels of release of each cytokine was observed on stimulation by the same concentration of all three strains tested. 4. Discussion The mechanisms by which S. epidennidis causes shock are at present unclear. It has been suggested that it might produce a superantigenic toxin, and indeed it does secrete exoproteins and toxins such as S-haemolysin, cytotoxins and Dnase which resemble their counterparts from S. aureus [ 15,161. Enterotoxin-producing isolates of S. epidermidis have been reported from animal samples [ 171, and an initial study of 7 human cases of CNS-related TSS suggested that only TSST- l-producing strains were involved [lS]. Later studies have, however, shown that these strains neither produce TSST-1 toxin nor possess the homologous genes [ 19,201. The S. epidermidis strains N900057 and N870094 were initially thought to have caused TSS in the patients from which they were isolated through an exoprotein because their DNAs appeared to hybridise with oligoprobes specific for the S. aureu,s seh and set genes. However, immunological assays detected no SEB or SEC in the culture supematants, suggesting antigenic variation [ 101. We have re-examined the possible presence of seb or set DNA in these strains by PCR, and find no signal even under relaxed conditions. We therefore conclude that the previous results obtained using oligoprobes were false positives due to inadequate specificity of the method, although dot-blot hybridisation has been widely used for the detection of bacterial genes. including those for TSST- 1 and enterotoxins [ 10,11,2 11. It remained possible that our S. epidermidis isolates produced an unrelated superantigenic exotoxin. so we tested supernatants of mature cultures for mitogenic activity on susceptible human and rabbit cells. No mitogenic activity was observed at any concentration, providing strong evidence that these strains do not secrete superantigenic toxins, or indeed any other mitogenic substance. An alternative mechanism for induction of TSS involves interaction between bacterial cell wall components and monocytes. leading to the release of cytokine mediators. Gram-negative bacteria such as E. coli induce shock through LPS in their outer membrane. and S. epidermidis can cause apparently identical experimental shock in rabbits [5]. In both cases the percentage of animals suffering shock was similar, and symptoms were accompanied by TNFQ and IL- 1p release. Recently peptidoglycans, teichoic acid and lipoteichoic acid from S. epidermidis cell walls have been shown to induce cytokine production in human monocytes [6,14.22]. We show here G. Lina et al. / FEMS Irnmur~olog~ and Medical that whole killed S. epidermidis is a powerful inducer of TNFcu, IL- 1j3 and IL-6 expression in human adherent monocytes. It might be questioned whether cytokine release in the absence of superantigen stimulation of T cells can provide a sufficient stimulus for TSS. It has been shown that immunisation against TNFQ protects animals from SEB-induced TSS, and that TNFa and IL-I /3 are major mediators of shock [7,8,23]. In addition, superantigen-induced TSS requires the presence of T cells, since nude mice are not susceptible, but T cell proliferation is not required, since cyclosporin treatment does not protect [24,25]. Release of cytokines. especially TNFcr and IL-I p. either through cell wall interactions with monocytes or through superantigen stimulation of T cells, thus appears to be a crucial element in the induction of TSS. It may be noted that S. e,uidernzidis strain 354 which was derived from a catheter-related bacteremia without known TSS, was as efficient an inducer of cytokine release as the two TSS-related strains. The incidence of TSS in human patients and in experimental animals is generally less than half of the potential cases. Although the capacity to induce excessive cytokine release appears necessary for the induction of TSS by a bacterium, other factors must intervene in the progression to clinical shock. S. epidermidis cell wall components appear to be a sufficiently powerful stimulus to cytokine release from monocytes to explain clinical TSS associated with this bacterium. Acknowledgements We are grateful to P. Schlievert for scientific advice. and B. Jaulhac and S. Foumier for their technical cooperation and assistance. References [I] Herwaldt. L.A. ( 1988) Coagulase-negative staphylococci: important nosocomial pathogens. Curr. Opin. Infect. Dis. 1. 755-763. [2] Fidalgo. S., Vazquez, F.. Mendoza. M.C., Perez. F. and MCndez, F.J. ( 1990) Bacteremia due to Sfaph~lococc~ts rpi- Microhiologx 13 f IYY61 81-86 85 microbiologic. epidemiologic, clinical and prognostic features. Rev. Infect. Dis. 12, 520-528. [3] Martin, M.A.. Pfaller. M.A. and Wenzel. R.P. (1989) Coagulase-negative staphylococcal bacteremia. Mortality and hospital stay. Ann. Intern. Med. 110. 9-16. [J] Freudenberg, M.A. and Galanos, C. (1990) Bacterial lipopolysaccharides: structure, metabolism and action. lnt. Rev. Immunol. 6. 207-22 I. [5] Wakabayashi. G., Gelfand. J.A., Jung. W.K., Connolly, R.J.. Burke. J.F. and Dinarello. C.A. (1991) Srupb~lococcus epidermidis induces complement activation, tumor necrosis factor and interleukin-1, a shock-like state and tissue injury in rabbits without endotoxemia. Comparison to E.scherkhia w/i. J. Clin. Invest. 87, 1925-1935. 161Timmerman. C.P.. Mattsson, E.. Martinez-Martinez. L.. De Graaf. L.. Van Strijp. J.A.G., Verbrugh. H.A., Verhoef, J. and Fleer. A. (1993) Induction of release of tumor necrosis factor from human monocytes by staphylococci and staphylococcal peptidoglycans. Infect, Immun. 61. 4167-4172. [71 Parsonnet. J., Hickman, R.K., Eardley. D.D. and Pier, G.B. (1985) Induction of human interleukin-I by toxic shock syndrome toxin-l. J. Infect. Dis. 151. 514-522. [81 Fast. D.J.. Schlievert. P.M. and Nelson. R.D. (1989) Toxic shock syndrome-associated staphylococcal and atreptococcal pyrogenic toxins are potent inducers of tumor necrosis factor production. Infect. Immun. 57. 291-294. 191 CDC (1980) Follow-up on toxic-shock syndrome. MMWR 29. 441-1-15. 1101 Jaulhac. B.. Bes. M., Bornstein. N., Piemont, Y.. Brun, Y. and Fleurette. J. (19921 Synthetic DNA probes for detection of genes for enterotoxins A. B. C. D, E and TSST-I in staphylococcal strains. J. Appl. Microbial. 72, 386-392. II II Ausubel. F.M.. Brent. R.. Kingston, R.E.. Moore. B.D.. Seidman, J.G., Smith. J.A. and Struhl. K. (1987) Analysis of DNA sequences by blotting and hybridization. In: Current Protocols in Molecular Biology (Janssen. K.. Ed.). Greene Publishing Associates and Wiley-Interscience, New York. [I21 Wilson. I.G.. Cooper. J.E. and Gilmour. A. ( 1991) Detection of enterotoxingenic Srapltvlococcrrs LIII~~USm dried skimmed milk: use of the polymerase chain reaction for amplification and detection of staphylococcal enterotoxin genes entE and enrCI and the thermonuclease gene nn~‘. Appl. Environ, Microbial. 57. 1793-798. [I31 Johnson. W.M., Tyler. SD.. Ewan. E.P.. Ashton. F.E., Pollard, D.R. and Rozee. K.R. (1991) Detection of genes for enterotoxins. exfoliative toxins and toxic shock syndrome toxin 1 in Srtrph&~oc~cus nnrens by the polymerase chain reaction. J. Clin. Microbioi. 29. 426-30. [IdI Mattsson. E.. Verhage, L.. Rollof. J.. Fleer. A.. Verhoef. J. and van Dijk. H. (1993) Peptidoglycan and teichoic acid from Stc~ph~loco~ws rpidennidis stimulate human monocytes to release tumour necrosis factor-a. interleukin-I p and interleukin-6. FEMS Immunol. Med. Microbial. 7. 28 I-288. of coagulase-negative [I51 Gemmell. C.G. (1987) Exo-proteins staphylococci as possible virulence factors. Zentralbl. Bakteriol. A 266, 93- 102. iI61 McKevitt. A.I., Bjornson. G.L., Mauracher. C.A. and dermidis: 86 [17] [18] [ 191 [20] [21] G. Lina et al. / FEM.7 Immunolog_v and Medical Microbiology Scheifele, D.W. (1990) Amino acid sequence of a deltalike toxin from Staph$ococcus epidermidis. Infect. Immun. 58. 1473-1475. Marin, M.E., Del Carmen de la Rosa, M. and Comejo. I. (1992) Enterotoxigenicity of staphylococcus strains isolated from Spanish dry-cured hams. Appl. Environ, Microbial. 58. 1067- 1069. Crass, B.A. and Bergdoll. M.S. (1986) Involvement of coagulase-negative staphylococci in toxic shock syndrome. J. Clin. Microbial. 23, 43-45. Parsonnet, J., Harrison, A.E., Spencer, S.E., Reading, A.. Parsonnet, KC. and Kass, E.H. (1987) Nonproduction of toxic shock syndrome toxin 1 by coagulase-negative staphylococci. J. Clin. Microbial. 25. 1370-1372. Kreiswirth, B.N., Schlievert, P.M. and Novick. R.P. (19871 Evaluation of coagulase-negative staphylococci for ability to produce toxic shock syndrome toxin 1. J. Clin. Microbial. 25, 2028-2029. Neill, R.J., Fanning, G.R.. Delahoz, F., Wolff, R. and Gem- [22] [23] [24] [25] 13 (19%) 81-86 ski, P. (1990) Oligonucleotide probes for detection and differentiation of Staph$ococcus aurerts strains containing genes for enterotoxins A, B and C and toxic shock syndrome toxin]. J. Clin. Microbial. 28, 1514-518. Heumann, D., Barras, C.. Severin, A., Glauser. M.P. and Tomasz. A. (1994) Gram-positive cell walls stimulate synthesis of Tumor Necrosis Factor alpha and Interleukin-6 by Human Monocytes. Infect. Immun. 62, 2715-2721. Miethke, T.. Gaus, H., Wahl, C., Heeg. K. and Wagner. H. (1992) T-cell-dependent shock induced by a bacterial superantigen. Chem. Immunol. 55, 172-184. Marrack. P., Blackman. M., Kushnir, E. and Kappler. J. (1990) The toxicity of staphylccoccal enterotoxin B in mice is mediated by T cells. J. Exp. Med. 171, 455-464. Lee, P.K., Deringer, J.R., Kreiswirth, B.N., Novick, R.P. and Schlievert. P.M. (1991) Fluid remplacement protection of rabbits challenged subcutaneously with toxic shock syndrome toxins. Infect. Immun. 59, 879-884.