* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download September 2006 - Highmark Blue Shield
Psychedelic therapy wikipedia , lookup
Drug design wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Compounding wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug discovery wikipedia , lookup
Electronic prescribing wikipedia , lookup
Pharmacogenomics wikipedia , lookup
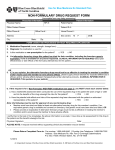
December 2007 ________________________________________________ 4th Quarter Update: Highmark Drug Formulary Enclosed is the 4th Quarter 2007 update to the Highmark Drug Formulary and pharmaceutical management procedures. The Formulary and pharmaceutical management procedures are updated on a quarterly basis, and the enclosed changes reflect the decisions made in September 2007 by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. As an added convenience, you can also search the Highmark Drug Formulary online at http://highmark.formularies.com. This function allows you to search by the drug name or therapeutic class. You can also find other helpful information regarding the prescription drug program from our online Resource Center under the Pharmacy/Formulary Information link. (NaviNet® users: Simply click on the Resource Center button for quick access to the Pharmacy/Formulary Information link.) Formulary changes will be reflective of both the Highmark Select/Choice Formulary (formerly the Highmark Closed/Incentive Formulary) and the Highmark Medicare-Approved Select/Choice Formulary. For each section, please refer to the header description to obtain information specific to that formulary. Section I contains changes to the Highmark Select/Choice Formulary. Section II contains changes to the Highmark Medicare-Approved Select/Choice Formulary. The Highmark Medicare-Approved Select/Choice Formulary can also be searched online at http://highmark.medicare-approvedformularies.com. If you have any questions, contact Provider Service or call Pharmacy Affairs, toll-free, at 1-800-600-2227. (over, please) Highmark Drug Formulary Update December 2007 Section I. Highmark Select/Choice Formulary (Formerly Closed/Incentive Formulary) A. Changes to the Highmark Select/Choice Formulary The Highmark Pharmacy and Therapeutics Committee has reviewed the medications listed in the following tables. Please note that since the Highmark Select/Choice Formulary is a complete subset of the Open Formulary, all medications added to the Select/Choice Formulary are automatically added to the Open Formulary. For your convenience, you can search the Highmark Select/Choice Formulary online at http://highmark.formularies.com. An electronic copy of the Highmark Select/Choice Formulary for use with a portable handheld device can be downloaded free by visiting www.epocrates.com. Table 1: Products Added (All products added to the formulary effective immediately unless otherwise noted) Brand Name Generic Name Comments ® AndroGel § testosterone 1% gel A topically applied testosterone product for the treatment of hypogonadism Exelon® Patch rivastigmine transdermal An acetylcholinesterase inhibitor indicated for the system treatment of mild to moderate Alzheimer’s dementia and mild to moderate dementia associated with Parkinson’s disease Exforge® amlodipine/valsartan A calcium channel blocker/angiotensin receptor blocker combination for the treatment of hypertension FreeStyle Lite blood glucose test strip Multiple other blood glucose test strips are also on the formulary. Humatrope®§ somatropin Norditropin® is also on the formulary. ™ Janumet sitagliptin/metformin A dipeptidyl peptidase-4 (DPP-4) inhibitor/metformin combination for the treatment of type II diabetes mellitus Januvia™ sitagliptin A dipeptidyl peptidase-4 (DPP-4) inhibitor for the treatment of type II diabetes mellitus Letairis™ ambrisentan An endothelin receptor antagonist (ERA) indicated for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1) in patients with WHO Class II or III symptoms to improve exercise capacity and delay clinical worsening §Effective Jan. 1, 2008 Table 2: Products Not Added* Brand Name Generic Name Chantix™ varenicline Divigel® estradiol gel Enablex® darifenacin extended release tablets Comments Bupropion and bupropion SR are on the formulary. Climara®, Estraderm® and Vivelle-Dot® are on the formulary. Detrol®, Detrol® LA, oxybutynin and oxybutynin ER are on the formulary. *Physicians may request coverage of these products using the Prescription Drug Medication Request Form, which can be found on Page 8 of the 2008 Highmark Drug Formulary book. You may also access the form online in Highmark’s Provider Resource Center, under Provider Forms; select Miscellaneous Forms from the fly-out menu. (continued) 2 A. Changes to the Highmark Select/Choice Formulary (continued) Table 2: Products Not Added* (continued) Brand Name Generic Name Comments Endometrin® progesterone vaginal insert Crinone® is on the formulary. Extina® ketoconazole foam Topical forms of ketoconazole are on the formulary. ® Lybrel levonorgestrel/ethynyl Multiple oral contraceptives are on the formulary. estradiol Neupro® rotigotine transdermal system Selegiline, carbidopa-levodopa, Comtan®, Mirapex® and Requip® are on the formulary. ® VesiCare solifenacin succinate Detrol®, Detrol® LA, oxybutynin and oxybutynin ER are on the formulary. Xyzal® levocetirizine Fexofenadine is on the formulary. Zyflo CR ™ zileuton extended release Accolate® and Singulair® are on the formulary. *Physicians may request coverage of these products using the Prescription Drug Medication Request Form, which can be found on Page 8 of the 2008 Highmark Drug Formulary book. You may also access the form online in Highmark’s Provider Resource Center, under Provider Forms; select Miscellaneous Forms from the fly-out menu. Table 3: Products to be Removed* from the Formulary (effective Jan. 1, 2008, unless otherwise noted) Brand Name Comments Generic Name MetroGel® 1%¶ metronidazole Generic metronidazole gel is on the formulary. Testim® testosterone 1% gel Xalatan® latanoprost Genotropin® somatropin somatropin Multiple testosterone products are on the formulary. Travatan®, Travatan® Z™ and Lumigan® are on the formulary. Humatrope® and Norditropin® are on the formulary. Humatrope and Norditropin are on the formulary. Nutropin AQ somatropin Humatrope and Norditropin are on the formulary. Nutropin Depot® somatropin Humatrope and Norditropin are on the formulary. Protropin® somatrem Humatrope and Norditropin are on the formulary. Serostim® somatropin Humatrope and Norditropin are on the formulary. Tev-Tropin® somatropin Humatrope and Norditropin are on the formulary. Nutropin® ® *Physicians may request coverage of these products using the Prescription Drug Medication Request Form, which can be found on Page 8 of the 2008 Highmark Drug Formulary book. You may also access the form online in Highmark’s Provider Resource Center, under Provider Forms; select Miscellaneous Forms from the fly-out menu. ¶Effective July 1, 2008 B. Updates to the Prior Authorization Program 1. Letairis™ (ambrisentan) Effective Nov. 1, 2007, Letairis was added to Highmark’s pulmonary arterial hypertension prior authorization policy. Letairis is an endothelin receptor antagonist indicated for the treatment of pulmonary arterial hypertension (WHO Group 1) in patients with WHO Class II or III symptoms to improve exercise capacity and delay clinical worsening. (continued) 3 B. Updates to the Prior Authorization Program (continued) 1. Letairis™ (ambrisentan) (continued) When a benefit, ambrisentan may be approved when all of the following criteria are met: • A diagnosis of pulmonary hypertension is substantiated by results from Doppler echocardiography and/or direct measurement of pulmonary arterial pressure (Pulmonary arterial hypertension is defined as a mean pulmonary arterial pressure of > or = 25 mmHg, with a pulmonary capillary wedge pressure of <15 mmHg), AND • Ambrisentan is prescribed under the supervision of a cardiologist or pulmonologist, AND • Ambrisentan is to be used for the treatment of pulmonary arterial hypertension (WHO Group I) in members with WHO functional Class II or III symptoms, AND • Ambrisentan may be used alone or in combination with calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, diuretics, digoxin and anticoagulants, but will not be covered when used concomitantly with bosentan (Tracleer™), sildenafil (Revatio™), epoprostenol sodium (Flolan®), treprostinil sodium (Remodulin™) or iloprost (Ventavis®), due to the lack of clinical data to support combination therapy with these agents. As there is no established criterion or algorithm for the transitioning of patients from one PAH drug product to another (e.g., sildenafil to bosentan), the use of two agents concomitantly may be authorized for a period of up to one month to accommodate potential overlapping titration schedules when changing therapy from one drug product to another. As stated above, coverage will not be provided for the use of two agents (bosentan, ambrisentan, sildenafil, epoprostenol, iloprost, treprostinil) as maintenance combination therapy for PAH. If approved, authorization may be granted for a period of up to one year. 2. Humira® (adalimumab) Effective Sept. 5, 2007, the prior authorization criteria for Humira was revised to allow for use as a first-line agent in the treatment of moderate to severe active rheumatoid arthritis. When a benefit, coverage for adalimumab may be approved if members meet the following criteria: • The member should be under the supervision of a rheumatologist or gastroenterologist, AND • The member is currently not using another biological DMARD [e.g., etanercept (Enbrel), anakinra (Kineret), etc.], AND • Adalimumab is to be used in reducing the signs and symptoms and inhibiting the progression of structural damage in adults with moderate to severe active rheumatoid arthritis, OR • Adalimumab is to be used in reducing the signs and symptoms of active arthritis in patients with psoriatic arthritis, OR • Adalimumab is to be used in reducing the signs and symptoms of patients with ankylosing spondylitis, OR • Adalimumab is to be used in reducing the signs and symptoms of patients with Crohn’s Disease who have failed two alternative therapies or monotherapy with Remicade. If approved, authorization may be granted for a period of up to one year. 3. Nexavar® (sorafenib) Effective Sept. 5, 2007, the prior authorization criteria for Nexavar was revised to include coverage when used for the treatment of hepatocellular carcinoma. These revisions were made in response to recent updates to the NCCN practice guidelines for hepatobiliary cancers. (continued) 4 B. Updates to the Prior Authorization Program (continued) 3. Nexavar® (sorafenib) (continued) When a benefit, sorafenib may be approved when all of the following criteria are met: • Sorafenib is to be prescribed under the supervision of an oncologist/hematologist. • Sorafenib is to be used for the treatment of advanced renal cell carcinoma after treatment with at least one other prior systemic therapy, OR • Sorafenib is to be used for the treatment of hepatocellular carcinoma. Use of sorafenib for disease states outside of these indications should be denied based on the lack of clinical data to support its effectiveness and safety in other conditions. If approved, authorization may be granted for a period of up to one year. C. Updates to the Managed Prescription Drug Coverage (MRxC) Program 1. Lyrica™ (pregabalin) Effective Sept. 5, 2007, the Managed Prescription Drug Coverage (MRxC) policy for Lyrica was revised to allow for coverage when used for the treatment of fibromyalgia. When a benefit, coverage for pregabalin for the treatment of fibromyalgia may be approved if members meet the following criteria: • The member has a documented diagnosis of fibromyalgia as determined by clinical notes including, but not limited to, confirmation of widespread bilateral pain both above and below the waist for >3 months duration AND the presence of at least 11 of 18 specific tender points AND documented fibromyalgia-related symptoms (e.g., fatigue, sleep disturbance, neurologic symptoms and/or exercise intolerance), AND • The member has a documented trial and failure of at least two additional agents used to treat fibromyalgia (e.g., tricyclic agents, cyclobenzaprine, SSRIs), one of which must be a tricyclic agent or cyclobenzaprine. If approved, authorization may be granted for a period of up to one year. 2. Subutex® (buprenorphine) and Suboxone® (buprenorphine and naloxone) Effective Sept. 5, 2007, the Managed Prescription Drug Coverage (MRxC) policy for Subutex and Suboxone sublingual tablets was revised. Subutex and Suboxone are classified as Schedule III controlled substances and are indicated for the treatment of opioid dependence. Subutex is used as a single agent for the initial treatment (induction) of opioid dependence, and Suboxone is used following the initial phase of therapy. When a benefit, coverage for Subutex and Suboxone may be approved if members meet the following criteria: Subutex: Subutex may be covered for a five-day supply (160 mg) of medication within the last 90 days for the induction treatment of opioid dependence. Authorization for an additional coverage period can be approved for female members who are pregnant and require treatment for opioid dependence for the duration of their pregnancy (up to nine months of treatment, at which time the member can be transitioned to treatment with the combination tablet). Otherwise, Subutex will not be covered for long-term therapy. Suboxone: Suboxone may be approved if a member meets the following criteria: • The prescribed dose of Suboxone does not exceed 720mg/30 days (24mg/day). Members who meet the criteria as outlined above will receive automatic authorization at the level of the (continued) 5 C. Updates to the Managed Prescription Drug Coverage (MRxC) Program (continued) 2. Subutex® (buprenorphine) and Suboxone® (buprenorphine and naloxone) (continued) Suboxone: (continued) pharmacy without documentation of additional information. Claims will adjudicate automatically with no prior authorization required. For members who do not meet the criteria noted previously, the dispensing pharmacist will be prompted that prior authorization is required. Prior authorization criteria include the following: • The member is being treated for opioid dependence by a physician certified in addiction medicine, AND • The patient is enrolled in at least one ancillary service (e.g., psychiatric, counseling, behavioral education), AND • The prescribed dose of Suboxone does not exceed 24mg/day. Upon receiving authorization for payment of claims for Suboxone, claims for opioid-containing products will reject at the point of sale if the member has a claim for Subutex or Suboxone in their pharmacy claims history within the past 120 days. Authorization for coverage of an opioid claim will be provided if the member has a documented acute pain condition (e.g., acute traumatic injury) in which treatment with other agents would cause insufficient pain control, or if the member requires treatment for pain related to a terminal illness. If approved, authorization may be granted for a period of up to one year. D. Quantity Level Limit Additions Effective Sept. 5, 2007, the following products were added to Highmark’s Quantity Level Limit (QLL) program. Table 4: Additions to the QLL program Brand Name Generic Name Up to 34 Days’ Supply 35-90 Days’ Supply Limit (retail) Limit (retail or mail) Elestrin™ 144 gm estradiol 0.06% gel 1 metered pump 3 metered pumps E. Updates to Highmark’s Formulary policies 1. Direct Renin Inhibitors This policy pertains to the products categorized as direct renin inhibitors. Aliskeren (Tekturna®) is currently the only product available within this therapeutic category. Aliskeren is indicated for the treatment of hypertension. It may be used alone or in combination with other antihypertensive agents. Most exposure to date is with diuretics and an angiotensin receptor blocker (ARB), valsartan. Use with maximal doses of ACE inhibitors has not been adequately studied. Significant benefits over currently available products within the class of ACE inhibitors or ARBs are unclear. Effective Sept. 5, 2007, when a benefit, coverage for Aliskeren may be approved if members meet the following criteria: • The agent must be used for an FDA-approved indication. • The member must have tried (see third bullet) and failed at least two formulary agents within either or both of the following class of drugs: ACE inhibitor or angiotensin receptor blocker (ARB). • An “adequate therapeutic trial” consists of using an ACE inhibitor or ARB at recommended doses for at least a two-week period (unless the member experiences an intolerable side effect due to drug therapy within that time frame). “Drug therapy failure” consists of not achieving the desired therapeutic goal, development of an intolerable side effect due to drug therapy or development of hypersensitivity reaction to the drug product. The length of therapy with the formulary products and the reason for treatment failure should be documented. (continued) 6 E. 1. • • Updates to Highmark’s Formulary policies (continued) Direct Renin Inhibitors (continued) If failure of an agent was due to an adverse effect related to the ACE inhibitor or ARB class (e.g., head and neck angioedema), then the use of Aliskeren is a relative contraindication. A request will not be considered in this instance due to the risk to the member. A request based on the reasoning that “the member is currently stable and cannot be switched to another agent” will not be considered legitimate unless the member has tried and failed two formulary products (as listed previously). Section II. Highmark Medicare-Approved Select/Choice Formulary A. Changes to the Highmark Medicare-Approved Select/Choice Formulary The Highmark Pharmacy and Therapeutics Committee has reviewed the medications listed in the following tables. As a reminder, the Highmark Medicare-Approved Select/Choice Formulary applies only to Highmark Medicare Advantage and BlueRxSM members. For your convenience, you can search the Highmark Medicare-Approved Select/Choice Formulary online at http://highmark.medicare-approvedformularies.com. Table 1: Products Added (All products added to the formulary effective immediately unless otherwise noted) Brand Name Generic Name Comments ® Androgel § testosterone gel A topical testosterone product Azopt®§ brinzolamide A carbonic anhydrase inhibitor used to treat openangle glaucoma Exelon® Patch rivastigmine An acetylcholinesterase inhibitor indicated transdermal system for the treatment of mild to moderate Alzheimer’s dementia and mild to moderate dementia associated with Parkinson’s disease ® Exforge amlodipine/valsartan A calcium channel blocker/angiotensin receptor blocker combination for the treatment of hypertension Famvir®§ famciclovir An oral antiviral agent for the treatment of herpes zoster (shingles) and herpes simplex infections ™ Janumet sitagliptin/metformin A dipeptidyl peptidase-4 (DPP-4) inhibitor/metformin combination for the treatment of type II diabetes mellitus Januvia™ sitagliptin A dipeptidyl peptidase-4 (DPP-4) inhibitor for the treatment of type II diabetes mellitus ™ Letairis ¶ ambrisentan An endothelin receptor antagonist (ERA) indicated for the treatment of pulmonary arterial hypertension (PAH) (WHO Group 1) in patients with WHO Class II or III symptoms to improve exercise capacity and delay clinical worsening ® Lexapro § escitalopram oxalate A selective serotonin reuptake inhibitor (SSRI) for the treatment of depression and generalized anxiety disorder lidocaine/prilocaine§ lidocaine/prilocaine A local anesthetic combination for topical use Lovaza™§ omega-3-acid ethyl An adjunct to diet to reduce triglyceride (TG) levels in esters adult patients with very high (>500 mg/dL) triglyceride levels §Effective Jan. 1, 2008 ¶Effective March 1, 2008 7 A. Changes to the Highmark Medicare-Approved Select/Choice Formulary (continued) Table 2: Products Not Added* Brand Name Generic Name Comments Chantix™ varenicline Bupropion and bupropion SR are on the formulary. Divigel® estradiol gel Climara®, Estraderm® and Vivelle-Dot® are on the formulary. ® Endometrin progesterone vaginal insert Crinone® is on the formulary. Extina® ketoconazole foam Topical forms of ketoconazole are on the formulary. Lybrel® levonorgestrel/ethynyl Multiple oral contraceptives are on the formulary. estradiol ® Neupro rotigotine transdermal Selegiline, carbidopa-levodopa, Comtan®, Mirapex® system and Requip® are on the formulary. Xyzal® levocetirizine Fexofenadine is on the formulary. Zyflo CR ™ zileuton extended release Accolate® and Singulair® are on the formulary. Reclast® zoledronic acid An I.V. bisphosphonate for the treatment of osteoporosis Torisel™ temsirolimus Intravenous medication for the treatment of advanced renal cell carcinoma *Physicians may request coverage of these products using the Prescription Drug Medication Request Form, which can be found on Page 8 of the 2008 Highmark Drug Formulary book. You may also access the form online in Highmark’s Provider Resource Center, under Provider Forms; select Miscellaneous Forms from the fly-out menu. Table 3: Products Removed* From the Formulary (effective Jan. 1, 2008) Brand Name Generic Name Comments Aromasin® exemestane Femara® and Arimidex® are on the formulary. Carisoprodol carisoprodol Ciloxan® ciprofloxacin This medication has been identified as a drug to avoid in the elderly. Generic is on the formulary. etidronate disodium Generic is on the formulary. Effexor venlafaxine HCl Generic is on the formulary. Flonase® fluticasone propionate Generic is on the formulary. Floxin Ophthalmic ofloxacin Generic is on the formulary. Isopto Carbachol Isopto Carbachol This product is no longer available. Phenylephrine HCl/ Promethazine HCl Primaxin® Phenylephrine HCl/ Promethazine HCl Imipenem-Cilastatin Cough/cold preparations are not covered under Medicare Part D. Merrem® is on the formulary. Pseudoephedrine HCl/brompheniramine maleate Pseudoephedrine HCl/brompheniramine maleate capsule, sustained action Pseudoephedrine HCl/brompheniramine maleate Pseudoephedrine HCl/brompheniramine maleate capsule, sustained action Cough/cold preparations are not covered under Medicare Part D. Didronel ® ® ® Cough/cold preparations are not covered under Medicare Part D. *Physicians may request coverage of these products using the Prescription Drug Medication Request Form, which can be found on Page 8 of the 2008 Highmark Drug Formulary book. You may also access the form online in Highmark’s Provider Resource Center, under Provider Forms; select Miscellaneous Forms from the fly-out menu. (continued) 8 A. Changes to the Highmark Medicare-Approved Select/Choice Formulary (continued) Table 3: Products Removed* From the Formulary (effective Jan. 1, 2008) (continued) Brand Name Generic Name Comments Pseudoephedrine HCl/carbinoxamine malate tablet, sustained action Pseudoephedrine HCl/chlorpheniramine maleate capsule, sustained action Urocit-K® Zoloft ® Pseudoephedrine HCl/carbinoxamine malate tablet, sustained action Cough/cold preparations are not covered under Medicare Part D. Pseudoephedrine HCl/chlorpheniramine maleate capsule, sustained action potassium citrate Cough/cold preparations are not covered under Medicare Part D. sertraline HCl Generic is on the formulary. Generic is on the formulary. *Physicians may request coverage of these products using the Prescription Drug Medication Request Form, which can be found on Page 8 of the 2008 Highmark Drug Formulary book. You may also access the form online in Highmark’s Provider Resource Center, under Provider Forms; select Miscellaneous Forms from the fly-out menu. Table 4: Tiering Changes Beginning in 2008, Medicare Advantage and BlueRxSM members will have a Medicare-Approved Choice (Incentive) Formulary design. For these members, the medications listed in the table below will be covered as Non-Preferred Brands (Tier 3). For members with a Medicare-Approved Select (Closed) Formulary, the products in this table are covered as Preferred Brands (Tier 2). Therapeutic Chapter Brand Name Generic Name Autonomic & CNS Drugs, Neurology, & Psych Antivertigo & antiemetic drugs Emend1 Aprepitant Antiparkisonism agents Comtan Entacapone Anticonvulsants Lyrica1 Pregabalin Miscellaneous antidepressants Cymbalta1 Duloxetine Effexor XR Venlafaxine HCL Aripiprazole Miscellaneous antipsychotics Abilify Aripiprazole ODT Abilify Disc-melt Paliperidone Invega Olanzapine Zyprexa Olanzapine Zyprexa Zydis Cardiovascular, Hypertension & Lipids Coagulation therapy Aggrenox Aspirin/dipyridamole Lipid/cholesterol-lowering agents Omacor Omega-3 acid ethyl esters Immunology, Vaccines & Biotechnology Interferons Betaseron1 Interferon beta-1b Musculoskeletal & Rheumatology Osteoporosis therapy Boniva IV only Ibandronate Respiratory, Allergy, Cough & Cold Miscellaneous pulmonary agents Zyflo Zileuton 1. Authorization Required B. Updates to the Prior Authorization Program 1. Letairis™ (ambrisentan) Effective March 1, 2008, Letairis will be added to Highmark’s pulmonary arterial hypertension prior authorization policy for Medicare Advantage and BlueRx members. Letairis is an endothelin receptor (continued) 9 B. Updates to the Prior Authorization Program (continued) 1. Letairis™ (ambrisentan) (continued) antagonist indicated for the treatment of pulmonary arterial hypertension (WHO Group 1) in patients with WHO Class II or III symptoms to improve exercise capacity and delay clinical worsening. When a benefit, ambrisentan may be approved when all of the following criteria are met: • A diagnosis of pulmonary hypertension is substantiated by results from Doppler echocardiography and/or direct measurement of pulmonary arterial pressure (Pulmonary arterial hypertension is defined as a mean pulmonary arterial pressure of > or = 25 mmHg, with a pulmonary capillary wedge pressure of <15 mmHg), AND • Ambrisentan is prescribed under the supervision of a cardiologist or pulmonologist, AND • Ambrisentan is to be used for the treatment of pulmonary arterial hypertension (WHO Group I) in members with WHO functional Class II or III symptoms, AND • Ambrisentan may be used alone or in combination with calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, diuretics, digoxin and anticoagulants, but will not be covered when used concomitantly with bosentan (Tracleer™), sildenafil (Revatio™), epoprostenol sodium (Flolan®), treprostinil sodium (Remodulin™) or iloprost (Ventavis®), due to the lack of clinical data to support combination therapy with these agents. The pulmonary arterial hypertension prior authorization policy has also been revised to allow for short-term combination therapy for PAH. As there is no established criterion or algorithm for the transitioning of patients from one PAH drug product to another (e.g., sildenafil to bosentan), the use of two agents concomitantly may be authorized for a period of up to one month to accommodate potential overlapping titration schedules when changing therapy from one drug product to another. As stated above, coverage will not be provided for the use of two agents (bosentan, ambrisentan, sildenafil, epoprostenol, iloprost, treprostinil) as maintenance combination therapy for PAH. If approved, authorization may be granted for a period of up to one year. 2. Humira® (adalimumab) Effective Sept. 5, 2007, the prior authorization criteria for Humira was revised for Medicare Advantage and BlueRxSM members to allow for use as a first-line agent in the treatment of moderate to severe active rheumatoid arthritis. When a benefit, coverage for adalimumab may be approved if members meet the following criteria: • The member should be under the supervision of a rheumatologist or gastroenterologist, AND • The member is currently not using another biological DMARD [e.g., etanercept (Enbrel), anakinra (Kineret), etc.], AND • Adalimumab is to be used in reducing the signs and symptoms and inhibiting the progression of structural damage in adults with moderate to severe active rheumatoid arthritis, OR • Adalimumab is to be used in reducing the signs and symptoms of active arthritis in patients with psoriatic arthritis, OR • Adalimumab is to be used in reducing the signs and symptoms of patients with ankylosing spondylitis, OR • Adalimumab is to be used in reducing the signs and symptoms of patients with Crohn’s Disease who have failed two alternative therapies or monotherapy with Remicade. If approved, authorization may be granted for a period of up to one year. 10 B. Updates to the Prior Authorization Program (continued) 3. Nexavar® (sorafenib) Effective Sept. 5, 2007, the prior authorization criteria for Nexavar was revised for Medicare Advantage and BlueRxSM members to include coverage when used for the treatment of hepatocellular carcinoma. These revisions were made in response to recent updates to the NCCN practice guidelines for hepatobiliary cancers. When a benefit, sorafenib may be approved when all of the following criteria are met: • Sorafenib is to be prescribed under the supervision of an oncologist/hematologist. • Sorafenib is to be used for the treatment of advanced renal cell carcinoma after treatment with at least one other prior systemic therapy, OR • Sorafenib is to be used for the treatment of hepatocellular carcinoma. Use of sorafenib for disease states outside of these indications should be denied based on the lack of clinical data to support its effectiveness and safety in other conditions. If approved, authorization may be granted for a period of up to one year. C. Updates to the Managed Prescription Drug Coverage (MRxC) Program 1. Lyrica™ (pregabalin) Effective Sept. 5, 2007, the Managed Prescription Drug Coverage (MRxC) policy for Lyrica was revised for Medicare Advantage and BlueRx members to allow for coverage when used for the treatment of fibromyalgia. When a benefit, coverage for pregabalin for the treatment of fibromyalgia may be approved if members meet the following criteria: • The member has a documented diagnosis of fibromyalgia as determined by clinical notes including, but not limited to, confirmation of widespread bilateral pain both above and below the waist for >3 months duration AND the presence of at least 11 of 18 specific tender points AND documented fibromyalgia-related symptoms (e.g., fatigue, sleep disturbance, neurologic symptoms and/or exercise intolerance), AND • The member has a documented trial and failure of at least two additional agents used to treat fibromyalgia (e.g., tricyclic agents, cyclobenzaprine, SSRIs), one of which must be a tricyclic agent or cyclobenzaprine. If approved, authorization may be granted for a period of up to one year. 2. Subutex® (buprenorphine) and Suboxone® (buprenorphine and naloxone) Effective Sept. 5, 2007, the Managed Prescription Drug Coverage (MRxC) policy for Subutex and Suboxone sublingual tablets was revised for Medicare Advantage and BlueRx members. Subutex and Suboxone are classified as Schedule III controlled substances and are indicated for the treatment of opioid dependence. Subutex is used as a single agent for the initial treatment (induction) of opioid dependence, and Suboxone is used following the initial phase of therapy. When a benefit, coverage for Subutex and Suboxone may be approved if members meet the following criteria: Subutex: Subutex may be covered for a five-day supply (160 mg) of medication within the last 90 days for the induction treatment of opioid dependence. Authorization for an additional coverage period can be approved for female members who are pregnant and require treatment for opioid dependence for the duration of their pregnancy (up to nine months of treatment, at which time the member can be transitioned to treatment with the combination tablet). Otherwise, Subutex will not be covered for long-term therapy. (continued) 11 C. Updates to the Managed Prescription Drug Coverage (MRxC) Program (continued) 2. Subutex® (buprenorphine) and Suboxone® (buprenorphine and naloxone) (continued) Suboxone: Suboxone may be approved if a member meets the following criteria: • The prescribed dose of Suboxone does not exceed 720mg/30 days (24mg/day). Members who meet the criteria as outlined above will receive automatic authorization at the level of the pharmacy without documentation of additional information. Claims will adjudicate automatically with no prior authorization required. For members who do not meet the criteria above, the dispensing pharmacist will be prompted that prior authorization is required. Prior authorization criteria include the following: • The member is being treated for opioid dependence by a physician certified in addiction medicine, AND • The patient is enrolled in at least one ancillary service (e.g., psychiatric, counseling, behavioral education), AND • The prescribed dose of Suboxone does not exceed 24mg/day. Upon receiving authorization for payment of claims for Suboxone, claims for opioid-containing products will reject at the point of sale if the member has a claim for Subutex or Suboxone in their pharmacy claims history within the past 120 days. Authorization for coverage of an opioid claim will be provided if the member has a documented acute pain condition (e.g., acute traumatic injury) in which treatment with other agents would cause insufficient pain control or if the member requires treatment for pain related to a terminal illness. If approved, authorization may be granted for a period of up to one year. D. Updates to Highmark’s Formulary policies 1. Direct Renin Inhibitors This policy pertains to the products categorized as direct renin inhibitors. Aliskeren (Tekturna®) is currently the only product available within this therapeutic category. Aliskeren is indicated for the treatment of hypertension. It may be used alone or in combination with other antihypertensive agents. Most exposure to date is with diuretics and an angiotensin receptor blocker (ARB), valsartan. Use with maximal doses of ACE inhibitors has not been adequately studied. Significant benefits over currently available products within the class of ACE inhibitors or ARBs are unclear. Effective Sept. 5, 2007, when a benefit, coverage for Aliskeren may be approved for Medicare Advantage and BlueRxSM members if the following criteria are met: • The agent must be used for an FDA-approved indication. • The member must have tried (see third bullet) and failed at least two formulary agents within either or both of the following class of drugs: ACE inhibitor or angiotensin receptor blocker (ARB). • An “adequate therapeutic trial” consists of using an ACE inhibitor or ARB at recommended doses for at least a two-week period (unless the member experiences an intolerable side effect due to drug therapy within that time frame). “Drug therapy failure” consists of not achieving the desired therapeutic goal, development of an intolerable side effect due to drug therapy or development of hypersensitivity reaction to the drug product. The length of therapy with the formulary products and the reason for treatment failure should be documented. • If failure of an agent was due to an adverse effect related to the ACE inhibitor or ARB class (e.g., head and neck angioedema), then the use of Aliskeren is a relative contraindication. A request will not be considered in this instance due to the risk to the member. • A request based on the reasoning that “the member is currently stable and cannot be switched to another agent” will not be considered legitimate unless the member has tried and failed two formulary products (as listed above). 2. Tiering Exceptions This policy applies to all Medicare Part D members who have a prescription drug benefit design with three or more tiers. Effective Sept. 5, 2007, the provider must document an adequate trial and/or failure of the (continued) 12 D. Updates to Highmark’s Formulary policies (continued) 2. Tiering Exceptions (continued) majority of the preferred medications before a tiering exception would be granted to non-preferred medications in the same drug class/category. When a benefit, a tiering exception may be approved if the following criteria are met: • If the tiering exception request is for a non-preferred, multi-source brand product and the generic is available on preferred, approval will be granted if: -- The member had an adequate trial and/or failed the generic medication plus two other available preferred medications within the same therapeutic class/category, OR -- The member had an adequate trial and/or failed the generic and each available preferred medication if a given therapeutic class/category has less than three available preferred medications. • If the tiering exception request is for a non-preferred, single-source brand product, approval will be granted if: -- The member had an adequate trial and/or failed three preferred medications within the same therapeutic class/category, OR -- The member had an adequate trial and/or failed each available preferred medication if a given therapeutic class/category has less than three available preferred medications. • Approvals will not be granted for a tiering exception request for a preferred, single-source brand product. • No tiering exception will be made for those drugs placed on the specialty tier. • A request based on the reasoning that “the patient is currently stable and cannot be switched to another agent” will not be considered legitimate unless the patient has tried and failed the required number of preferred products (see first and second bullets, above). • If a specific policy for a medication or therapeutic category/indication is established, then the medication or therapeutic category/indication policy would supersede the tiering exception policy. • No exceptions will be made for requests of non-preferred combination products that are currently available as separate preferred agents. E. 1. Updates to Recent Formulary Changes In the 1st Quarter 2007 Formulary Update, Noroxin® was listed as a medication to be removed from the formulary. Noroxin will remain on the Highmark Medicare-Approved Select/Choice Formulary. 2. In the 1st Quarter 2007 Formulary Update, Levaquin® was listed as a medication to be added to the formulary (effective May 1, 2007). Levaquin will not be added to the Highmark Medicare-Approved Select/Choice Formulary. 3. In the 3rd Quarter 2007 Formulary Update, Je-Vax® and Imovax® were listed as medications to be added to the formulary, effective June 2007. Je-Vax and Imovax will be added to the Highmark Medicare-Approved Select/Choice Formulary effective Jan. 1, 2008. F. Specialty Drug Tier Program Specialty drugs are very high-cost and unique drugs as defined by the Centers for Medicare and Medicaid Services. These drugs may incur a coinsurance based on their negotiated price. Because of this, the cost may vary slightly due to pricing changes in the drug. Drugs in the specialty tier apply to Highmark Medicare Advantage, BlueRxSM and Highmark Health Insurance Company members. Please refer to the following list for products included in the Specialty Drug Tier program. (continued) 13 F. Specialty Drug Tier Program (continued) Table 5: Products Included in the Specialty Drug Tier Program Product Name Accutane Humira Regranex Actimmune Humira Pen Remicade Actiq Immune Globulin Revlimid Adagen Increlex Ribapak Aldurazyme Infergen Ribasphere Alferon N Innohep Ribatab Anadrol-50 Intron A Ribavirin Apokyn Invirase Rilutek Aptivus Iressa Risperdal Consta Aralast Iveegam En Rituxan Aranesp Kaletra Roferon-A Aranesp Albumin Free Kineret Saizen Aredia Kytril Sandostatin Arixtra Leukine Sandostatin LAR Atripla Leuprolide Acetate Sensipar Avonex Lovenox Serostim Avonex Administration Pack Lupron Somavert Baraclude Lupron Depot Soriatane Betaseron Lupron Depot-Ped Sprycel Buphenyl Matulane Sucraid Carimune Mepron Sutent Carimune Nf Nanofiltered Mesnex Synarel Cerezyme Myozyme Tarceva Colistimethate Sodium Naglazyme Targretin Coly-Mycin M Parenteral Neulasta Tev-Tropin Copaxone Neumega Thalomid Copegus Neupogen Tracleer Cubicin Nexavar Truvada Cytovene Nimotop Tygacil D.H.E. 45 Norditropin Valcyte Declomycin Norditropin Nordiflex Vancocin Elaprase Novantrone Velcade Elitek Nutropin Venoglobulin-S 14 Section III. Miscellaneous Updates A. Zyrtec® to be Available Over the Counter Within the next few months, all forms of the prescription, non-sedating antihistamine Zyrtec will become available over the counter. This change will apply to Zyrtec tablets, Zyrtec chewable tablets, Zyrtec syrup and Zyrtec-D 12 Hour® extended-release tablets. The exact date of the prescription to over-the-counter switch has not yet been announced by the manufacturer. However, it will most likely occur in January 2008, shortly after the prescription patent expiration date of Dec. 25, 2007. B. Correction The relative cost of Humatrope® is incorrectly listed as $2,000-$2,500 on page 72 of the 2008 Highmark Drug Formulary book. The correct relative cost of this product is $1,000-$1,500. Highmark is a registered mark of Highmark Inc. BlueRx is a service mark of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans. Highmark Senior Resources Inc., a subsidiary of Highmark Inc., has a contract with the Federal government to administer Medicare Prescription Drug Coverage in the states of Pennsylvania and West Virginia. NaviNet is a registered trademark of NaviMedix, Inc. NaviMedix, Inc. is an independent company that does not provide Highmark Blue Shield products or services. NaviMedix, Inc. is solely responsible for the products and services that it provides and that are referenced in this bulletin. 15