* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Colloids
Drug interaction wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Non-specific effect of vaccines wikipedia , lookup
Intravenous therapy wikipedia , lookup
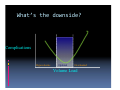
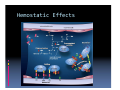
Duane J. Funk MD FRCP(C) What this talk will hopefully accomplish • What is a colloid? • How do colloids work? • How do the colloids differ? • Are there any bad effects? What are we going to talk about • Physiology of fluid movement • Types of fluids and distribution • Physiology of Colloids • Some of the controversies My last day in the OR • 80kg, 40 year old male, traumatic fall, compartment syndrome and ‘smashed ankle’. • Here for a free flap. • Cases starts at 0730. ends at 2130. How much fluid should I give him? • Have to account for several factors: • • • • Deficit Maintenance 3rd space losses Blood loss How do you calculate this? • 4‐2‐1‐ rule gives you maintenance rate. • 4cc/kg/hr for the 1st 10kg • 2cc/kg/hr for the 2nd 10kg • 1cc/kg/hr for every kg above 20kg • • • • • 40cc + 20cc + 60 cc= 120cc/hr maintenance. Assume 8 hours of fasting, so 1L deficit. 14hr Surgery x 120cc/hr= 1700cc 3rd space losses=6700cc Blood loss 1000cc=4000cc cryst. Total=13,400cc The next day Does it matter at all? Why give fluids? Reduced Reduced Circulating Circulating Volume Volume Inadequate Inadequate Tissue Tissue Perfusion Perfusion Gut Mucosal Barrier Disruption Translocation of Bacteria/Endotoxin Activation Activation of of Inflammatory Inflammatory Pathways Pathways MODS MODS What’s the downside? What’s the downside? What’s the downside? Complications Hypovolemic Optimal Overloaded Volume Load Physiology of fluid movement • How does the fluid get to where we don’t want it? • Governed by starling forces Volumes of body fluid compartments Distribution of various solutions Plasma Volume Expansion= Volume of compartment Infused into Volume of Distribution For Example • Infuse 1L of D5W • It distributes evenly throughout fluid compartments So 3L ≅ 7%PVE 45L • Infuse 1L of NaCl 3L ≅ 20%PVE 15L • Infuse 1L of colloid 3L ≅ 100%PVE 3L Why use a colloid? Less volume Longer lasting ‘Suck fluid’ from the interstitium Able to replace blood volume 1:1 versus 3:1 or 4:1 • Associated with better outcomes • • • • Why wouldn’t you use a colloid? • Expense • Bleeding risk • Risk of adverse renal outcomes • Not a believer What kind of colloids are there? Synthetic Colloids Produced by hydroxyethylating maze. Synthetic Colloids Synthetic Colloids ® 450/0.6 • 6% Hespan 6% • 6% Hextend® 670/0.7 • 10% Pentaspan® 260/0.45 • 6% Haes‐Steril® 200/0.5 • 6% Voluven® 130/0.4 Classification of Colloids • Concentration • Molecular weight • Degree of Substitution • C2:C6 ratio Concentration • In Canada, 10% and 6% solutions available. • 10% Solution is Hyperoncotic, 6% isooncotic. What does oncotic refer to? • Oncotic pressure or colloid osmotic pressure • The pressure required to prevent the movement of small ions and solvent. • Normal in plasma is ~25mmHg. • Pentaspan 80mmHg • Voluven 36mmHg • 25% HSA 80mmHg What do all the numbers mean? 264/0.45/13 First Number: Molecular Weight • HES are ploydisperse substances. • They contain a distribution of molecular weights. • The number on the package is the average. •After infusion the molecules are broken down by endo‐ amylases. •If their size is below the renal threshold, they are excreted. •Hydroxyethylation slows down the rate of breakdown. • Low MW solutions have more molecules per volume. • This gives them a greater oncotic effect. • Also gives them less persistence in plasma. • Contrast this with larger molecules. Second number: Molar substitution • This is where the drugs derive their name. • 0.6 = Hextend • 0.5 = Pentaspan • 0.4 = Voluven (a tetrastarch) Second number: Molar substitution • Proportion of the carbon atoms that are hydroxyethylated. • Expressed as a number from 0 to 1. • Most starches are substituted in the C2 or C6 position. Third Number: C2:C6 ratio • Refers the the proportion of molecules that are hydroxyethylated at the C2 vs he C6 position. • A higher C2:C6 ratio results in longer intravascular half life. Adverse effects of colloids • Hemostatic • Dermatologic • Renal Hemostatic Effects Hemostatic Effects • Seems to be more pronounced with the slowly degraded starches. • Predominant effect is on vWF:VIII. • Some platelet effects, but these are non‐ significant. Hemostatic Effects • We’re Ok using Pentaspan, Voluven. • There is a dilutional effect, but this is only relevant at very high doses. Hemostatic Effects • Dinosaur Starches are associated with bleeding, the newer ones aren’t. Hemostatic Effects • Numerous studies have shown no change in bleeding with the newer starches. • (Chest tube losses, coagulation factors, TEG). Renal Effects Renal Effects Renal Effects • The starch was 240/0.6 • Similar but different. • Probably not the best group to test your hypothesis in. Renal Effects What does VISEP answer? • What happens when you give a toxic dose of a drug? •This wasn’t Pentaspan or Voluven. •10% 200/0.5 (Hemohes). •It was a hyperoncotic solution. •This drug can accumulate in plasma. • The dose was as high as 500‐750cc/day. Good thing 25% Albumin is OK!! Albumin in the critically ill Albumin in the critically ill • • Cochrane review in 1998 of the 30 trials of albumin involving over 1400 patients 6 additional deaths for every 100 patients treated. •Randomized patients to either 4% albumin or abnormal saline. Not so good for the brain! Not so good for the brain! DON’T MINIMIZE THE EFFECT OF HYPERONCOTIC SOLUTIONS! • PEff= (Pcap –PBow ) ‐ Ppla Remember, it’s 25% Albumin • Hyperoncotic albumin has been known to be a cause of renal failure since the 1980s. • Using a hyperoncotic solution with little crystalloid may be bad. Albumin 10 Commandments of Fluids D5W and D5 ½ NS have no role in resuscitation. Crystalloids have an ephemeral intravascular presence. Normal Saline is not Normal. Colloids are drugs, and have a dosage and side effects. Aim for a balanced resuscitation. Blood transfusions are bad, but anemia might be worse. Your average, stable ICU patient is (almost) NEVER hypovolemic. VIII. There is no role for ‘maintenance fluids’ for patients on full tube feeds. IX. Positive fluid balance is associated with worse outcomes. X. Don’t covet my slides. I. II. III. IV. V. VI. VII.