* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Appendix I - Cairdtech
Heart failure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Jatene procedure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Electrocardiography wikipedia , lookup
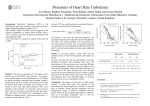
Model 2000 Digital Ambulatory ECG Holter System Heart Rate Turbulence — is the physiological, bi-phasic response of the sinus node to premature ventricular contractions. It consists of a short initial acceleration followed by a deceleration of the heart rate. HRT can be quantified by two numerical parameters, namely the Turbulence Onset and the Turbulence Slope. HRT is most probably an autonomous baro-reflex. The premature ventricular contraction causes a brief disturbance of the arterial blood pressure (low amplitude of the premature beat, high amplitude of the ensuing normal beat). When the autonomic control system is intact, this fleeting change is registered immediately with an instantaneous response in the form of HRT. If the autonomic control system is impaired, this reaction is either weakened or entirely missing. HRT is suitable for assessing the risk following myocardial infarction. After analysis of the data of more than 3,000 postinfarction patients it was established that HRT is - independent of other risk predictors - the most powerful ECG-related risk predictor. The predictive value of HRT is comparable with that of the ejection fraction of the left ventricle. Turbulence Onset The percentage difference between the average value of the first two normal intervals following the PVC and of the last two normal intervals preceding the PVC. Initially, TO is determined for each individual PVC, followed by the determination of the average value of all individual measurements. TO is determined for each individual PVC, followed by the determination of the average value of all individual measurements. Positive values for Turbulence Onset indicate deceleration, negative values indicate acceleration of the sinus rhythm. Turbulence Slope The steepest slope of a linear regression line through five consecutive measurement points in the averaged tachogram. The Turbulence Slope calculations are based on the averaged tachogram and expressed in ms per RR interval The algorithm for HRT quantification can only deliver usable results if the triggering event was a true PVC (and not an artefact, T-wave or similar). In addition it must be ensured that the sinus rhythm immediately preceding and following the PVC is free from arrhythmia, artefacts and false classifications. In order to fulfill these requirements, we use filters which exclude RR intervals with the following characteristics from the HRT calculation: < 300 ms > 2000 ms > 200 ms difference to the preceding sinus interval > 20% difference to the reference interval (mean of the 5 last sinus intervals) Appendix I Page 1 of 7 Model 2000 Digital Ambulatory ECG Holter System In addition, we limit the HRT calculations to PVCs with a minimum prematurity of 20% and a post-extrasystole interval which is at least 10 % longer than the normal interval Appendix I Page 2 of 7 Model 2000 Digital Ambulatory ECG Holter System Methods for the Assessment of Heart Rate Turbulence in Holter- ECGs Raphael Schneider, Petra Barthel, Georg Schmidt , I. Medizinische Klinik der Technischen Universität & Deutsches Herzzentrum München, Germany Background Heart Rate Turbulence (HRT) is a new and powerful predictor of mortality in post- infarction patients. In low risk patients, sinus rhythm after a VPC exhibits a characteristic pattern with an immediate acceleration and a subsequent deceleration (figure, upper panel). Such a pattern cannot be observed in high risk patients (figure, lower panel). Aim of the study was to develop and to optimize descriptors of HRT. Patients 100 CHD patients with sinus rhythm and >10 VPCs/ h during 24- h Holter monitoring. Table 1 shows the patient characteristics. The Follow- up period was two years. Table 1: Patient characteristics n Deaths (n) Age, years Gender (f/ m) Previous MI (n) LVEF (%) VPC /h 100 17 62.8 9.7 15/ 18 26 (26%) 46.4 14. 6 176. 2 209.5 Methods The Holter tapes were processed with an Oxford Excel 2 system. After visual inspection and manual editing, computer files were created listing RR interval duration (sampling frequency 128 Hz) and QRS morphological classifications. For the quantification of HRT, ten different descriptors were tested. These included the difference of the heart rate before and after the VPC, the difference between the maximum and minimum RR interval, the standard deviation of the RR intervals, the slope of the steepest regression line assessed over n subsequent RR intervals within the first 20 RR intervals after Continuous variables were compared by the Mann- Whitney test. For dichotomized variables the Cox proportional hazards model with a stepwise forward procedure was used. Cut- off points for the dichotomization of the HRT descriptors in “normal” and “abnormal” values were determined by the method of maximizing the log- rank test statistics. Results Two HRT descriptors were significant: “Turbulence Onset” (TO) which describes the early acceleration and “Turbulence Slope” (TS) which describes the subsequent deceleration. The both descriptors are calculated as follows (see figure): TO is the mean of the first x sinus RR intervals following a VPC divided by the mean of the last x sinus RR intervals before the VPC. TS is the maximum positive slope of a regression line assessed over any sequence of n subsequent sinus RR intervals within the first 20 sinus RR intervals after a VPC. Table 2: Association of TO with mortality with varying number of RR intervals used #RRIs used 1 2 3 45 p- value 0. 195 0.009 0.071 0. 060 0.140 Table 3: Association of TS with mortality with varying number of RR intervals used #RRIs used 3 4 5 6 7 p- value 0. 018 0.015 0.007 0.008 0. 013 TO and TS contain additional mortality information to other known risk indicators such as age, previous MI, mean heart rate, heart rate variability index and left ventricular ejection fraction. (see table 4.) Appendix I Page 3 of 7 Model 2000 Digital Ambulatory ECG Holter System Table 4: Association of HRT descriptors and known risk variables with total mortality p- value of Cox analyses Risk indicators univariate multivariate TO 1.0 TS 2.5 ms/ RRI 0. 0006 <0. 0001 0.049 0. 0002 Age 65 years Previous MI Mean HR > 75 bpm HRV Index 20 units LVEF < 30% 0.024 0.048 0. 0001 0.021 0.049 Conclusion Turbulence Onset and Turbulence Slope are good descriptors of heart rate turbulence and provide information on the risk of subsequent mortality independent of other known. 700 800 900 1000 -5 0 5 10 15 700 800 900 R R inte rva l ( ms ) # beats TO TS Figure: Heart rate turbulence: The upper part shows the typical pattern of a long term survivor. The lower part shows the HRT tachogram of a patient who died three months after acute myocardial infarction. Appendix I Page 4 of 7 Model 2000 Digital Ambulatory ECG Holter System Heart Rate Turbulence is a Post-Infarction Mortality Predictor which is Independent of and Additive to Other Recognised Risk Factors Marek Malik, PhD, MD, Georg Schmidt, MD, Petra Barthel, MD, Raphael Schneider, MEng, Maria Teresa La Rovere, MD, J Thomas Bigger Jr, MD, Peter J Schwartz, MD, St. George’s Hospital Medical School, London, England, Technical University, Munich, Germany, S Maugeri Foundation, University of Pavia, Italy, Columbia University, New York, NY Heart rate turbulence (HRT) is a newly established risk factor which characterizes the early acceleration (HRT Onset) and late deceleration (HRT Slope) of sinus rhythm following ventricular premature beats. Absence of HRT has been shown to be a very strong mortality predictor after myocardial infarction but its additive value in combination with other risk factors has not been examined in detail. Methods: HRT Slope was measured in Holter recordings of 912 patients enrolled into the ATRAMI study of whom 34 died during the 2-year follow-up. In these patients, baroreflex sensitivity (BRS), left ventricular ejection fraction (LVEF), mean 24-hour heart rate (mHR) and 24-hour heart rate variability (HRV) -the SDNN measure, were also available. Univaritate positive predictive characteristics (PPC) for the prediction mortality were computed for all these indices and multivariate PPC were computed based of the combination of HRT Slope with each other risk factor. Results: In the practically relevant range of 30% - 50% sensitivity, HRT Slope was the strongest univariate predictor (Left figure: bold line). At 40% sensitivity, the positive predictive accuracies (PPA) were as follows: HRT slope 12.5%, BRS (circles) 7.8%, LVEF (triangles) 10.9%, mHR (squares) 10.4%, HRV (diamonds) 9.9%. In a multivariate analysis, HRT Slope was additive to every other risk predictor (Right figure). At 40% sensitivity, HRT Slope best combined with HRV (PPA of 20.3%) and with LVEF (PPA of 17.3%) Conclusion: The predictive power of HRT Slope is not only stronger that that of other predictors, but also additive to other mortality predictors. Appendix I Page 5 of 7 Model 2000 Digital Ambulatory ECG Holter System Heart Rate Turbulence: Rate of Frequency Decrease Predicts Mortality in Chronic Heart Disease Patients Raphael Schneider, MEng, Andreas Röck, Petra Barthel, MD, Marek Malik*, PhD, MD, A. John Camm*, MD, Georg Schmidt, MD, 1. Medizinische Klinik und Deutsches Herzzentrum der Technischen Universität München, Germany, *St. George’s Hospital Medical School, London, UK Heart rate turbulence (HRT) is a newly established risk predictor which characterizes the early acceleration (HRT Onset) and late deceleration (HRT Slope)of sinus rhythm following ventricular premature complexes (VPCs) (left figure). HRT has shown to be a strong mortality predictor after myocardial infarction. The local tachogram after a VPC (right figure, thin line) can be described by an oscillation with a decreasing frequency over time (right figure, thick line). This study was performed to investigate if the rate of frequency decrease (HRT frequency decrease) is correlated with mortality and is independent of other known risk indicators. Methods: One hundred patients suffering from coronary artery disease with sinus rhythm and >10 VPBs/h during 24-h Holter monitoring were used. During a 2-year follow-up period, 17 patients died. We calculated oscillations with different rates of frequency decrease. The HRT frequency decrease which minimized the square error between the model and the original data was used as risk parameter. Total mortality was used as the endpoint. Results: Using multivariate Cox analyses, the rate of frequency decrease was significantly associated with mortality (p < 0.03) and independent of other known risk indicators such as age, arrhythmia, mean heart rate, heart rate variability, HRT Onset, HRT Slope and left ventricular ejection fraction. Conclusion: The tested model allows a good description of HRT. Patients with a slow HRT response are at enhanced risk. Appendix I Page 6 of 7 Model 2000 Digital Ambulatory ECG Holter System Heart Rate Turbulence in Patients With and Without Autonomic Dysfunction Petra Barthel, Georg Schmidt , Raphael Schneider, Kurt Ulm, Marek Malik*, Albert Schömig, 1. Medizinische Klinik & Deutsches Herzzentrum, Technische Universität München, München, Germany, * St. George's Hospital Medical School, London, UK Background: Heart Rate Turbulence (HRT) is a phenomenon, described by our working group, based on fluctuations of sinus rhythm cycle length after single ventricular premature beats (VPBs). HRT is a biphasic reaction and can be quantified by two numerical parameters (turbulence onset: TO; and turbulence slope: TS). Both parameters are potent risk stratifiers in post-MI patients which are independent of each other and other known risk factors. We hypothesize that TO and TS reflect specific autonomic regulations. This study was performed to investigate whether HRT is affected by autonomic dysfunction. Methods: In 100 patients (pts) with coronary artery disease, HRT was assessed using Holter-ECGs. TO and TS were dichotomized into ‘normal’ and ‘abnormal’ values using predefined cut-off-points. Pts were divided into two groups according to the history of diabetes mellitus (G0: no diabetes, G1: diabetes). Univariate and multivariate Cox regression analysis was performed to test the differences between the two groups. In the multivariate analysis, age, history of previous infarction, left ventricular ejection fraction (LVEF), mean heart rate, and SDNN were included. Primary endpoint was cardiac mortality. Results: With the univariate approach, TO was a significant predictor of cardiac mortality in G0 and G1 (p<0.05 respectively). TS was a significant predictor in G0 (p<0.0001), but not in G1 (p=0,56). With the multivariate approach, we found 3 independent risk parameters (TS p<0.001, LVEF p<0.05, age p<0.05) in G0. In G1, LVEF was the only independent variable (p<0.02). Conclusion: Our findings support our hypothesis that TS is mediated by a autonomic reflex presumably a baroreflex activated by the changes of the arterial pressure during and after VPBs. Appendix I Page 7 of 7