* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Anti-seizure
Survey
Document related concepts
Transcript
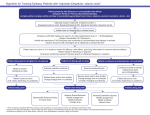
Pharmacology: Antiseizure Drugs (Bannon) SEIZURES: Definition: finite episodes of brain dysfunction resulting from abnormal discharge of cerebral neurons Types: Partial Seizures (Simple): o Consciousness preserved (simple) o Various manifestations: Convulsive jerking Paresthesias Psychic symptoms (altered sensory perceptions, illusions, hallucinations, affect changes) Autonomic dysfunction Partial Seizures (Complex): o Impaired consciousness (complex) that is preceded, accompanied, or followed by psychologic symptoms Tonic-Clonic Seizures (Generalized): o Tonic phase involves abrupt LOC, muscle rigidity and respiration arrest (less than 1 minute) o Clonic phase involves jerking of body muscles, with lip or tongue biting, and fecal and urinary incontinence (2-3 minutes) o Formerly called grand mal seizures Absence Seizures (Generalized): o Impaired consciousness (often sudden onset and brief) o Sometimes accompanied by automatisms, loss of postural tone, or enuresis o Begin in childhood and usually cease by age 20 o Formerly known as petit mal seizures Myoclonic Seizures: o Single or multiple myoclonic jerks Status Epilepticus: o A series of seizures (usually tonic-clonic) without recovery of consciousness between attacks o Life-threatening emergency Risk Factors: Children: fever, mental retardation, cerebral palsy, genetics Adults: trauma, tumors Elderly: Alzheimer’s Disease, Stroke DRUGS AND OTHER TREATMENTS FOR SEIZURES: General: First Generation Drugs: o Use: effective for the treatment of generalized tonic-clonic and partial seizures Many rate-dependently prolong inactivation of voltage-gated Na channels (similar to lidocaine) Others potentiate GABA by several mechanism o Use: effective against generalized (absence) seizures Thought to block T-type Ca channel-mediated current in thalamic neurons Newer Drugs: o Newer Phenotypic Models: mutant mice, models of kindling or neuropathic pain o Targeting of Defined Biochemical Mechanisms: GABA uptake, metabolism, receptor effects o Novel AD Targets: glutamate receptors (NMDA), K+ channels (open to hyperpolarize) or Ca++ channels Drugs with Broad Spectrum of Action: o May be due to multiple mechanisms of action and/or novel mechanisms of action Drugs for Partial and Generalized Tonic-Clonic Seizures: Drugs of Choice: o Phenytoin (Dilantin): History: oldest nonsedative antiseizure drug MOA: blockade of Na channels is the strongest effect (but not the only effect) at therapeutic concentrations Pharmacokinetics: Absorption: highly dependent on the formulation o Fosphenytoin: soluble prodrug that allows for IM or IV administration Elimination: via the liver; dose-dependent and need to titrate dose slowly Toxicity/Side Effects: Nystagmus early Diplopia and ataxia are dose-limiting effects Gingival hyperplasia and hirsutism are common long-term Idiosyncratic reactions are rare Use: considered a 2nd line drug by some, but still one of the most widely used drugs in the world o Carbamazepine: Structure: tricyclic compound related to some antidepressants Other Uses (Besides Seizures): Treatment of BPD Treatment of trigeminal neuralgia Drug abuse (?) MOA: blockade of Na channels is the primary effect Pharmacokinetics: Metabolism: significant microsomal induction and may have to adjust dose of this and other drugs over time (ie. induces its own metabolism) Toxicity/Side Effects: Diplopia and ataxia (dose-related) Idiosyncratic blood dyscrasia in the elderly Stevens-Johnson Syndrom (rare but serious skin reaction) o Genetic risk determined by presence of a specific HLA allele (testing recommended by FDA) o 10x higher risk in Asians Side effects may be decreased with ER formulation Important: may exacerbate myoclonic and absence seizures (do not use for these) o Valproic Acid: Use in Seizures: Partial seizures Generalized tonic-clonic Myotonic seizures Atonic seizures Generalized (absence) seizures Combination seizures Other Uses (Besides Seizures): Treatment of BPD Treatment of migraine (Divalproex sodium ER) MOA: unclear; broad spectrum of action most likely due to multiple MOA Blockade of Na channels possible GABA effects may also be relevant Histone deacetylation inhibition to INCREASE gene expression (potentiation of Sp transcription factor family turns on a bunch of genes) May also have effects on Ca++ channels (due to efficacy against absence seizures) Side Effects: serious effects are rare, but may not be first line due to these rare events Severe idiosyncratic hepatotoxicity (requires monitoring of liver function) Formulations: Divalproex Sodium ER: used once daily o Complex partial seizures o Absence seizures o Migraine Alternative Drugs: o Phenobarbital: MOA: potentiate GABA effects Use: rapid effects, safety profile and low cost can make it a DOC Side Effects: sedative effects can be limiting o Lamotrigine: MOA: blockade of Na channels; may have additional MOAs due to broad spectrum of activity - Use: shown to be as effective as the DOCs (may now be considered one) Side Effects: rare but life-threatening dermatitis possible in infants o Levetiracetam: MOA: binds SV2A to interfere with release of NT Use: very good for refractory seizures in adults and children (another possible DOC) Side Effects: well tolerated o Gabapentin and Pregabalin (Lyrica): MOA: binds voltage gated Ca channel subunit (not related to GABA) Other Uses (Besides Seizures): Neuropathic pain Migraine Anxiety Surgical analgesia o Topiramate (Topamax): MOA: broad spectrum drug, probably with multiple MOAs Use: hot drug for off-label use Refractory migraine BPD Many other disorders Side Effects: typical CNS side effects and memory problems Drugs for Generalized (Absence) Seizures: Drugs of Choice: o Ethosuximide: Use: ONLY a first line drug for absence seizures (no other types) MOA: blocks T-type Ca++ channel Pharmacokinetics: Absorption: good Metabolism: complete Toxicity: well tolerated Dose-related gastric distress More rare instances of rashes and psychosis o Valproic Acid: already described o Clonazepam: Use: Absence seizures (may be less effective that ethosuximide or valproic acid) Myoclonic seizures Atonic seizures Infantile spasms Side Effects: typical benzo side effects that limit use Sedation Development of tolerance Withdrawal syndrome Treatment of Status Epilepticus: Treatment: o IV diazepam or lorazepam o Followed by IV fosphenytoin or phenobarbitol Important Point: watch for synergistic CNS depression when combining these drugs! Other Aspects of Antiseizure Drug Therapy: Teratogenicity: o Difficult to assess: due to seizures and heterogeneity of these medications Most pregnant patients on these drugs deliver normal infants Apparent overall 2X increase in risk of congenital malformations when on the drugs (no increased risk if off the drugs during pregnancy) If you choose to keep them an a drug (which is typically done), use the lowest effective dose of monotherapy o Specific Known Risks: Phenytoin: fetal hydantoin syndrome (?) Valproic Acid: risk of spina bifida (1-2%) and possible effect on IQ - Drug Withdrawal: o Most difficult for people on benzodiazepines and barbiturates o ~70% of people with epilepsy enter remission while on medications (>5 years seizure free) o ~75% of these patients can be successfully and gradually withdrawn from their medications Other: o Increased suicide risk (2X) o Decreased bone density (chronic use) Future of Pharmacotherapy for Seizures: Large number of candidate drugs being identified through high-throughput screening Some have novel MOAs and should be useful/improve the treatment of refractory epilepsy Improved understanding of genetic and cellular basis for epilepsy will lead to more precisely targeted therapeutics and new strategies to delay/prevent epileptogenesis Ketogenic Diet: History: o Fasting formerly used to treat epilepsy o Lost favor because of practical difficulties and antiquated medical theories Description: o Low calorie diet with 4 grams of fat per gram of protein or carbs o Diet creates ketones by fat metabolism (mimics fasting) and ketones replace glucose as fuel o Not entirely clear what the MOA of this diet is with regard to seizure treatment o Strict adherence is required (children need to initially be hospitalized to ensure adherence) Use: o Treatment of refractory seizures in children (ie. Lennox-Gastaut Syndrome) Surgery: Anterior Temporal Lobectomy: o Use: very effective for refractory and harmful cases of the most common partial seizure of adults o Results: most patients seizure free for 5 years (enter remission) Corpus Callostomy: o Use: Lennox-Gastaut Syndrome (difficult to treat childhood onset form of epilepsy characterized by frequent and different types of seizures) Hemispherectomy: o Use: other severe forms of childhood epilepsy Ramussen Syndrome (rare chronic inflammatory neurological disorder) Sturge Weber Syndrome (rare congenital neurological and skin disorder) Vagus Nerve Stimulation (NeuroCybernetic): o Use: Refractor complex partial and generalized seizures Poor surgical candidates Now being tested in children Also used in depression, anxiety and other disorders o Response: MOA is unclear but clearly effective Good response (seizure reduction in 30-75% of patients) Therapeutic Principles for the Management of Epilepsy: Pre-Therapy: o Determine cause of seizures if possible o For children, wait and see before treating after a single, unprovoked seizure Therapy: o Use a drug of choice appropriate for the seizure type Partial Seizures and Generalized Tonic-Clonic: phenytoin, carbamazepine, valproic acid Possibly: phenobarbital, lamotrigine, levetiracetam Generalized (Absence) Seizures: ethosuximide, valproic acid, clonazepam o Therapeutic index and toxicity not uncommon with most antiseizure drugs, so need to ensure adequate trial of a single drug AND monitor plasma levels closely Cases of Treatment Failure: o Occurs in as many as ½ of patients- first try monotherapy with another first line drug o If total pharmacological failure (20-30% of patients), consider surgery or vagal nerve stimulation