* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Lipid Solubility Modulates pH Potentiation of Local Anesthetic Block
Survey
Document related concepts
Transcript
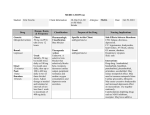
513 Lipid Solubility Modulates pH Potentiation of Local Anesthetic Block of Vmax Reactivation in Guinea Pig Myocardium Archer Broughton, Augustus O. Grant, C. Frank Starmer, Jayne K. Klinger, Bruce S. Stambler, and Harold C. Strauss From The Division of Cardiology, Department of Medicine, and Department of Pharmacology, Duke University Medical Center, Durham, North Carolina Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 SUMMARY. Current theories envision recovery from local anesthetic block of sodium channels via slow hydrophilic and fast hydrophobic paths. Extracellular pH reduction which increases cationic/neutral anesthetic form should especially prolong recovery kinetics of highly lipid soluble compounds that could readily exit via the hydrophobic pathway at normal extracellular pH. To test this hypothesis, we compared the effects of three related compounds with similar pKa on the time course of Vmax reactivation in guinea pig papillary muscle at pH<, 7.4 and 6.95. The compounds were lidocaine and its two desethylation products, monoethylglycinexylidide and glycinexylidide. Judged from the octanol:water partition coefficient, lidocaine was the most lipid soluble (log partition coefficient 2.39 ± 0.10), followed by monoethylglycinexylidide (log partition coefficient 1.32 ± 0.09) and glycinexylidide was the least lipid soluble (log partition coefficient 0.41 ± 0.09). At 30 MM and pHo 7.4, the potency order for Wmix depression at zero diastolic interval was lidocaine (53 ± 6%), monoethylglycinexylidide (17 ± 3%), and then glycinexylidide (7.8 ± 1.9%). The decay of V ^ block appeared monoexponential, and the time constant of recovery was dose independent. Most important is the fact that there were significant differences in the r r increase with extracellular pH reduction (P < 0.05; Scheffe contrasts). The increase was greatest with lidocaine [73 ± 28% (mean ± SD)], less with monoethylglycinexylidide (42 ± 15%), and least with glycinexylidide (13 ± 17%). The simplest interpretation of the differences in extracellular pHdependence of recovery kinetics was that recovery from block due to the neutral form of these ionizable local anesthetics depended on lipid solubility, whereas recovery from block due to the protonated form depended on molecular weight. (Circ Res 55: 513-523, 1984) IONIZABLE antiarrhythmic drugs such as lidocaine possess the useful property of more potent electrophysiological action in ischemic than in normal myocardium (Kupersmith et al., 1975; Hille, 1978; Hondeghem, 1976; Allen et al., 1978; Lazzara et al., 1978; Cardinal et al., 1981). This potentiation has been attributed in part to an increase in H + concentration within ischemic areas (Kupersmith et al., 1975). Measurements of phase 0 V ^ , reactivation in guinea pig papillary muscle (Grant et al., 1980) and sodium conductance reactivation in voltageclamped nerve, skeletal muscle, and Purkinje fibers (Khodorov et al., 1976; Schwarz et al., 1977; Bean et al., 1982) indicate that recovery from local anesthetic sodium channel block is delayed by extracellular pH reduction. Acidosis is thought to increase the proportion of channels occupied by the protonated form of the local anesthetic base (Kupersmith et al., 1975; Schwarz et al., 1977). Experiments with permanently charged quaternary amine local anesthetics in nerve and heart indicate that hydrophilic protonated drug molecules unblock with much slower kinetics than more lipid-soluble neutral forms (Strichartz, 1973; Schwarz et al., 1977; Gin- tant et al., 1983). The kinetic difference has been attributed to the very large difference in lipid solubility (Hille, 1977; Schwarz et al., 1977; Courtney, 1980). However, studies examining heterogeneous groups of local anesthetic amines at normal pH have produced conflicting conclusions as to the importance of lipid solubility in determining recovery kinetics (Courtney, 1980; Campbell, 1983). If lipid solubility is of pivotal importance, pH reduction should especially prolong recovery kinetics of compounds with highly lipid-soluble neutral form, since these would readily unblock via the membrane phase at normal pH. We thought it would be of advantage to restrict the comparison to a small group of related compounds with different lipid solubility and similar values for pKa; we therefore chose to examine the electrophysiological properties of lidocaine and its two desethylation products, monoethylglycinexylidide (MEGX) and glycinexylidide (GX). Dealkylation is expected to reduce lipid solubility (Hansch and Leo, 1979). We were particularly interested in determining whether there was a corresponding reduction in the pH dependence of recovery kinetics. Circulation Research/Vo/. 55, No. 4, October 1984 514 The cellular electrophysiological properties of MEGX and GX have not previously been described. They have been shown to accumulate in the plasma of patients and dogs receiving lidocaine and to partition into the myocardium to an extent similar to lidocaine (Strong et al., 1973; Halkin et al., 1975; Handel et al., 1983). MEGX appears to possess antiarrhythmic and convulsant properties comparable to lidocaine, whereas GX appears considerably less potent (Smith and Duce, 1971; Blumer et al., 1974; Tenthorey et al., 1981). We determined lipid solubility by octanol:H2O partition coefficient (P). The kinetics of recovery from block of phase 0 Vmax were assessed by determining the time constant of recovery (rr) in guinea pig papillary muscle at normal and low pH using conventional microelectrodes. Methods Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 Tissue Preparation and Apparatus Guinea pigs (250-350 g) were stunned and the hearts rapidly removed and dissected in room temperature-oxygenated Krebs-Henseleit solution. Right ventricular papillary muscles (0.8-1.0 mm in diameter) were mounted in a three-compartment sucrose gap chamber. The length of muscle in the test chamber was limited to 0.5-1.0 mm (Reuter and Scholz, 1968). The 0.7-ml capacity test compartment was perfused at 3 ml/min. Bath temperature was monitored by thermister (YSI no. 511 probe) and controlled to 36 ± 1°C. The preparation was stimulated with constant current pulses, 2 msec in duration. Pulse amplitude was that required to maintain constant latency (usually 2 msec) between end of stimulus and peak upstroke velocity of the action potential. Transmembrane potential was recorded differentially between two glass microelectrodes containing 3 M KC1 (resistance 15-30 Mfi). In most experiments, the microelectrode tips were beveled to reduce resistance to 15-20 MQ. One electrode impaled the cell and the other was positioned in close proximity just above the tissue surface. The microelectrodes were coupled via Ag/AgCI half-cells (WPI EH-3FS) to matched voltage followers having high input impedance (1010Q) and input capacity neutralization. The output of the voltage followers was amplified by the 3A9 differential amplifier of a Tektronix 565 oscilloscope. The maximum rate of rise of the transmembrane potential (V^*) was obtained by electronic differentiation (differentiator output linear over the range 10-1000 V/sec). Oscilloscope traces of the action potential and its time derivative were photographed by a Grass C4 camera and enlarged (8x) for analysis by projection onto a digitizing tablet. Solutions Under control conditions, the anterior (test) compartment was perfused with Krebs-Henseleit (K-H) solution at pH 7.4, containing (ITIM): NaCl, 118; NaHCO3, 21; KC1, 4.3; MgSO4, 1.2; glucose, 11. The solution was gassed continuously with 95% O2, 5% CO2 starring 10 minutes before the addition of CaCh. To test the effects of acidosis, we reduced pH to 6.95 by replacing all but 7.5 rrtM NaHCO3 with NaCl. The pH of the solution was titrated to 7.4 or 6.95 by the addition of HC1 or NaOH, using a high precision pH analyzer (IL Inc., model 113). Preliminary experiments showed that solution pH remained constant from solution reservoir to anterior chamber; we routinely monitored reservoir pH, not anterior chamber pH, to avoid disturbing the preparation. Acidosis increases ionized calcium activity (Spitzer and Hogan, 1979). The present pH reduction increased the ionized calcium activity of our K-H solution from 1.41 ± 0.01 to 1.57 ± 0.01 mM (mean ± SD, n = 3). We decided not to reduce the calcium concentration of the pH 6.95 solutions to counteract this change, since no such compensation would occur in vivo. The middle compartment was perfused with isotonic sucrose solution containing 0.01 mM CaCl2 and gassed with 100% O2. The posterior (current-injecting) compartment was perfused with isotonic KC1 solution produced by substitution of all NaCl in the standard K-H solution. Procedures An initial 60-minute equilibration period in control solution was allowed. Once a stable impalement had been obtained, action potential characteristics and Vmax recovery kinetics were recorded. Recordings were repeated after 30, 60, and 120 minutes of exposure to lidocaine, MEGX, and GX, respectively. Only one drug was tested in each preparation. The metabolites, being less lipid soluble, required longer exposure times to produce a stable effect than did lidocaine. The basic drive stimulus (SI) was delivered in repetitive 10-beat trains at 1 Hz separated by 2-second pauses. By definition, diastole began when phase 3 repolarization had returned the membrane potential to 1 mV from its resting value. To determine recovery kinetics, a test stimulus (S2) was introduced at varying diastolic intervals following successive trains. Any reduction in Vmax of the test action potential was expressed as a fraction of the amplitude during the preceding basic drive action potential according to the expression: fractional Vmax reduction, (b) = (VmaxSi - VmaxS2)/Vmai<si. Since Vmax reactivation followed a single exponential in the present experiments, the decay of b from its value at zero diastolic interval (b0) is given by b(t) = b0 exp (—t/r,), where T, is the time constant of reactivation. Thus b decays linearly over time in a semilogarithmic plot. After logarithmic transformation of b, linear regression techniques were used to obtain least squares estimates of b0 and the slope (regression coefficient) of the decay. rr is simply the inverse slope. It was easier to measure the kinetics of recovery from lidocaine block of Vmax than metabolite block, because of lidocaine's greater potency. With GX, the least potent, it was necessary to average =5 replications at each diastolic interval to obtain a sufficiently noise-free estimate of the time course of Vmax reactivation. This approach was used in all GX experiments and some MEGX experiments. However, our criteria for adequate kinetics determination (see Statistical Analysis) could be satisfied for MEGX and lidocaine without the use of replication. In some preparations, the effects of two concentrations of a single drug were examined (15 and 30 /IM lidocaine or MEGX; 30 and 120 //M GX). To test the effects of low HCO3 acidosis in drug-free solution and during exposure to drug, the sequence of pH 7.4 and 6.95 solutions was: pH 7.4 (60 minutes), pH 6.95 (20 minutes), pH 7.4 (20 minutes), pH 7.4 with drug (30, 60, or 120 minutes for lidocaine, MEGX or GX, respectively), pH 6.95 with drug (20 minutes), pH 7.4 with drug again (60 minutes). Because of the difficulty in maintaining long impalements, it was often not possible to record the entire sequence within the one cell. Partial experiments are reported pro- 515 Broughton et al./pH, Lipid Solubility, and Vmax Reactivation Block vided data were collected from the same cell before and during the particular intervention being examined. That is, a return to pre-intervention conditions was not always possible. Octanol:H2O Partitioning Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 Differences in lipid solubility between lidocaine and its two metabolites were assessed by comparison of octanol:water partition coefficients. Partitioning was examined 2 pH units above, and 2 pH units below, drug pKa to reflect properties of neutral and charged drug molecules, respectively. Siliconized 15-ml glass test tubes containing cross-saturated octanol (2 ml) and water (2 ml) were gently rocked for 1 hour at 23°C after the addition of drug. The water was pipetted off after centrifugation at 1500 rpm for 5 minutes. Initial aqueous phase drug concentration (=167 Mg/ml) and final aqueous concentration after partitioning were measured by reverse phase ion-pair HPLC (Laboratory Data Control, model 1204A; 4.6 mm X 25 cm, Zorbax ODS column). The mobile phase contained 4.52 g NaH2PO4, 10 ml triethylamine (Aldrich), and 130 ml acetonitrile (Fisher Scientific, HPLC grade). Mobile phase pH was lowered to 3.0 with phosphoric acid before the addition of acetonitrile. The mobile phase was pumped at 1.9 ml/min, and the UV detector was set to measure absorbance at 200 nm. Estimates of drug concentration were the average of five replications. Statistical Analysis Student's f-test for paired data was used to assess the significance of pairwise comparisons within cells (resting membrane potential before and during drug exposure, or at two different pH values, etc.). The value during an experimental intervention was compared to the average of the value before and the value following recovery if both were available—otherwise, to the value beforehand. To compensate for simultaneous multiple comparisons, for example, when assessing the effect of GX 30 /xM on resting potential, action potential duration and steady state Vma», a method analogous to the Bonferroni method, was used (Wallenstein et al., 1980). The probability value corresponding to the non-modified f-statistic for the difference between each pair of means was found to three significant figures by linear interpolation using logarithms of the standard two-tailed probability values (Rohlf and Sokal, 1969). A significance level of P < 0.05/m was used, where m = number of simultaneous comparisons. P values are reported together with their correction factor when derived from paired f-tests (e.g., P < 0.05/3). One-way analysis of variance was used to assess the significance of differences in recovery kinetics across the three drugs, since the data were obtained in separate cell populations. Scheffe's method was used to correct for the multiple pairwise comparisons among lidocaine and the two metabolites (Wallenstein et al., 1980). Experimental noise sometimes prevented reliable estimates of recovery kinetics being obtained. Linear regression techniques were used to eliminate from analysis experiments with unacceptable variance of the In b — diastolic interval relation [correlation coefficient <0.9, or regression coefficient not significant at the 1 % level (Snedecor and Cochran, 1967)]. Regression analysis was also used to assess the significance of any change in T,, since this reflected a change in regression coefficient. Here, we obtained the F ratio of the residual mean square variance when one slope, as opposed to two slopes, was fitted to the data (Snedecor and Cochran, 1967). Results Steady-State Action Potential Characteristics As expected at pH,, 7.4,15 nu lidocaine shortened action potential duration (P < 0.05/3; Table 1). However, resting potential and steady-state V^x remained closely similar to the lidocaine-free values at the stimulation rate of 1 Hz, consistent with previous reports (see Chen et al., 1975). Neither 15 tiM MEGX nor 30 MM GX had any effect on these three variables. No further changes were observed after doubling the dose of lidocaine (n = 6) and MEGX (n = 7) or quadrupling the dose of GX (n = 3). Reducing pHo to 6.95 increased action potential duration significantly, both under drug-free conditions and during exposure to lidocaine and MEGX (P < 0.01/3; Table 2). A similar increase with acidosis during exposure to GX approached, but did not reach, statistical significance (3P = 0.062). pH<, reduction produced a small decline in steady-state Vmax which was significant with lidocaine (—11%) and MEGX (-14%), but not under drug-free conditions or GX exposure (Table 2). pHo reduction also produced a small reduction in resting potential in the absence and presence of drug, but the change was statistically significant only when drug-free and drug results were pooled (1.4 mV, P < 0.01/3, n = 26). V max Reactivation Drug-Free Conditions At pHo 7.4, Vmax recovery was virtually complete (>98%) by the time membrane potential had repolarized to 1 mV from its resting value. The subsequent small residual recovery approached experimental noise. In 25 muscles, control time constants of Vmax reactivation were not calculable in 23 (<20 msec). In the remaining two muscles, the values were 26 and 36 msec. pHo reduction to 6.95 had little effect on reactivation kinetics (« = 8). Recovery may have been slightly prolonged (e.g., Fig. 1, panel TABLE 1 Effect of Lidocaine, MEGX, and GX on Action Potential Characteristics at 1 Hz in Guinea Pig Papillary Muscle RMP (mV) APD (msec) (V/sec) 11 85.8 ± 6 . 3 +0.3 238 ± 26 -9* 224 + 51 -3 Control MEGX (30 6 85.0 ± 1 .1 +1.0 197 ± 21 -2 285 + 44 -8 Control 5 82.9 ± 0 .6 -0.8 203 ± 27 +4 234 + 25 -16 Control Lidocaine (15 ,IM) GX (30 jiM]1 Results are mean ± SD in control solution, average change in absolute units with drug. RMP, resting membrane potential; APD, action potential duration until repolarization to 1 mV from RMP; Vouu, maximum upstroke velocity of action potential. * P < 0.05/3 for difference from control. 516 Circulation Research/Vol. 55, No. 4, October 1984 TABLE 2 Effect of Reducing Extracellular pH on Action Potential Characteristics at 1 Hz under Drug-Free Conditions and after Lidocaine, MEGX and GX RMP (mV) APD (msec) (V/sec) 8 85.6 ± 2.6 -1.1 208 ± 31 +19* 227 ± 28 -13 7.40 6.95 6 83.3 ± 2.5 -2.1 219 ± 20 +24 209 ± 39 -22* 7.40 6.95 6 82.9 + 4.5 -1.3 208 + 21 + 19* 262 + 38 7.40 6.95 6 82.7 ± 1.5 -0.9 195 + 25 +25 222 ± 51 -14 pH n Drug free 7.40 6.95 Lidocaine (15 HM) MEGX (30 ^M) GX (30 JJM) -36f Results are means ± SD at pH 7.40, average change in absolute units at pH 6.95. Abbreviations as in Table 1. * P < 0.01/3; t P < 0.05/3 for difference between the values at each pH. Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 3) but could not be quantified in five of eight muscles (Fig. 1, panels 1 and 2). MM (b0 = 0.43 ± 0.08, n = 12), MEGX 30 »M (b0 = 0.17 ± 0.03, n = 10), and then GX 30 m (b0 = 0.078 ± 0.019, n = 10). These differences were significant at the 1% level (one-way analysis of variance; Scheffe contrasts). As can be seen from Figure 2, unblocking following the train on average proceeded most rapidly with lidocaine (P < 0.05), then with GX, and least rapidly with MEGX (P < 0.01). An increase in dose of the three compounds increased b0 but did not alter the kinetics of Vmax reactivation (Fig. 3; Table 3). To determine how closely recovery from lidocaine block approximated Drug Exposure At pHo 7.4, Vmax recovery was delayed by exposure to both metabolites, as well as to lidocaine itself. There were marked differences among the three compounds in the level of Vmax block present at the beginning of diastole, and moderate differences in the subsequent time course of unblocking (Fig. 2). The order of potency for fractional V ^ block at zero diastolic interval (b0) was lidocaine 15 1.0 DRUG-FREE DRUG-FREE DRUG-FREE b D 8 O MUSCLE DEOl MUSCLE 15D O 0.01 -50 0 50 100 -50 0 50 100 -50 DIASTOLIC INTERVAL (ms) 0 50 100 FIGURE 1. Three individual examples of the time course of Vm*, reactivation under drug-free conditions at extracellular pH 7.4 (filled circles) and 6.95 (empty circles). Data are expressed as fractional Vmo reduction (b) in the "test" vs. "basic drive" action potential (1 Hz) as described in the legend to Figure 4. Data points falling prior to zero diastolic interval (see Methods) were excluded from analysis. The time constant of Vma reactivation (T,) was too short to be calculated from later points in muscles DEOl and 15D at either pH. T, was slightly prolonged by acidosis in muscle MG17. The lines through the data points in the right panel were fitted by the method of least squares from the regression of In b on diastolic interval. Broughton et a/./pH, Lipid Solubility, and Vmol Reactivation Block 1.0 LIDOCAINE I n Tr I39*26rm 12 MEGX 30^.M 232*34 10 GX 30/i.M 182t35 10 b o.i Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 0.01 0 250 500 DIASTOLIC INTERVAL (ms) FIGURE 2. Average time course of Vmal reactivation at pH0 7-4 during exposure to lidocaine, MEGX, or GX. The slope and elevation of each line are means of the slopes and elevations at zero diastolic interval (bo) obtained in individual muscles from the regression of In b on diastolic interval (see legend to Figure 4). Vertical bars on left show variance (±1 SD) around the mean b0 for each compound. a monoexponential decay, recovery kinetics were determined particularly in an additional 18 muscles. The Vmax measurements at each coupling interval were averaged over five replications to minimize variance from experimental noise. The relationship between In b and time was linear in all cases, with the correlation coefficient averaging 0.990 (range 0.942-0.999) in the 18 experiments. Thus, the decay in Vmax block appeared monoexponential (Fig. 4). 517 Reduction in pHo to 6.95 markedly delayed the recovery from lidocaine block, as expected (Figs. 5 and 6). The kinetics of recovery from MEGX block were also slowed significantly (P < 0.01), but to a lesser extent (P < 0.05). By contrast, recovery from GX block was not significantly affected by pH<, reduction (Figs. 5 and 6). The increase in recovery time constant produced by acidosis averaged 73 ± 28% with lidocaine (P < 0.01; n = 6), 42 ± 15% with MEGX (P < 0.01; n = 9), but only 13 ± 17% with GX (P > 0.4; n = 7). The change in recovery kinetics in each individual muscle was tested by linear regression analysis. The change in slope of the linear relationship between In b and diastolic interval was significant in all six muscles exposed to lidocaine (P < 0.001 in each), in eight of nine muscles exposed to MEGX (P < 0.025 or better), but in only one of seven musles exposed to GX (P < 0.05 in this muscle). Acidosis also reduced b 0 due to MEGX (from 0.17 ± 0.036 to 0.121 ± 0.028, P < 0.01). No comparable effect was observed with lidocaine or GX (Fig. 6). Octanol:H2O Partitioning Considerable differences in lipid solubility of the neutral form were suggested by the partitioning differences among the three compounds in vitro at pH = pKa +2. Lidocaine was the most lipid soluble. P, the ratio of octanol:H2O concentrations after partitioning, was 249 ± 60 (« = 4). MEGX was next most lipid soluble, with the ratio of octanol:H2O concentrations averaging 21.2 ± 4.3 (n = 3). GX was the least lipid soluble (P = 2.56 ± 0.3, n = 3). Biological activity has been found to vary with log lipid solubility (Hansch and Leo, 1979; Courtney, 1980). The differences in log P are shown in Table 4. The value for lidocaine is almost twice that of MEGX and almost six times that of GX. Partitioning under conditions pH = pKa — 2 excluded measurable GX MEGX LIDOCAINE Tr "o 120/i.M. U 5 r m .14 .077 3 0 F M . 159 120flM 30/iM MUSCLE AGI5 0 250 500 0 250 500 0 DIASTOLIC INTERVAL (ms) 250 500 FIGURE 3. Individual examples of Vma reactivation during exposure to two different concentrations of lidocaine, MEGX, or GX. Methods and abbreviations as in legend to Figure 4, except that data points in the left and middle panels represent one test action potential at each diastolic interval, not the mean of five replications. Circulation Research/Vol. 55, No. 4, October 1984 518 TABLE 3 Recovery Kinetics from V^, Block at Two Doses of Lidocaine, MEGX, and GX in Guinea Pig Papillary Muscle at 1 Hz Lower dose Higher dose T, Lidocaine (15 and 30 MM) MEGX (15 and 30 MM) GX (30 and 120 MM) 6 5 3 b0 (msec) b0 (msec) 0.385 + 0.024 0.106 ±0.014 0.065 ± 0.010 143 ± 32 228 ± 45 180 ± 28 0.534 ± 0.058 0.182 + 0.027 0.145 ± 0.032 146 ± 27 226 + 45 175 ± 28 Data are means ± SD; b0, fractional Vmsx block at the onset of diastole; T,, time constant for decay of V™ block. lipid solubility of the charged (protonated) form of lidocaine, MEGX, and GX. Discussion Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 In the doses examined, neither lidocaine nor its desethylated metabolites, MEGX and GX, depressed phase 0 Vmax of the 1 Hz basic drive action potentials. However, test impulses detected significant Vmax block in early diastole following a 1 Hz train in the 1.0 r LIDOCAINE 15/iM r = 0.999 slope = 0.0064910.000085 T> = 154 ms |P<0.001) b MUSCLE J22 \ DRUG FREE Q X, 36 mj 0.01 LA 0 250 500 DIASTOLIC INTERVAL (ms) FIGURE 4. An individual example of lidocaine's effect on the time course of Vm^ reactivation in guinea pig papillary muscle at pH0 7.4. Reactivation was assessed by varying the coupling interval of a single "test" action potential following a 1 Hz train. Data show the timedependent decay in fractional Vma block (b), where b = [Vmax (1 Hz train) — Vma (test)]/]/^ (1 Hz train). Each data point is the average of five replications. The lines through the data points were fitted by the method of least squares from the regression of In b on diastolic interval. The correlation coefficient (r) shows the data is well fitted by a straight line. Calculated b at zero diastolic interval (bo) was 0.52 in this muscle. The significance of the slope value (regression coefficient) was obtained from "t" = the ratio of slope to its standard deviation (degrees of freedom n-2; Snedecor and Cochran, 1967). The time constant of Vmia reactivation (rr) is the inverse slope. presence of each of the three compounds. At equimolar concentration, the initial diastolic block (b0) was most intense with lidocaine, of lesser intensity with MEGX, and least with GX. At 30 /IM, b 0 averaged 0.53 with lidocaine (Table 3), 0.17-0.18 with MEGX (Fig. 2; Table 3), but only 0.07-0.08 with GX (Fig. 2; Table 3). These differences roughly paralleled the relative lipid solubilities of the three compounds, which presumably determined the membrane concentration of neutral anesthetic molecules adjacent to sodium channels (relative log P 1.0:0.55:0.17, for lidocaine, MEGX, and GX, respectively). It would be necessary to obtain full doseresponse curves to determine how closely potency for early diastolic block is a function of lipid solubility as assessed from octanol:H2O partitioning. All three compounds slowed the kinetics of Vmax reactivation. Significant differences were observed in the rate of diastolic decay of Vmax block. At pHo 7.4, lidocaine block dissipated most rapidly (time constant r r 139 msec), followed by GX (rr 182 msec), whereas MEGX unblocked most slowly (rr 232 msec) (Fig. 2). These differences were not a consequence of the potency differences for b0 block. Reactivation kinetics were shown to be dose (and hence b0) independent for the three compounds over the range of b 0 values from 0.08 to 0.53 (see Fig. 3 and Table 3). The question then arises whether the differences in Vmax reactivation can be taken to indicate comparable differences in the rates of sodium channel unblocking among the three compounds. Although a close correlation between Vmax and peak inward sodium (INa) current is expected in cardiac muscle on theoretical grounds, whether Vmax is a reliable index of available sodium conductance (gNa) is controversial (Cohen and Strichartz, 1977; Hondeghem, 1978; Strichartz and Cohen, 1978; Walton and Fozzard, 1979; Cohen et al., 1981; Bean et al., 1982). Bean et al. (1982) have recently reported that, despite the precaution of constant latency, Vmax appeared to be a nonlinear index of gNa changes with tetrodotoxin in voltage clamp experiments. A similar nonlinear relationship between Vmax and gNa was obtained when the number of sodium channels available to open during a sudden depolarization was varied by using different holding potentials to Broughton et al./pH, Lipid Solubility, and Vm<lr Reactivation Block 10 r LIDOCAINE 15>iM f 519 GX 30/iM MEGX 30/iM pH Tr 6.95 7.4 235 mi 163 pH .12 .15 6.95 7.4 T, 162« 130 bo .086 .093 b 0.1 MUSCLE DEOI 0.01 500 0 250 250 500 0 DIASTOLIC INTERVAL (ms) 500 250 Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 FIGURE 5. Individual examples of the effect of extracellular pH reduction on Vma reactivation during exposure to lidocaine, MEGX, or GX. Abbreviations and method for determining recovery kinetics as in legend to Figure 4, except that data points in the left panel represent one test action potential at each diastolic interval, not the mean of five replications. change inactivation (Cohen et al., 1984). An important consequence predicted from their study was that the time course of reactivation measured by Vmax will be distorted and nonexponential (curvilinear) when the underlying recovery of gNa is exponential. In the present study at 37°C, we did not observe curvilinear Vmax reactivation. The kinetics we obtained closely approached monoexponential decay except for a slight deviation at the shortest coupling intervals consistent with recovery of drugfree channels (Fig. 4). Clarification of the discrepancy between the two methods is impeded by the current difficulty of obtaining reliable measurements of sodium current in heart under the same conditions of physiological sodium concentration, membrane potential and temperature at which Vmax measurements are obtained. 1.0 LIDOCAINE 15^M(n=6) Effects of pH, Reduction The kinetics of recovery from lidocaine block of Vmax was markedly slowed by extracellular acidosis, MEGX 30/iM(n = 9 pH T, I 6.95 231J26mi .47*07 7.4 !36t20 .47t.O9 b Nonetheless, Vmax provides an indirect measure of sodium conductance which must be interpreted with great caution. Linear kinetics of Vmax reactivation are a necessary but not sufficient feature ensuring proportionality with gNa reactivation. Complex interactions of activation and inactivation gating processes producing an apparently pure semilogarithmic decay but with an incorrect slope cannot be excluded (see Bean et al., 1982). However the b 0 independence of Vmax reactivation probably ensures that directional changes in the time course of sodium channel reactivation is reliably indicated. pH Tr 6.95 3l4*57n» I2J.O3 7.4 22U27 .I7S.04 GX 30/xM (n = 7) pH T, 6.95 2 0 I * } 4 I « I .078! 033 7.4 185:43 .084!.019 PH6.95 pH7.4 0.01 0 250 500 0 250 500 0 DIASTOLIC INTERVAL . ms 250 500 FIGURE 6. Average time course of V^ reactivation at pHo 7.4 and 6.95 during exposure to lidocaine, MEGX, or GX. The slope and elevation of each line are the means of the slopes and elevations at zero diastolic interval (bo) obtained in individual muscles from the regression of In b on diastolic interval (see legend to Figure 4). 520 Circulation Research/Vol. 55, No. 4, October 1984 TABLE 4 Physicochemical Properties of Lidocaine, MEGX, and GX [Neutral]/[protonated] Lidocaine MEGX GX Molecular wt 234 206 178 pK. pH.7.4 pH, 6.95 logP* 7.86t 8.04J 7.68J 0.35 0.23 0.53 0.12 0.081 0.19 2.39 ± 0.20 (n = 4) 1.32 ± 0.09 (« = 3) 0.41 ± 0.06 (n = 3) * Octanol:H2O partition coefficient at pH = pK« + 2; five replicates each estimation, t Truant and Takman, 1969; J Johansson, 1982. Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 as previously reported by Grant et al. (1980). Interestingly, recovery from MEGX block was less affected, and recovery from GX block almost completely unaffected, by moderate pH,, reduction. Current theories attribute the exponential recovery of sodium conductance between action potentials to drug exiting from sodium channels (Strichartz, 1973; Courtney, 1975; Hille, 1977, 1978; Hondeghem and Katzung, 1977). Hydrophobic neutral drug molecules are thought to return rapidly to the membrane phase once transmembrane potential no longer favors channel occupancy; the lipid-insoluble charged form must exit via the hydrophilic channel inner mouth unless it loses its charge (Hille, 1977). Channel-gating configuration in diastole is thought to impede escape of the charged species from the blocking position, although other explanations for slow unblocking kinetics have not been excluded. Reduction in pHo is thought to favor protonation of drug molecules within the channel to an extent dependent on drug pKa. Lidocaine, MEGX, and GX are weak bases with pKa 7.86, 8.04, and 7.68, respectively. The protonated form predominates at low pH o . However, in the present study, the alteration in recovery kinetics with pHo reduction did not correlate with the calculated change in ratio of neutral to protonated form (Table 4). Indeed, the calculated change was greatest with GX, which showed little or no potentiation at all. This apparent contradiction is resolved if an important role is proposed for lipid solubility in determining the unblocking rate of the neutral form (Hille, 1977; Courtney, 1980). Thus, an increase in protonated:neutral form should especially prolong recovery kinetics of a highly lipid soluble compound like lidocaine, which could readily exit via the membrane phase at normal pH. By contrast, lipid-insoluble GX unblocked relatively slowly whether protonated or not. MEGX with intermediate lipid solubility of the neutral form showed intermediate pH potentiation as far as kinetics of unblocking are concerned. The question arises as to whether the marked slowing of lidocaine unblocking that we observed can reasonably be attributed to the modest reduction in ratio of neutral:protonated form produced with reduction in pHo to 6.95. To clarify this question, we examined two simple kinetic alternatives. The binding of neutral and protonated drug (Dn,Dc) to a drug-free channel (U) to form a blocked channel (Bn,Bc) was restricted to the duration of the action potential and was assumed to be negligibly slow at the present micromolar concentrations once repolarization was complete. Scheme 1 (uncoupled) U + Dc ^ Bc U + Dn Scheme 2 (coupled) U Bn Dc ^ Bc U + Dn ^ Bn where k is a composite rate constant term describing drug association during diastole which combines rate contants for binding, diffusion, field effect, and drug concentration; / is a composite rate constant term describing drug dissociation during diastole which combines rate constants for binding, diffusion, and field effect; and where /„ » kn and 4 ^> kc in schemes 1 and 2 during diastole (Strauss et al., in press). Fractional block at the onset of diastole (b0) equaled the sum of block due to both neutral and charged species (bn + bc). In scheme 1, the fraction of charged and neutrally blocked channels (bn and bc) decay as independent processes. In other words, there is no conversion of Bc to Bn, governed by pH o . In scheme 2, interconversion between charged and neutrally blocked channels is permitted to maintain the value of R (bn/bc) constant throughout the decay in total Vmax block. We assume here that ambient pH and drug pKa within a blocked channel are the same as for drug in extracellular solution, so that R = b n /b c = IOP^-P"*. The coupled scheme was thought more realistic in view of the known access of extracellular protons to the channel-binding site (Schwarz et al., 1977) and the high speed of proton transfer reactions (Bell, 1973). As can be seen from Figure 7, scheme 1 is unlikely to account for the pH potentiation we observed with lidocaine. Time constants for the exponential decay of neutral and protonated species block (r n , TC) were assumed to be 50 and 500 msec, respectively. The decay in total block is biexponential with an early rapid phase due to Broughton et fl/./pH, Lipid Solubility, and V™, Reactivation Block 1.0 AGGREGATE DECAYS pH: 7.4 6.95 b 0.1 Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 0.01 0 250 500 DIASTOLIC INTERVAL (ms) FIGURE 7. Simulated effect of extracellular pH reduction on Vmol reactivation according to kinetic scheme 1 (see Discussion). It is assumed that recovery from Vmal block due to protonated lidocaine (LH+) and recovery from block due to neutral lidocaine (L) occur as two independent monoexponential decays with time constants 500 and 50 msec, respectively. At zero diastolic interval, bn:bc, the ratio of block due to L and block due to LH+, is assumed to equal the ratio [L]:[LH+] in the extracellular fluid. That is, bjbc = W"''1"^. The curvilinear aggregate decay in total b from a b0 value of 0.5 at each pH was found by addition of the linear decays of bn and bc. recovery from neutral species block and a subsequent slow phase due to recovery from protonated species block. Our lidocaine data were much better fit by scheme 2 which, for r n <3C TC, as above, implies that a significant proportion of the decay in bc involves a hydrophobic pathway of drug egress as molecules lose their charge and exit via the membrane phase. For scheme 2, where b n /b c remains constant throughout diastole, bn = Rb/(1 + R) and bc = b/(l + R). If /„ and fc are rate constants for decay of b n and b c , respectively, then: 521 rate constants for neutral and charged forms of lidocaine correspond to r n and TC values of 44 and 483 msec, respectively, at the resting potential of the present experiments (—82 mV). The predicted relationship between r r and R from Equation 2, assuming the above values for /„ and fc for lidocaine, is shown in Figure 8. It can be seen that recovery kinetics of V^,* block approaches the TC value as R decreases, particularly once R is less than 0.3. This would correspond to pHo at least 0.5 U below pKa. Schwarz et al. (1977) observed even more steep pH dependence of recovery from lidocaine block of INa in frog skeletal muscle at 12.5°C. For MEGX, the r n and TC values were 70 and 439 msec, respectively. For GX, r n was 144 msec and TC was 217 msec. The simplest interpretation of these differences is that rn decreases as lipid solubility increases, whereas r c decreases with molecular weight. However, the relation between physicochemical properties and kinetics of drug action is complex (Campbell, 1983), and it has yet to be demonstrated that extrapolation of these conclusions beyond this small series of related low molecular weight compounds is valid. The analysis predicts unexpectedly fast recovery kinetics for the protonated tertiary amine species in view of results obtained with permanently charged quaternary compounds (Gintant et al., 1983). The discrepancy may reflect steric hindrance from the more bulky amine region of the quaternary molecule. Bean et al. (1983) recently published data on the time course of sodium current reactivation in rabbit Purkinje fiber exposed to lidocaine under voltage clamp at pHo 7.0 500 400 300 AGGREGATE (ms) 200 - db/dt = -/ n Rb/(l + R) - / c b/(l + R) Thus b(t) = b 0 exp - (/nR R) (1) Thus, reactivation should be monoexponential with the time constant for decay in total V ^ block (rr) given by R)/(/nR (2) Knowing our experimental values for r r at pH, 7.4 and 6.95, and calculating R, Equation 2 can be solved for / n and 4 giving values of 2.25 X 10"2 and 2.07 x 10~3 msec"1, respectively. These dissociation (RATIO OF NEUTRAL TO CHARGED DRUG) FIGURE 8. Predicted relationship between the time constant of Vmla reactivation (aggregate T,) and the ratio of neutral to protonated lidocaine, MEGX or GX during changes in extracellular pH, according to kinetic scheme 2 (see Discussion). It is assumed that bn:bc, the ratio of Vm4t block due to neutral drug-.block due to protonated drug within sodium channels, remains identical to the value ofR, the ratio [neutral drug]:[protonated drug] in the extracellular fluid, throughout the decay in total b. R= 10'"'''*: 522 and 8.1. Application of our kinetic analysis to their data also predicts relatively rapid unblocking of the protonated form of lidocaine (TC 1000 msec), but leads to a surprisingly large value for the time constant of the lipid-soluble neutral form of the molecule (r n 342 msec). This may reflect maintenance of their preparation at a temperature below the point of phase transition of membrane lipids. Further studies are required to validate the relationship between the aggregate r r and R over a wider range of R, as the estimates of dissociation rate constants for the charged and neutral forms of the compounds are sensitive to the accuracy with which the decrease in Vmax measures sodium channel block. Additional studies are also needed to confirm the importance of lipid solubility for pH potentiation of local anesthetic block. Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 Clinical Implications Serum levels of MEGX and GX approaching or exceeding 20 JIM have been reported in human subjects receiving lidocaine infusion. Previous experimental studies suggest that this MEGX concentration would produce some antiarrhythmic effect. MEGX was reported to have about one-third the equimolar potency of lidocaine for antifibrillatory action in chloroform-exposed mice, one-half the potency for premature ventricular contraction suppression in dogs after coronary ligation, full potency for suppression of ouabain-toxic atrial arrhythmias in guinea pigs, and one-fourth the potency for block of frog sciatic nerve (Ehrenberg, 1948; Smith and Duce, 1971; Burney et al., 1974). In comparison, we found that the level of Vmax block immediately after action potential repolarization was one-third of the block with lidocaine at 30 tiu concentration, similar to the reported potency ratios for nerve block and suppression of ventricular arrythmia. In addition, the kinetics of recovery from MEGX block was prolonged somewhat by acidosis, which may promote suppression of arrhythmia in ischemic myocardium. GX was reported one-fourth as potent as lidocaine in a model of ventricular arrhythmia (Tenthorey et al., 1981), but failed to suppress ouabain-toxic atrial arrhythmias (Burney et al., 1974). The present study suggests that its antiarrhythmic action probably is minimal at clinically observed blood levels in patients with ischemic ventricular arrhythmias, since Vmax block at the onset of diastole was less than onesixth that seen with lidocaine, and recovery from block was not delayed by acidosis. The work could not have been carried out without the generous support of Dr. J.C Greenfield, Jr. We are grateful to Astra Pharmaceutical Products, Inc., Worcester, MA for supplies of lidocaine, MEGX, and GX. Mali Hutchison rendered invaluable technical expertise. Supported by National Institutes of Health Grants 19216 and 17670. Part of the work was carried out while Dr. Broughton was an Overseas Research Fellow of the National Heart Foundation of Australia. Circulation Research/Vol. 55, No. 4, October 1984 Dr. Broughton's present address: Baker Medical Research Institute, Commercial Road, Prahran, Victoria, Australia 3181. Address for reprints: Harold C Strauss M.D., Box 3845, Duke University Medical Center, Durham, North Carolina 27710. Received October 31, 1983; accepted for publication August 2, 1984. References Allen DJ, Brennan FJ, Wit AL (1978) Actions of lidocaine on transmembrane potentials of subendocardial Purkinje fibers surviving in infarcted canine hearts. Circ Res 43: 470-481 Bean BP, Cohen CJ, Tsien RW (1982) Block of cardiac sodium channels by tetrodotoxin and lidocaine: Sodium current and Vm.* experiments. In Normal and Abnormal Conduction in the Heart, edited by A Paes de Carvalho, BF Hoffman, M Lieberman. Mount Kisco, Futura, pp 189-209 Bean BP, Cohen CJ, Tsien RW (1983) Lidocaine block of sodium channels. J Gen Physiol 81: 613-642 Bell RP (1973) The Proton in Chemistry, ed 2. Ithaca, Cornell University Press Blumer J, Strong JM, Atkinson AJ (1973) The convulsant potency of lidocaine and its A/-dealkylated metabolites. J Pharmacol Exp Ther 186: 31-36 Burney RG, DiFazio CA, Peach MJ, Petrie KA, Silvester MJ (1974) Antiarrhythmic effects of lidocaine metabolites. Am Heart J 88: 765-769 Campbell TJ (1983) Importance of physico-chemical properties in determining the kinetics of the effects of class I antiarrhythmic drugs on maximum rate of depolarization in guinea-pig ventricle. Br J Pharmacol 80: 33-40 Cardinal R, Janse MJ, van Eeden I, Werner G, d'Alnoncourt C, Durrer D (1981) The effects of lidocaine on intracellular and extracellular potentials, activation, and ventricular arrhythmias during acute regional ischemia in the isolated porcine heart. Circ Res 49: 792-806 Chen C, Gettes LS, Katzung BG (1975) Effect of lidocaine and quinidine on steady-state characteristics and recovery kinetics of (dV/dt)™,, in guinea pig ventricular myocardium. Circ Res 37: 20-29 Cohen CJ, Bean BP, Tsien, RW (1984) Maximal upstroke velocity as an index of available sodium conductance: Comparison of maximal upstroke velocity and voltage clamp measurements of sodium current in rabbit Purkinje fibers. Circ Res 54: 636-651 Cohen I, Attwell D, Strichartz G (1981) The dependence of the maximum rate of rise of the action potential upstroke on membrane properties. Proc R Soc Lond [Biol] 214: 85-98 Cohen IS, Strichartz GR (1977) On the voltage-dependent action of tetrodotoxin. Biophys J17: 275-279 Courtney KR (1975) Mechanism of frequency-dependent inhibition of sodium currents in frog myelinated nerve by the lidocaine derivative GEA 968. J Pharmacol Exp Ther 195: 225-236 Courtney KR (1980) Structure-activity relations for frequencydependent sodium channel block in nerve by local anesthetics. J Pharmacol Exp Ther 213: 114-119 Ehrenberg L (1948) The time-concentration curve of local anesthetics. Acta Chem Scand 2: 64-80 Gintant GA, Hoffman BF, Naylor RE (1983) The influence of molecular form of local anesthetic-type antiarrhythmic agents on reduction of the maximum upstroke velocity of canine cardiac Purkinje fibers. Circ Res 52: 735-746 Grant AO, Strauss LJ, Wallace AG, Strauss HC (1980) The influence of pH on the electrophysiological effects of lidocaine in guinea pig ventricular myocardium. Circ Res 47: 542-550 Halkin H, Meffin P, Melmon KL, Rowland M (1975) Influence of congestive heart failure on blood levels of lidocaine and its active monodeethylated metabolite. Clin Pharmacol Ther 17: 669-676 Handel F, Luzzi FA, Wenger TL, Barchowsky A, Shand DG, Strauss HC (1983) Lidocaine and its metabolites in canine plasma and myocardium. J Cardiovasc Pharmacol 5: 44-50 Hansch C, Leo A (1979) Substituent constants for correlation in chemistry and biology. New York, Wiley-Interscience Broughton et fl/./pH, Lipid Solubility, and Vmax Reactivation Block Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 Hille B (1977) Local anesthetics: Hydiophilic and hydrophobic pathways for the drug-receptor reaction. J Gen Physiol 69:497515 Hille B (1978) Local anesthetic action on inactivation of the Na channel in nerve and skeletal muscle: Possible mechanisms for antiarrhythmic agents. In Biophysical Aspects of Cardiac Muscle, edited by M Morad. New York, Academic Press, pp 55-74 Hondeghem LM (1976) Effects of lidocaine, phenytoin and quinidine on the ischemic canine myocardium. J Electrocardiol 9: 203-209 Hondeghem LM (1978) Validity of V,™, as a measure of the sodium current in cardiac and nervous tissue. Biophys ] 23: 147-152 Hondeghem LM, Katzung BG (1977) Time and voltage dependent interaction of antiarrhythmic drugs with cardiac sodium channels. Biochim Biophys Acta 472: 373-398 Johansson P (1982) liquid-liquid distribution of lidocaine and some structurally related anti-arrhythmic drugs and local anesthetics. Acta Pharm Suec 19: 137-142 Khodorov B, Shiskhova L, Peganov E, Revenko S (1976) Inhibition of sodium currents in frog Ranvier node treated with local anesthetics. Role of slow sodium inactivation. Biochim Biophys Acta 433: 409-435 Kupersmith J, Antman EM, Hoffman BF (1975) In vivo electrophysiological effects of lidocaine in canine acute myocardial infarction. Circ Res 36: 84-91 Lazzara R, Hope RR, El-Sherif N, Scherlag BJ (1978) Effects of lidocaine in hypoxic and ischemic cardiac cells. Am J Cardiol 41: 872-879 Reuter H, Scholz H (1968) Uber den einfluS der extracellularen Ca-Konzentration auf membranpotential und kontraktion isolierter herzpraparate bei graduierter depolarisation. Pflugers Arch 300: 87-107 Rohlf FJ, Sokal RR (1969) Statistical Tables. San Francisco, WH Freeman, p 159 Schwarz W, Palade PT, Hille B (1977) Local anesthetics: Effects 523 of pH on use-dependent block of sodium channels in frog muscle. Biophys J 20: 343-368 Smith ER, Duce BR (1971) The acute antiarrhythmic and toxic effects in mice and dogs of 2-ethylamino-2,6-acetoxylidine (L86), a metabolite of lidocaine. ] Pharmacol Exp Ther 179: 580585 Snedecor GW, Cochran WG (1967) Statistical Methods. Ames, Iowa, Iowa State University Press Spitzer KW, Hogan PM (1979) The effects of acidosis and bicarbonate on action potential repolarization in canine cardiac Purkinje fibers. J Gen Physiol 73: 199-218 Strauss HC, Broughton A, Starmer CF, Grant AO (in press) pH potentiation of local anesthetic action in heart muscle. In Cardiac Electrophysiology and Arrhythmias edited by DP Zipes, J Jalife. Orlando, Grune & Stratton, Strichartz GR (1973) The inhibition of sodium currents in myelinated nerve by quaternary derivatives of lidocaine. ] Gen Physiol 62: 37-57 Strong JM, Parker M, Atkinson AJ (1973) Identification of glycinexylidide in patients treated with intravenous lidocaine. Clin Pharmacol Ther 14: 67-72 Tenthorey PA, Block AJ, Ronfeld RA, McMaster PD, Byrnes EW (1981) New antiarrhythmic agents. 6 Quantitative structureactivity relationships of aminoxylidides. J Med Chem 24: 798806 Truant AP, Takman B (1959) Differential physical-chemical and neuropharmacologic properties of local anesthetic agents. Anesth Analg (Paris) 38: 478-484 Wallenstein S, Zucker CL, Fleiss JL (1980) Some statistical methods useful in circulation research. Circ Res 47: 1-9 Walton M, Fozzard HA (1979) The relation of V,™ to IN,, to GN., and h«, in a model of the cardiac Purkinje fiber. Biophys J 25: 407-420 INDEX TERMS: Lidocaine metabolites • block • V~,, reactivation kinetics • Acidosis Local anesthetic Lipid solubility modulates pH potentiation of local anesthetic block of Vmax reactivation in guinea pig myocardium. A Broughton, A O Grant, C F Starmer, J K Klinger, B S Stambler and H C Strauss Downloaded from http://circres.ahajournals.org/ by guest on April 29, 2017 Circ Res. 1984;55:513-523 doi: 10.1161/01.RES.55.4.513 Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1984 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7330. Online ISSN: 1524-4571 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circres.ahajournals.org/content/55/4/513 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation Research is online at: http://circres.ahajournals.org//subscriptions/