* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 1400_Milligan_GF5E3
Pharmaceutical industry wikipedia , lookup
Electronic prescribing wikipedia , lookup
Toxicodynamics wikipedia , lookup
Compounding wikipedia , lookup
Theralizumab wikipedia , lookup
Neuropharmacology wikipedia , lookup
Plateau principle wikipedia , lookup
History of general anesthesia wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacokinetics wikipedia , lookup
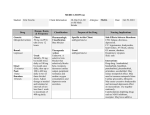
TUMESCENT ANESTHESIA: Best Practice Protocols Elizabeth Milligan RN, RPhS Macon, GA NO DISCLOSURES Emersion and Knowledge • Dr. Jeffrey Klein’s book Tumescent Technique • Hands-on Tumescent Training • Familiarity with ultrasound (For Endovenous procedure) BEST OF THE BEST PROPER TRAINING and PROTOCOLS • Safety • Clinical pharmacokinetics and pharmacology • Technique • Adverse events • Empathy Safety • • • • Safer Sharps, Neutral Zone Avoid IV infusion Prevent Mixing and Dosage Errors Standard Formula: 1gm Lidocaine + 1mg Epi 100ml 10mEqNa+Bicarb10ml 0.9% Physiologic Saline 1000ml 1gm/1110ml = 0.09% Safety - Mixing Standard Formulas Posted Towel = Do NOT Disturb Clean workspace, Blunt Tip needles Safety - Dosage FDA Lidocaine Labeling: 7mg/kg outof-the bottle commercial • Based on 1948 Obstetric Epidural Data • FDA Has No Data on Subcutaneous Infiltration http://tumescent.org/wp-content/uploads/Anesth-Analg-2016-Klein.pdf Safety - Dosage Dr Klein: • Maximum safe dosage TLA 28 mg/kg (non-lipo cases) • Peak Plasma lidocaine level with TLA = 12 hours • Added liposuction reduces peak plasma lidocaine levels by approx. 10 -30% • Peak Plasma lidocaine concentration should NOT exceed 5 ųg/ml http://tumescent.org/wp-content/uploads/Anesth-Analg-2016-Klein.pdf Safety -Drug Interactions • Nurse Counseling • Drug Interactions • Bleeding Risk • Lidocaine Metabolism • Prescribing • Antibiotic • Benzodiazepine – Lorazepam vs Diazepam • Clonidine Protocols- NO VARIATION • Clear Staff Roles • Clear Physician Written Order • TEAM commitment to safe Dosage • Surgical Time out • Continued monitoring Protocols- NO VARIATION • Forms and Record keeping • Calculating Dosage and Limitations based on weight • Document volume and dosage administered Protocols- NO VARIATION • Forms and Record keeping • Labeling • Keep bottles used for mixing until next day Adverse Events – Vasovagal Syncope • Vasovagal Syncope • Failure of physiologic mechanisms responsible or maintain both blood pressure and cerebral blood flow – Dr Klein • Need response protocol • Preventive measures for syncope • Know ahead of time if patient is prone to fainting • Patient should NOT watch - Keep head bed down • Eat before appointment Adverse Events – Anaphylaxis • Develop Emergency Response Protocols Adverse Events – Lorazepam Toxicity • Sign: decreased respiration, decreased pulse rate, decreased blood pressure, decreased O2 sat, difficult to arouse. • Action: • Flumazenil 0.2 mg IV push for 15 seconds every minute for 1-5 doses • Repeat that sequence in 20 min if needed Adverse Events – Lidocaine Toxicity • Signs: drowsiness, lightheadedness, nausea, vomiting, nervousness, apprehension, euphoria, confusion, dizziness, blurred/double vision, tremors • Action: • ER visit to have plasma level checked and possibly stay overnight for observation (5 ųg/ml threshold) • Beware of mimic Adverse Events – Advanced Lidocaine Toxicity • Signs: Dysrhythmia or seizures • Action: • Call 911. • Start O2 • Alert EMS of the following medication recommendations: • Bretylium (for dysrhythmia) • Midazolam (for seizures): 5-7mg bolus, then 1-2 mg until controlled. • Let EMS know not to use Diazepam Adverse Events – Slow Lidocaine Absorption • Signs: Toxicity occurring about 12 hrs after tumescent administration, usually after waking up from a nap. • Usually it will resolve in about 1-2 hours Action: • • • • • Drink water Sit slightly reclined (like watching tv) Breathe in a paper bag Staff call patient every 30 minutes If occurs after 12 hours and /or the symptoms worsen /are severe - go to the ER or call 911 Adverse Events – Beware of the Mimic • Mimicking behaviors of Lidocaine Toxicity • Benzodiazepine toxicity • Self-medicating (sedation drug, narcotic, alcohol) Action (if mild): • Monitor patient (or call every hour if patient at home) until symptoms improve • Drink fluids • Relax • IF worsens, or severe, ER examination OUTSIDE THE BOX • Allergy to Lidocaine • Drug challenge with allergist • Prilocaine (citanest) • Preservative Free Solution • Histamine Reaction • Pre-treat with anti-histamine and H2 blocker • Preservative Free Solution • Epinephrine Sensitivity • • • • Slow infusion, avoid IV injection Education Preservative Free Solution Epinephrine is responsible for the profound vasoconstriction and consequent hemostasis essential to the tumescent technique – Dr Klein Histamine Reaction Action • No suture strips used • Oral Anti-histamine and H2 blocker • Allergist drug challenge • Prilocaine, preservative free solution, for subsequent procedures Initial Picture 7 days postprocedure 6 weeks postprocedure OUTSIDE THE BOX • Liver Disease • Lidocaine metabolized in liver, • Rate of metabolism dependent on rate of blood flow to the liver • Conditions that may cause compromised metabolism : • Shock, Congestive heart failure, Beta-blockers, Cirrhosis • Kidney Disease • Lidocaine clearance normal • Use caution regarding fluid overload Empathy • Anxiety heightens pain • Anxiolysis • Verbal Anesthesia • Warm solution • Music • Relaxation APP • Target less tender sites for initial numbing • Patience and Gentleness Prevention of complication is key: • Training • Witten Policy and procedure • Accurate record keeping • Written orders for TLA • Double check dosage calculations • Properly trained staff References Klein, Jeffrey A. (2000). Tumescent Technique , Tumescent Anesthesia & Microcannular Liposuction. St. Louis, Missouri: Mosby, Inc. Klein, Jeffrey A. (2016). Tumescent Drug Delivery: Lidocaine and Beyond. [Power Point Slides]. Retrieved from: http://tumescent.org/TLA-AAD-2016.pdf Klein, Jeffrey A. Collection of Articles: http://tumescent.org/tumescent-anesthesia-articles/ Klein, Jeffrey A. & Jeske, Daniel R. (2016). Estimated Maximal Safe Dosages of Tumescent Lidocaine. International Anesthesia Research Society. DOI: 10.1213/ANE.0000000000001119. www.anesthesia-analgesia.org May 2016 • Volume 122 • Number 5. Retrieved from http://tumescent.org/wp-content/uploads/Anesth-Analg2016-Klein.pdf Klein, Jeffrey A. (1990). Tumescent Technique for Regional Anesthesia Permits Lidocaine Doses of 35 mg/kg for Liposuction. J. Dermatol Surg Oncol 1990; 16:248-263. Retrieved from http://tumescent.org/tumescenttechnique-for-regional-anesthesia-permits-lidocaine-doses-of-35-mgkg-for-liposuction/ THANK YOU! [email protected]