* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Comparison of symptom response following advice for a diet low in
Survey
Document related concepts
Transcript
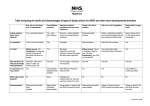
Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome H. M. Staudacher, K. Whelan, P. M. Irving & M. C. E. Lomer Presented by Victoria Scholl Irritable Bowel Syndrome Most common gastrointestinal condition Most commonly diagnosed in women and patients under 50 Assessment based on Rome III criteria/NICE Criteria No biochemical, histopathological or radiological diagnostic test for IBS exists Symptoms include: constipation, diarrhea, abdominal pain and distention. IBS The condition usually causes long-term symptoms May occur in episodes. Symptoms vary and may be meal-related. Symptoms interfere with daily life and social functioning in many patients. Symptoms sometimes seem to develop as a consequence of a severe intestinal infection or to be precipitated by major life events, or in a period of considerable stress. Pathogenesis IBS patients present with GI complaints which physicians can find no organic cause Brain-gut interaction Heritability/Genetics Dietary and intestinal flora Abnormalities in neuroendocrine system of the gut Management of IBS Pharmacotherapy: No drug fits all Antispasmodics Antidepressants Anti diarrhea agents Antibiotics Alternative Therapies Aloe Peppermint oil probiotics Fiber IBS-D IBS-C Why research on IBS is important Quality of life Current health care costs to manage IBS Ability to cope with symptoms more effectively Research into dietary management of symptoms is promising FODMAPs Stands for: Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. These are short chain carbohydrates that are poorly absorbed in the small intestine This malabsorption is common to everyone however, with altered gut flora, motility disorders, and hypersensitivity in IBS, the outcome can induce symptoms. Low-FODMAP Diet Reduction in high fructan foods (e.g. wheat, onion) and substitution with wheat free and other low fructan alternatives Reduction in high galactooligosaccharide foods (e.g. chickpeas, lentils) Reduction in high polyol foods and avoid polyol-sweetened sourcesReplace with suitable fruits and vegetables In those with lactose malabsorption, reduction in high lactose foods (e.g. milk, yoghurt) by restricting volume in one sitting or substitution with lactose free products. In those with fructose malabsorption, reduction in excess fructose foods (e.g. honey) NICE Guidelines Healthy eating principles (e.g. regular eating, taking time to eat). Limit high fat foods, ensure a good intake of non caffeinated fluids, limit fizzy drinks Limit insoluble fiber for diarrhea and increase gradually for constipation Limit sugar free sweets and foods containing sorbitol Limit fruit to 3 portions a day Avoiding resistant starch may be useful (e.g. pulses, sweet corn, green bananas, partbaked and reheated bread) Addition of oats and linseeds may be helpful Purpose To compare the clinical effectiveness of a low-FODMAP diet with the standard NICE guidelines for dietary therapy for IBS. Materials and Methods low-FODMAP dietetic service established with the assistance of a dietitian Resources tailored to the UK context Dietitians working in secondary and primary care trained in delivering low-FODMAP dietary advice. Materials and Methods: Study Population A total of 82 patients completed the study n=39 standard group, n=43 low-FODMAP group Consecutive adult patients returning for a follow up dietetic outpatient visit were included Common to all patients selected: diagnosed with IBS by primary care physician/gastroenterologist Had been referred for dietary advice Seen by a dietitian within the previous 2-6 months Materials and Methods: Participants Symptoms, dietary assessments and diet history's were assessed for all participants The same group of dietitians were used throughout the study Patients seen prior to June 2009 were placed in the “Standard” group. Patients seen after implementation of low-FODMAP diet were placed in the low-FODMAP group. Materials and Methods: Intervention Fructooligosaccharides, galactooligosaccharides and polyols were restricted in all patients 9 month evaluation period Written information was given to both groups at initial consultation was specific to the dietary advice given. Standard group= 2 page written resource Low-FODMAP group= color booklet Questionnaire 16 point questionnaire Verbal responses were collected regarding symptom change and satisfaction Likert scale taken from validated IBS Global Improvement Scale was used to rate symptom change Four point statements relating to satisfaction with symptom response were also asked All answers were anonymous and confidential Statistical Analysis Data analyzed using SPSS Descriptive statistics for demographic data, baseline symptom comparisons, and types of standard dietary advice Chi-squared test- symptom response and satisfaction comparison between groups Symptoms responses collapsed into improved and not improved Magnitude of improvement response collapsed into : worsened, no change, slightly improved, moderately improved, substantially improved. Results: Symptom change More patients in the low-FODMAP group reported improvements in bloating, abdominal pain, and flatulence compared to standard. low-FODMAP group less likely to report deterioration or lack of improvement for symptoms than standard. More patients in low-FODMAP group reported symptom improvements for diarrhea No significant difference in proportion of participants reporting improvements in constipation between groups More patients in the low-FODMAP group had improvements in nausea and energy levels Satisfaction with symptom response and dietary advice 76% of patients in low-FODMAP group reported satisfaction with symptom response compared to 54% in standard dietary advice group There was no difference between groups in ease of understanding of written information More patients in low-FODMAP group showed interest in implementing further change to their diet than standard group Most patients reported following the diet strictly Symptom resolution mean time= 3.5 weeks. Discussion More patients in the low-FODMAP group reported satisfaction with symptom response There was a better overall symptom response in lowFODMAP group More patients in the low-FODMAP group reported improvements in bloating, flatulence, and abdominal pain compared to standard. Strengths and Weaknesses Strengths •Used dietitians •Gave participants information to take home with them Weaknesses •No random selection •No assessment of dietary intake •Medications/ change in use of medications not recorded •Individual assessment of each symptom •Probiotic intake not recorded •Patients were similar at baseline •Multiple dietitians conducting interviews- differing ways to communicate information •Use of a control group •Overlap between diets Conclusion and Implications for Future Research This study suggests that a low-FODMAP diet may be more effective than standard dietary advice for the management of IBS symptoms. Future research on implementation and patient efficacy of a low-FODMAP diet is needed. Implementation of a low-FODMAP diet in American patients still needed. Studies on reintroducing low-FODMAP foods after a period of exclusion needed. Questions???? Judith- ”I know that this is a completely different disease, but I am curious if in your research you found that any IBS sufferers experience cyclic symptoms and if so do you believe this is diet related? If so could this be due to the vegetables/fruits that are in season?” Aubrey- “While Likert scales have been validated and effective, do you think there are any other questionnaire or collection methods that would have been more efficient? I thought that maybe food diaries would have been helpful for the RD's so they could track patient diets and make sure they were consuming the right foods.” Kirstie- “In this study they stated that fiber intake was not recorded. Do you think that recording fiber intake would have changed the results of the study?” Questions??? Sarah E.- ”Could this "diet" work for other stomach/intestine/colon issues such as after gastric bypass surgery to prevent bloating, or fiber-related advice after diverticulitis surgery?” Sarah S. “Do you know if this diet is implemented anywhere in the US? If not, can you see this becoming more of a “standard” diet prescription for individuals with IBS who do not see improvement with a standard nutrition prescription?” Katie- Do you think patients in the U.S. would have a difficult time following a low FODMAP diet?? References 1. Chirila I, Petrariu FD, Ciortescu I, Mihai C, Drug VL. Diet and irritable bowel syndrome. J Gastrointestin Liver Dis. Vol 21. Romania2012:357-362.Acessed March 10,2013 2. El-Salhy M. Irritable bowel syndrome: diagnosis and pathogenesis. World J Gastroenterol. Oct 7 2012;18(37):5151-5163. Acessed March 10,2013 3. Occhipinti K, Smith JW. Irritable bowel syndrome: a review and update. Clin Colon Rectal Surg. Vol 25. United States2012:46-52.Accessed March 20, 2013 4. Simren M, Barbara G, Flint HJ, et al. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. Vol 62. England2013:159-176. Acessed April 1,2013 5. Staudacher HM, Lomer MC, Anderson JL, et al. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. Vol 142. United States2012:15101518.March 20, 2013 6. Staudacher HM, Whelan K, Irving PM, Lomer MC. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. Oct 2011;24(5):487-495.Acessed March 10,2013