* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ICDs: What We Have Learned and Current Guidelines
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
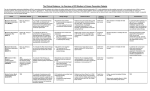
ICDs: What We Have Learned and Current Guidelines Alberto Diaz, MD Assistant Professor of Medicine, Case Western Reserve University MetroHealth Medical Center Sudden Cardiac Death • 450,000 deaths per year • 50% of all cardiovascular deaths • Incidence: 1 to 2 per 1000 people per year. Cardiac Death 65 Nonsudden Sudden 60 50 45 40 35 30 19 89 19 90 19 91 19 92 19 93 19 94 19 95 19 96 19 97 19 98 Percent 55 Zheng, et al, Circ. 2001;104:2158-2163 Sudden Death 80 75 Percent 70 35-44 45-54 55-64 65-74 75-84 65 60 55 50 45 40 Age Zheng, et al, Circ. 2001;104:2158-2163 Sudden Cardiac Death • Is an epidemic • Disproportionately affects younger, less symptomatic heart failure patients Protection: Device Therapy: The AVID Trial • The Antiarrhythmics Versus Implantable Defibrillators Trial • 1016 patients from 56 world centers with either resuscitated from SCD or had symptomatic VT with LVEF <0.40. • Randomized to ICD or drug (97% Amiodarone) therapy • Primary end point was total mortality • Mean follow-up was 18.2 months AVID: Mortality 40 Percent Mortality 35 ICD Group Drug Group 30 25 31 27 39 20 15 10 5 0 1 year 2 years 3 years ICD Survival Benefit: Secondary Prevention Studies 1 1 The AVID Investigators. N Engl J Med. 1997;337:1576-1583. Kuck K. Circ.2000;102:748-754. 3 Connolly S. Circ. 2000;101:1297-1302. 2 2 3 The AVID Trial :Overall Conclusions • ICDs are more effective than AADs in reducing arrhythmic cardiac death1 • The results of AVID may be generalized for all patients with VF and symptomatic VT. 1 • Patients in the Registry with a seemingly lower-risk (asymptomatic VT, and VF/VT associated with a transient or reversible cause) have a high mortality similar to higher risk AVID patients.2 1 The 2 AVID Investigators, JACC 1999;34:1552-1559. Anderson JL, et al. Circulation 1999; 99:1692-1699. Ventricular Fibrillation Applying Classification of Recommendations and Level of Evidence Class I Class IIa Class IIb Class III Benefit >>> Risk Benefit >> Risk Additional studies with focused objectives needed Benefit ≥ Risk Additional studies with broad objectives needed; Additional registry data would be helpful Risk ≥ Benefit No additional studies needed Procedure/ Treatment SHOULD be performed/ administered IT IS REASONABLE to perform procedure/administer treatment Procedure/Treatment MAY BE CONSIDERED Level of Evidence: Level A: Data derived from multiple randomized clinical trials or meta-analyses Multiple populations evaluated; Level B: Data derived from a single randomized trial or nonrandomized studies Limited populations evaluated Level C: Only consensus of experts opinion, case studies, or standard of care Very limited populations evaluated Procedure/Treatment should NOT be performed/administered SINCE IT IS NOT HELPFUL AND MAY BE HARMFUL Secondary Prevention I IIa IIb IIbIII III I IIa IIb III I IIa IIb III ICD therapy is indicated in patients who are survivors of cardiac arrest due to ventricular fibrillation or hemodynamically unstable sustained VT after evaluation to define the cause of the event and to exclude any completely reversible causes. ICD therapy is indicated in patients with structural heart disease and spontaneous sustained VT, whether hemodynamically stable or unstable. ICD therapy is indicated in patients with syncope of undetermined origin with clinically relevant, hemodynamically significant sustained VT or VF induced at electrophysiological study. Early Defibrillation With Early CPR Maximizes Survival >3 Min from Collapse to CPR Survival (%) <3 Min from Collapse To CPR 70 70 60 44 50 40 7 30 20 39 31 10 22 0 <6 7-12 >12 Minutes Before Defibrillation Closing the barn door after the horse is in the meadow Risk Factors For SCD •Coronary artery disease •Left ventricular dysfunction •Nonsustained Ventricular Tachycardia Potential treatments to prevent SCD in high risk patients • Optimal medical therapy for heart failure and coronary artery disease • Antiarrhythmic medicine treatment • Prophylactic ICD therapy (Primary Prevention) Number of Deaths Residual Risk of SCD in Treatment Arms of CHF Beta Blocker Trials 1 % Sudden Death of Total Death 31% No. Pts in Treatment Arm: N = 1327 16 months Average Follow-Up: 1 CIBIS-II 2 54% N = 1990 12 months Investigators. Lancet. 1999;353:9-13. Study Group. Lancet. 1999;353:2001-2007. 3 Packer M. N Engl J Med. 1996:334:349-355. 2 MERIT-HF 3 54% N = 696 6.5 months Cardiac Arrhythmia Suppression Trial (CAST) • Post myocardial infarction patients • Open label titration to achieve PVC suppression. • After confirmation of suppression: • Randomization to: – Placebo – Effective Drug (Flecainide/Encainide) • Mean follow-up 10 months Cardiac Arrhythmia Suppression Trial (CAST) Echt, et al., NEJM, 1991;324:781 Prevention: STAT CHF Trial • Patients with cardiomyopathy and LVEF <0.35. • Randomized to Amiodarone, 300 mg/d vs placebo. • 2 year survival did not differ comparing the two limbs. Primary Prevention ICD Therapy Closing the Barn Door Before The Horse Is In the meadow MADIT Trial • Multicenter Automatic Defibrillator Implantation Trial • Prophylactic ICD therapy • 196 patients – Prior MI – LVEF <0.35 – Asymptomatic Nonsustained VT MADIT Trial MADIT-II: Eligibility • Chronic CAD with prior MI • EF<0.30 • No requirement for NSVT or EPS • No upper age limitation MADIT-II: Design • Randomization: ICD vs. No ICD (3:2 ratio) • Sequential design with preset stopping boundaries for efficacy, no difference, and inefficacy of ICD vs. No ICD Primary Outcome Kaplan-Meier Survival by Treatment Group 0.78 0.69 P=0.007 (probability of survival) MADIT-II: CONCLUSION • In coronary patients with LVEF <0.30, prophylactic ICD therapy is associated with 31% reduction in mortality. • This improved survival is on top of optimal medical Rx. The Sudden Cardiac Death in Heart Failure Trial: SCD-HeFT • Design: – Prospective, Multi-center, Randomized – 2521 Patients enrolled • Inclusion Criteria: – NYHA class II/III due to ischemic or nonischemic dilated cardiomyopathy – EF 35% – CHF 3 months – Age 18 years – CHF treatment with vasodilators – No cardiac arrest or episode of sustained VT Bardy GH, et al. N Engl J Med. 2005;352:225-237 SCD-HeFT: Tested ICDs or Amiodarone on Top of Conventional Medical Therapy (CMT) Eligible Patients Electrocardiography, Liver & Thyroid function tests, Six Minute Walk, Holter Monitor and Chest Radiography Randomization 1 Patient CMT Bardy GH, et al. N Engl J Med. 2005;352:225-237 1 Patient CMT + Amiodarone 1 Patient CMT + ICD SCD HeFT Trial Amiodarone vs. Placebo ICD vs. Placebo 0.4 Hazard Ratio (97.5% Cl) 1.06 (0.86 - 1.30) 0.77 (0.62 - 0.96) Mortality Rate 0.3 0.2 0.1 Amiodarone Placebo ICD 0.0 0 No. at Risk Amiodarone Placebo ICD 12 24 36 48 60 280 304 304 97 89 103 Months of Follow-Up 845 847 829 772 797 778 Bardy GH. N Engl J Med. 2005;352:225-237. 715 724 733 484 505 501 P-Value 0.53 0.007 Conclusions In NYHA class II or III CHF patients with EF 35% on good background drug therapy: – ICD therapy significantly decreased the relative risk of death by 23% (p-value 0.007) – Resulting in an absolute reduction of 7.2% at five years – Amiodarone had no beneficial effect on survival, despite the use of appropriate dosage and reasonable compliance rates Bardy GH, et al. N Engl J Med. 2005;352:225-237 Implantable Cardioverter-Defibrillators I IIa IIb III ICD therapy is indicated in patients with LVEF less than or equal to 35% due to prior MI who are at least 40 days post-MI and are in NYHA functional Class II or III. I IIa IIb III ICD therapy is indicated in patients with nonischemic DCM who have an LVEF less than or equal to 35% and who are in NYHA functional Class II or III. I IIa IIb III I IIa IIb III ICD therapy is indicated in patients with LV dysfunction due to prior MI who are at least 40 days post-MI, have an LVEF less than or equal to 30%, and are in NYHA functional Class I. ICD therapy is indicated in patients with nonsustained VT due to prior MI, LVEF less than or equal to 40%, and inducible VF or sustained VT at electrophysiological study. Implantable Cardioverter-Defibrillators I IIa IIb III ICD implantation is reasonable for patients with unexplained syncope, significant LV dysfunction, and nonischemic DCM. I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III ICD implantation is reasonable for patients with sustained VT and normal or near-normal ventricular function. ICD implantation is reasonable for patients with HCM who have 1 or more major† risk factors for SCD. ICD implantation is reasonable for the prevention of SCD in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) who have 1 or more risk factors for SCD. ICD implantation is reasonable to reduce SCD in patients with longQT syndrome who are experiencing syncope and/or VT while receiving beta blockers. Implantable Cardioverter Defibrillators All primary sudden cardiac death (SCD) prevention implantable cardioverterdebrillator (ICD) recommendations apply only to patients who are receiving optimal medical therapy and have reasonable expectation of survival with good functional capacity for more than 1 year. New England J of Med, August 1, 2002 To the Editor: If one assumes a conservative onetime cost of $30,000 per cardiac-defibrillator implantation, heeding the call of Moss et al. to provide an implantable cardiac defibrillator for the estimated yearly flow of 400,000 new patients would cost public and private payers $12 billion annually. This cost alone is three times the estimated 2003 budget for the Centers for Disease Control and Prevention. If physicians feel that ICD therapy is: •Over-used •Financially unviable •Risks have been under represented How do we apply the therapy to those who are likely to need it? Optimize specificity Appropriate sensitivity OR How do we implant devices in those likely to use them and not implant devices in those unlikely to? Without a…… Nonsustained Ventricular Tachycardia • Meta-analysis of 12 trials of Electrophysiology Studies in patients with NSVT. • Sudden death or sustained arrhythmia: – Inducible Group: 18% – Noninducible Group: 7% – Positive Predictive Value: 18% – Negative Predictive Value: 93% T Wave Alternans – Subtle alternation in the T wave during higher atrial rates – Current technology uses a bicycle to increase atrial rate – T Wave alternans is a noninvasive marker of vulnerability to ventricular arrhythmias T Wave Alternans T Wave Alternans Predicts Arrhythmia Vulnerability Rosenbaum, et al., NEOJM 1994;330:235 Developing an innovative approach for prevention and treatment of sudden cardiac death using the noninvasive T wave alternans test to guide ICD therapy Synergistic Value of EPS and MTWA Testing EVENT RATE 0.20 0.15 EVENT RATE 0.20 0.15 0.10 P = 0.017 0.05 0.00 0.10 0.05 MTWA Abnormal / EPS + MTWA Normal / EPS 0 3 6 9 MONTHS 12.6% 12 7.5% 5.0% 2.3% 0.00 MTWA Norm EPS – ( n = 99 ) MTWA Abnorm EPS ( n = 245 ) MTWA Norm EPS + ( n = 66 ) MTWA Abnorm EPS + ( n = 156 ) Conclusions: • ICD therapy significantly reduces mortality for patients who have sustained VT or a cardiac arrest. • Primary prevention of sudden death: – Makes clinical sense because of the poor survival after cardiac arrest – Is proven to reduce mortality – Has not been implemented consistently according to ACC/AHA guidelines • Better screening of patients at high risk of SCD may increase guideline adherence Thank You