* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular System Notes
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
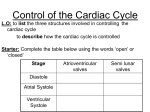
Do Now Finish the “Heart Disease” article and questions. Cardiovascular System Ch.13 Objectives - Identify the organs of the cardiovascular system and its overall function. - Label the different parts of the heart. The Cardiovascular System - Pumps 7,000 liters of a blood a DAY!!! - Contracts about 2.5 billion times in a lifetime - Functions to carry oxygen and nutrients to the cells of the body and carry carbon dioxide and other waste away from the cells of the body. Structures of the System 1. Heart - pumps blood to the lungs and throughout the body 2. Arteries, arterioles - Carry blood AWAY from the heart to cells 3. Capillaries - Tiniest tubes; place where nutrient and gas waste exchanges 4. Veins, venules - Carry blood TO the heart from cells Arteries vs. Veins - Arteries - Strong, elastic, thick - Carry blood AWAY from the heart under high pressure - Veins - Thinner, not as elastic - Contain 1-way valves Pulmonary vs. Systemic Circuits - Pulmonary - Carries Oxygen depleted blood (deoxygenated) to the lungs to pick up O2 and unload CO2. - Systemic - Sends oxygen-rich (oxygenated) blood from heart to all body cells. The Heart - Located in the thoracic cavity within mediastinum - Rests on top of the diaphragm - Distal end extends to the left - Encased in a “parietal pericardium” Wall of the Heart 1. Outer Epicardium (visceral pericardium) • Serous membrane, consists of connective tissue • Protects the heart by reducing friction 2. Middle Myocardium • Thick, mostly cardiac tissue involved in pumping blood out of the heart 3. Inner Endocardium • Made of epithelial and connective tissue • Lines the inner chambers of the heart Heart Chambers - Atria - Upper chambers - Receive blood returning to the heart - Ventricles - Lower chambers - Receive blood from atria and force blood into arteries - Septum - Separates left and right so blood doesn’t mix Septum *Remember anatomical position!! Objectives - Explain the flow of blood through the heart, lungs, and body. - To label a diagram of the heart. - Compare and contrast angina vs. a heart attack. Heart Valves - Atrioventricular Valves: separate atria from ventricles and prevent back-flow of blood: - Tricuspid: - Right side - Bicuspid/Mitral: - Left side Leaky valve Heart Valves (cont.) - Semilunar Valves: - Pulmonary: - Found between the right ventricle and the pulmonary artery - Aortic: - Found between the left ventricle and the aortic arch Heart Valve Abnormalities - Heart “murmur” 1. Regurgitation: valve doesn’t close properly, blood regurgitates back into atrium • Mitral valve prolapse: valve contracts and stretches, bulging into the left atrium 2. Stenosis: not enough blood passes through Different heart sounds! Heart Diagram Labeling! Blood Supply to the Heart • Coronary arteries: – first two branches of the aorta – supply blood to the tissues of the heart • Cardiac veins: – bring deoxygenated blood from heart tissue to coronary sinus (empties into right atrium) Angina Pectoris - A “thrombus” or “embolus” partially blocks or narrows a coronary artery and deprives myocardial cells of oxygen, causing pain. *many people mistake this for a heart attack - A complete blockage by a blood clot is a myocardial infarction (aka heart attack) Pathway of Blood - Great Pathway of Blood Video! Blood Flow • Please fill out the pathway of blood through the heart on your worksheets! Blood Flow Chart What gives us a pulse? “Pulse of Life” Lab! -Ventricular contraction causes a “surge” in arteries, distending the elastic arterial walls, pressure drops immediately after contraction -Only felt in arteries close to the surface such as your carotid in your neck Do Now - What do you think causes your heart beat? - Write the flow of blood ONLY through the heart. Objectives - To explain what occurs in a normal cardiac cycle. - To define systole and diastole. - To determine what causes heart sounds. Cardiac Cycle - Systole= contraction - Diastole = relaxing * During atrial systole, ventricles are in ventricular diastole * During ventricular systole, atria are in atrial diastole - Both relax briefly after ventricular systole - Cycle Animation Steps of the Cycle 1) Pressure is low during ventricular diastole, opening the A-V valves (tricuspid/bicuspid) 1) Ventricles fill with blood, atrial systole occurs 2) A-V valves close when ventricular pressure exceeds atrial pressure 1) Papillary muscles pull on chordae tendinae to prevent valves from bulging back into atria Steps of the Cycle 4) Atrial pressure is low (atrial diastole) and they begin to fill up again to start next cycle. 5) Ventricular pressure rises, opening the semilunar valves, forcing blood into the pulmonary trunk and aortic arch (ventricular systole) 6) Pressure drops in ventricles after contraction, and the semilunar valves close. Echocardiogram Heart Sounds - The heart makes a “Lubb-Dupp” sound - The “Lubb” is the closing of the A-V valve during ventricular contraction. - The “Dupp” is the closing of the semilunar valve when the ventricles are relaxing. Do Now - Explain the steps of the cardiac cycle. - How do you think these steps are coordinated? Objectives - To explain the cardiac conduction system - To identify the components of an EKG - To identify different heart arrhythmias Cardiac Muscle Fibers • Cardiac muscle fibers form bands of muscle that wind around the heart • Work as a unit called a functional syncytium: –Allows top and bottom parts to contract in their own unique way Cardiac Conduction System - Coordinates the events of the cardiac cycle Cardiac Conduction System 1) 2) 3) 4) 5) 6) 7) The Sinoatrial Node (SA Node)- “Pacemaker” - Specialized cardiac muscle tissue - Can depolarize on its own - Generates impulses 7080 times per minute Atrial syncytium: causes atrial contraction A-V Node A-V Bundle (Bundle of His) Right and left bundle branches Purkinje Fibers Ventricular syncytium: causes ventricular contraction Cardiac Conduction • Conduction Electrocardiogram • Recording of the electrical changes that occur in the myocardium (cardiac muscle) Electrocardiogram • P-wave: depolarization of atria • QRS complex: depolarization of ventricular fibers • T-wave: repolarization of ventricles Researching Arrhythmias • • • • • • V-fib (Ventricular Fibrillation) Sinus Bradycardia Sinus Tachycardia A-fib (Atrial Fibrillation) Atrial Flutter Asystole Do Now • In your own words, Explain the cardiac conduction system and how it works to control the cardiac cycle. Objectives • To identify EKG’s of different heart arrhythmias. • To determine how fast a heart is beating by looking at an EKG. • To explain blood pressure readings and understand how blood pressure can be effected. Reading an EKG • Read the article about reading an EKG! • How can you figure out the rate? Do Now: Identify the EKG’s! Normal EKG A. B. C. D. E. Blood Pressure • Blood pressure= the force blood exerts against the inner walls of blood vessels. • Interesting Fact! The human heart creates enough pressure to squirt blood 30 feet!! Measuring Blood Pressure • Systolic Pressure: max pressure during ventricular systole • Diastolic Pressure: max pressure during ventricular diastole Factors Affecting Blood Pressure • Heart Action – Stroke volume (vol of blood discharged with each contraction) and heart rate • Blood Volume – If you lose a lot of blood, your blood pressure will be lower. • Peripheral Resistance – If the vessels are constricted, pressure increased • Blood Viscosity – More viscous=more pressure