* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cephalosporins
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug discovery wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Theralizumab wikipedia , lookup
Ciprofloxacin wikipedia , lookup
Levofloxacin wikipedia , lookup
Dydrogesterone wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
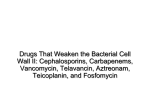
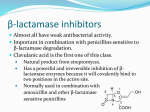
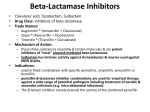
Cephalosporins Cephalosporins are grouped into generations according to their effectiveness against different organisms, their characteristics, and their development. A. Antibacterial spectrum / Pharmacotherapeutics Cephalosporins have been classified as first, second, third, and fourth generation, based largely on their bacterial susceptibility patterns and resistance to β-lactamases. 1. First generation: The first-generation cephalosporins act as penicillin G substitutes. They are resistant to the staphylococcal penicillinase (that is, they cover MSSA) and also have activity against Proteus mirabilis, E. coli, and Klebsiella pneumoniae (the acronym PEcK has been suggested). 2. Second generation: The second-generation cephalosporins display greater activity against three additional gram-negative organisms: H. influenzae, Enterobacter aerogenes, and some Neisseria species, whereas activity against gram-positive organisms is weaker (the acronym HENPEcK has been suggested with the second generation’s increased coverage). Antimicrobial coverage of cefotetan and cefoxitin also includes the anaerobe, Bacteroides fragilis. However, neither cefotetan nor cefoxitin is the preferred treatment because of the increasing prevalence of resistance amongst B. fragilis to both agents. 3. Third generation: These cephalosporins have assumed an important role in the treatment of infectious diseases. Although inferior to first-generation cephalosporins in regard to their activity against MSSA, the third-generation cephalosporins have enhanced activity against gram-negative bacilli, including those mentioned above, as well as most other enteric organisms plus Serratia marcescens. Ceftriaxone [sef-trye-AKS-own] and cefotaxime [sef-oh-TAKS-eem] have become agents of choice in the treatment of meningitis. Ceftazidime [sef-TA-zi-deem] has activity against P. aeruginosa, however, resistance is increasing and appropriate use should be evaluated on a case-by-case basis. Third generation cephalosporins must be used with caution, as they are associated with "collateral damage," essentially meaning the induction and spread of antimicrobial resistance. 4. Fourth generation: Cefepime [SEF-eh-peem] is classified as a fourth generation cephalosporin and must be administered parenterally. Cefepime has a wide antibacterial spectrum, being active against streptococci and staphylococci (but only those that are methicillin susceptible). Cefepime is also effective against aerobic gram-negative organisms, such as Enterobacter species, E. coli, K. pneumoniae, P. mirabilis, and P. aeruginosa. When selecting an antibiotic that is active against P. aeruginosa, clinicians should refer to their local antibiograms (laboratory testing for the sensitivity of an isolated bacterial strain to different antibiotics) for direction. Representative Drugs First -generation cephalosporins include cefadroxil, cefazolin sodium, and cephalexin monohydrate. Second -generation cephalosporins include cefaclor, cefprozil, cefoxitin, cefuroxime axetil, and cefuroxime sodium. Third -generation cephalosporins include cefdinir, cefixime, cefotaxime sodium, cefpodoxime proxetil, ceftazidime, ceftibuten, and ceftriaxone sodium. Fourth -generation cephalosporins include cefepime hydrochloride. Sensitivity Because penicillins and cephalosporins are chemically similar (they have what’s called a beta-lactam molecular structure ), cross-sensitivity occurs in 10% to 15% of patients. This means that someone who has had a reaction to penicillin is also at risk for a reaction to cephalosporins. B. Pharmacokinetics Many cephalosporins are administered parenterally because they aren’t absorbed from the GI tract. Some cephalosporins are absorbed from the GI tract and can be administered orally, but food usually decreases the absorption rate of these oral cephalosporins, though not the amount absorbed. Two cephalosporins (oral cefuroxime and cefpodoxime) actually have increased absorption when given with food. 1. Administration: Many of the cephalosporins must be administered IV or IM because of their poor oral absorption. 2. Distribution: All cephalosporins distribute very well into body fluids. However, adequate therapeutic levels in the CSF, regardless of inflammation, are achieved only with select a few cephalosporins. > For example, ceftriaxone or cefotaxime is effective in the treatment of neonatal and childhood meningitis caused by H. influenzae. > Cefazolin finds application as a single prophylaxis dose prior to surgery because of its 1.8-hour half-life and its activity against penicillinase-producing S. aureus. However, additional intraoperative cefazolin doses may be required if the surgical procedure lasts longer than 3 hours. > Cefazolin is effective for most surgical procedures, including orthopedic surgery because of its ability to penetrate bone. > All cephalosporins cross the placenta. 3. Metabolism Many cephalosporins aren’t metabolized at all. To a small extent, ceftriaxone is metabolized in the intestines to inactive metabolites, which are excreted via the biliary system. 4. Elimination: Elimination occurs through tubular secretion and/or glomerular filtration. Therefore doses must be adjusted in cases of severe renal failure to guard against accumulation and toxicity. An exception is ceftriaxone which is excreted through the bile into the feces and, therefore, is frequently employed in patients with renal insufficiency. Generational divide Cefuroxime (second -generation) and the third -generation drugs cefotaxime, ceftriaxone, and ceftazidime cross the blood -brain barrier after I.V. or I.M. administration. Cefepime (fourth -generation) also crosses the blood -brain barrier, but to what extent isn’t known. C. Pharmacodynamics Like penicillins, cephalosporins inhibit cell -wall synthesis by binding to the bacterial enzymes known as PBPs, located on the cell membrane. After the drug damages the cell wall by binding with the PBPs, the body’s natural defense mechanisms destroy the bacteria. D. Adverse Reactions to Cephalosporins Adverse reactions to cephalosporins include: Confusion, seizures, bleeding, nausea, vomiting, diarrhea. Ceftriaxone may be associated with a decrease in prothrombin activity (prothrombin time and partial thromboplastin time), leading to an increased risk of bleeding. Patients at risk include those with renal impairment, liver disease, or impaired vitamin K synthesis or storage. Hypersensitivity reactions are the most common systemic adverse reactions to cephalosporins. They include: hives, itching, measles -type rash, serum sickness (reaction after injection of a foreign serum characterized by edema, fever, hives, and inflammation of the blood vessels and joints) anaphylaxis (in rare cases). E. Drug interactions The patient receiving cephalosporins who drinks alcoholic beverages with or up to 72 hours after taking a dose may experience acute alcohol intolerance, with such signs and symptoms as headache, flushing, dizziness, nausea, vomiting, or abdominal cramps within 30 minutes of alcohol ingestion. This reaction can occur up to 3 days after discontinuing the antibiotic. Other Drug Interaction 1. Uricosurics (drugs to relieve gout), such as probenecid and sulfinpyrazone, can reduce kidney excretion of some cephalosporins. Probenecid is used therapeutically to increase and prolong plasma cephalosporin concentrations. 2. Cephalosporins may also decrease estrogen absorption, leading to decreased efficacy of oral contraceptives containing estrogen and progesterone. Therapeutic Application of Cephalosporins st 1 Generation Cephalosporins 3rd Generation Cephalosporins Gram (+) cocci Gram (+) cocci Staphylococcus aureus*_ Staphylococcus epidermidis Streptococcus pneumoniae Streptococcus pyogenes Anaerobic streptococci Streptococcus pneumoniae Streptococcus pyogenes Anaerobic streptococci Gram (-) rods Neisseria gonorrhoeae Escherichia coli Klebsiella pneumoniae Proteus mirabilis *Methicillin-resistant staphylococci are resistant 2nd Generation Cephalosporins Gram (+) cocci Staphylococcus aureus_ Streptococcus pneumoniae Streptococcus pyogenes Anaerobic streptococci Gram (-) cocci Neisseria gonorrhoeae Gram (-) rods Enterobacter aerogenes Escherichia coli Haemophilus in_uenzae Klebsiella pneumoniae Proteus mirabilis Anaerobic organisms** **Cefoxitin and cefotetan have anaerobic coverage Gram (-) cocci Gram (-) rods Enterobacter aerogenes Escherichia coli Haemophilus in_uenzae Klebsiella pneumoniae Proteus mirabilis Pseudomonas aeruginosa