* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Keeping the Beat
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
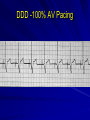
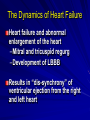
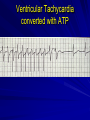
Need to Know: Implantable Devices Carolyn Brown RN, MN, CCRN Education Coordinator Emory Healthcare Atlanta, Georgia Disclosure Statement I have no relationships to disclose. Objectives Discuss the most current method of device implantation Describe indications for device therapy in the cardiac patient Manage troubleshooting in patients with an ICD or pacemaker. Address patient education and precautions. Device Therapy Pacemaker ICD Pacemaker/ICD Cardiac Resynchronization Therapy (biventricular pacemaker) Biventricular Pacemaker/ICD Pacemakers for slow symptomatic rhythms Slow rhythms that require pacing DDD -100% AV Pacing Rate Responsive Pacers Vary the rate of pacing according to the patient’s physiologic need Pacemakers All have a set rate of pacing = basic rate Magnet rate = fixed or non demand pacing at a set rate Pacemaker Terms Rate Output Sensitivity Fire Capture Intrinsic rhythm Pacer Responses Mode of response –Inhibit = stops pacing when the patient’s HR > set rate –Trigger = pacing initiated by an event Cardiac Resynchronization Therapy Biventricular Pacing Left Ventricular Remodeling Relatively normal chamber size and geometry Cohn JN, et al. J Am Coll Cardiol. 2000;35:569-582. Remodeled ventricle Electrical Conduction System Consequences of Remodeling Globular shape of the ventricles Distortion of the mitral and tricuspid valves Results in MR and TR – Increased workload and EDV The Dynamics of Heart Failure Heart failure and abnormal enlargement of the heart –Mitral and tricuspid regurg –Development of LBBB Results in “dis-synchrony” of ventricular ejection from the right and left heart Cardiac Veins Biventricular Pacing Reduces QRS Duration -------Therapy OFF---------------Therapy ON--------- Lead V3 QRS=160 ms QRS=120 ms Case Presentation 69yo woman with VF arrest, ICD implanted Idiopathic Cardiomyopathy, LVEF 20%, QRS 180ms 5 years later: Progressive CHF, NYHA Class III, Spironolactone 50mg QD, furosemide 160 BID Zaroxolyn PRN, dig, coreg, zestril, amio, etc. ICD upgraded to BiV pacing DDD ICD Case Presentation 3 months later - unscheduled clinic visit for dizziness: BP 66/50, orthostatic, wgt. loss 10lbs Diuretic dose progressively reduced during subsequent clinic visits over the next 8mos Improving functional status and exercise capacity with EF 35 - 40% Off zaroxolyn and spironolactone, furosemide dose reduced to 40mg prn Pt walking up to 2miles daily. Internal Cardioverter Defibrillators (ICDs) Fast rhythms that require cardioversion or defibrillation (Ventricular Tachycardia) Rhythms that require defibrillation (Ventricular Fibrillation) In the beginning…. Dr. Michael Mirowski identified need in 1960’s –Sudden cardiac death syndrome AICD vs ICD A History of Internal Cardioverter Defibrillators The First Generation – A shock box only – No programmable shocks – No back-up pacing A History of Internal Cardioverter Defibrillators The Second Generation – Programmable shock – Back-up VVI pacing A History of Internal Cardioverter Defibrillators The Third Generation Tiered Therapy – Anti-tachycardia Pacing – Cardioversion – Programmable shock – Back-up VVI pacing ICD with leadwire ICD Implantation with Lead Wire Patient Selection LF EF < 40 % (systolic HF) Previous Sudden Cardiac Death Unexplained syncope likely due to VF Previous STEMI (especially Anterior Wall Myocardial Infarction) History of sustained VT ICD Therapies Anti-tachycardia pacing Cardioversion Defibrillation Back-up (post shock) pacing Anti-Tachycardia Pacing Suitability for ATP – EP-proven return to SR with ATP – VT < 170 beats per minute – Monomorphic VT Ventricular Tachycardia converted with ATP Anti-Tachycardia Pacing Advantages – Quick treatment delivery – Low energy use – Painless treatment of VT – Well-tolerated by patient Anti-Tachycardia Pacing Disadvantages – Ineffective in Polymorphic VT or VF – Ineffective for VT at rates > 180 or so – Requires Defibrillation backup – May accelerate VT to VF Cardioversion Synchronized shock at 2 – 34 joules up to a certain number of attempts VT converted with cardioversion Ventricular Fibrillation with defibrillation shock VT (rate of 250) with defibrillation VT with cardioversion shock and back-up pacing Magnet Maneuvers Magnets placed over the generator will deactivate the ICD ATP/Defibrillation Once the magnet is removed, the device will resume previous settings and function Troubleshooting ICDs Effects of Drug Therapy = Rate of rhythm too slow ICD therapy based on HR If rhythm is slower than cut-off rate, device will not fire. Plan to reprogram at a lower cut-off rate. Failure of Shocks to Convert Cardiac scarring may effect success ICD malfunction Nursing Implications: – Prepare for immediate external defibrillation – Do not be afraid to “harm” the ICD! Inappropriate Shocks Potential Sensing – (? double counting) Fast rhythms that are not VT (Afib) Intervention: – Prepare to de-activate the device until MD can assess program features – Use the magnet to stop shocks! Failure to Shock Rate of rhythm too low ICD may be off or inactive Dysrhythmia may be too short Magnetic interference Sensing lead failure Device will need to be checked for proper functioning VT with ATP causing VF Appropriate Excessive Shocks Increased episodes of VT/VF Medication therapy causing increased VT/VF Nursing Implications – Move to ICU – Turn device off (magnet) – Start IV meds (amiodarone) – Sedation Patient Education What to do in case of a shock Describe shock sensation Device follow-up Potential changes in medications Avoid strong magnetic fields Driving implications Lifestyle changes Emotional & Social Concerns Anxiety and fear of shocks Social support/family support Loss of independence Fear of sex or other activities Question Anti-tachycardia Pacing (ATP) has been shown to be successful in the following ICD patient situations: A. Polymorphic VT at rates between190 to 250 B. Inducible VFib C. Monomorphic VT < 170 beats/minute D. Non-inducible tachy-dysrhythmias Answer: C Question The programmed criteria that third & fourth generation defibrillators (ICD) use to decide when to initiate treatment is: A. Body temperature B. Morphology of the QRS complex C. Level of consciousness D. Heart rate Answer: D Question The patient with an ICD should seek emergency attention if: A. More than one shock felt in 24 hours B. The device has not fired in two days C. The ATP mode is used more than 3 times/day D. A beep sounds near electromagnetic field Answer: A Question True or False The purpose of Cardiac Resynchronization Therapy is to enhance cardiac output by stimulating both ventricles simultaneously. Answer: True