* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Spatial behavior reflects the mental disorder in OCD patients with
Pyotr Gannushkin wikipedia , lookup
Asperger syndrome wikipedia , lookup
Narcissistic personality disorder wikipedia , lookup
Rumination syndrome wikipedia , lookup
Political abuse of psychiatry wikipedia , lookup
Generalized anxiety disorder wikipedia , lookup
Excoriation disorder wikipedia , lookup
Spectrum disorder wikipedia , lookup
Moral treatment wikipedia , lookup
Conversion disorder wikipedia , lookup
Mental status examination wikipedia , lookup
History of psychosurgery in the United Kingdom wikipedia , lookup
History of mental disorders wikipedia , lookup
Dissociative identity disorder wikipedia , lookup
Emergency psychiatry wikipedia , lookup
Glossary of psychiatry wikipedia , lookup
Schizophrenia wikipedia , lookup
Psychosurgery wikipedia , lookup
History of psychiatric institutions wikipedia , lookup
History of psychiatry wikipedia , lookup
Sluggish schizophrenia wikipedia , lookup
Obsessive–compulsive personality disorder wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
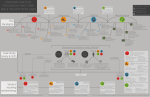
ORIGINAL RESEARCH CNS Spectrums, page 1 of 14. & Cambridge University Press 2013 doi:10.1017/S1092852913000424 Spatial behavior reflects the mental disorder in OCD patients with and without comorbid schizophrenia Anat Gershoni,1 Haggai Hermesh,2 Naomi A. Fineberg,3 and David Eilam1*1 Department of Zoology, Tel-Aviv University, Ramat-Aviv, Israel CBT Unit, Geha Mental Health Center, Petah Tikva, Sackler Faculty of Medicine, Tel Aviv University, Ramat-Aviv, Israel 3 National OCD Treatment Service, Queen Elizabeth II Hospital, Welwyn Garden City, UK 2 Objective. Resolving the entangled nosological dilemma of whether obsessive-compulsive disorder (OCD) with and without schizophrenia (schizo-OCD and OCD, respectively) are two independent entities or whether schizo-OCD is a combined product of its parent disorders. Methods. Studying motor activity in OCD and in schizo-OCD patients. Performance of the patients was compared with the performance of the same motor task by a matching control individual. Results. Behavior in both schizo-OCD and OCD patients differed from controls in the excessive repetition and addition of acts, thus validating an identical OC facet. However, there was a significant difference in spatial behavior. Schizo-OCD patients traveled over a greater area with less focused activity as typical to schizophrenia patients and in contrast to OCD patients, who were more focused and traveled less in a confined area. While schizo-OCD and OCD patients share most of the OC ritualistic attributes, they differ in the greater spread of activity in schizo-OCD, which is related to schizophrenia disorder. Discussion. It is suggested that the finding on difference in spatial behavior is a reflection of the mental differences between OCD and schizophrenia. In other words, this could be an overt and observable manifestation of the mental state, and therefore may facilitate the nosology of OC spectrum disorders and OCD. Conclusion. It seems as if both the OCD patients’ focus on specific thoughts, and the contrasting wandering thoughts of schizophrenia patients, are reflected in the focused activity of the former and wandering from one place to the next of the latter. Received 26 March 2013; Accepted 16 May 2013 Keywords: OC behavior, OCD, Rituals, Schizophrenia, Spatial behavior. Clinical Implications > > > > > There is an overt behavioral difference between comorbid schizophrenia and OCD (schizo-OCD) compared with OCD. OCD patients are mostly stationary, whereas schizo-OCD patients wander over a large space. However, as in OCD, schizo-OCD patients have excessive repetition and addition of acts. These features may serve as bedside sign and facilitate the nosology of OC spectrum disorders and OCD. These overt differences may also reflect the differences between OCD and schizophrenia in cognition, attention, and brain malfunctioning. y We are grateful to the anonymous patients and control individuals who willingly participated in this study. *Address for correspondence: David Eilam, Ph.D., Department of Zoology, Tel-Aviv University, Ramat-Aviv 69978, Israel. (Email: [email protected]) Introduction Obsessive-compulsive disorder (OCD) and schizophrenia are distinct diagnostic entities.1,2 The main features of OCD are as follows: (i) obsessions, which are recurring, persistent thoughts, impulses, or images that are experienced as intrusive and unwanted and causing marked distress or anxiety, and (ii) compulsions, which are repetitive motor behaviors such as checking or mental behaviors such as counting that occur in response to an obsession and are performed according to strictly applied rules.3 However, observations have revealed that disparate mental disorders may also possess obsessive-compulsive (OC) features, leading to the concept of the OC spectrum disorder (OCSD).4–9 Schizophrenia, on the other hand, consists of both positive symptoms, such as delusions (fixed false beliefs), hallucinations, disorganized speech, and abnormal psychomotor behavior, and negative symptoms, such as diminished emotional expression.3 2 A. Gershoni et al. Two nosological notions have been suggested to explain the association and relationship between OCD and other Axis-I mental diagnoses, including schizophrenia disorder: comorbidity and spectrum. According to the comorbidity notion, there is an endophenotype that is a combination of OCD and schizophrenia (‘‘schizo-OCD’’), whereas according to the spectrum notion, schizo-OCD is a subtype of schizophrenia.10–12 While comorbidity implies that each disorder maintains its own features, the spectrum notion suggests that schizo-OCD patients have a unique pattern of neuropsychological deficits.10,13 Furthermore, schizo-OCD patients are considered more impaired14 and have greater neurocognitive deficits compared with either patients with OCD or schizophrenia alone.10 A synthesis of both comorbidity and spectrum notions has also been suggested, presenting a continuum of comorbidity between OCD and schizophrenia.1 This spectrum comprises four subgroups: (i) schizophrenia in OCD patients, (ii) schizotypal personality disorder (SPD) in OCD patients, (iii) OCD with poor insight, and (iv) schizophrenia with OC features. The prevalence of schizophrenia in OCD patients has been reported to be as high as 4%; nonetheless, OCD patients have no greater chance of developing schizophrenia later in life.1,15 Schizophrenia patients with OC symptoms are a well-described group, comprising 7.8–55% of schizophrenics.1,16–18 Traditionally, it was suggested that, for the most part, schizo-OCD patients are primarily schizophrenic patients that additionally suffer from comorbid OC symptoms.1 A comparison of schizophrenic symptoms and signs between patients with schizophrenia with or without OCD revealed no difference,16,19–21 though increased levels of cognitive inflexibility have been detected in neurocognitive tests in schizo-OCD.22 Thus, the target of this study was to answer the outstanding question regarding schizo-OCD: Is it a comorbidity that integrates symptoms of its parent disorders, or is it a subtype of one of the parent disorders? OCD, schizo-OCD, and schizophrenia may represent different states along the continuum of thought disorder. One end of this continuum is that of the obsessive thought process that characterizes OCD, consisting of repetitive thoughts that the patients perceive as senseless and unwanted.14,23 The other end of the continuum is that of the delusive process of fixed false beliefs that characterizes schizophrenia.3,14 In between these ends, there are the overvalued ideas and OCD with poor insight that appears in schizoOCD. In this state, patients no longer address their obsessions as senseless and unwanted, but view them as realistic.14–16 Despite the above differences between the three states, several studies have suggested that schizo-OCD patients do not differ significantly from patients with schizophrenia (without OCD) in terms of the global assessments of functioning.19 Schizophrenic, schizo-OCD, and OCD patients may also differ in the motor manifestation of the respective disorders. Schizophrenic patients mainly suffer from several motor dysfunctions, including hypokinesia, catatonia, catalepsy, and Parkinsonism without overt motor tasks.24 In contrast, schizo-OCD patients display compulsive motor tasks that are reminiscent of those displayed by nonpsychotic OCD patients.25 Accordingly, in the present study, we set out to compare the motor behavior of OCD and schizo-OCD patients in order to uncover the differences and similarities between these two psychiatric categories. Spatial motor behavior in schizophrenic patients spreads over a wide area, involving a greater locomoted distance,26 whereas OCD motor behavior (compulsions) is repetitive, comprising numerous nonfunctional acts that seem irrelevant for the current task, and are performed with high concentration.27–29 In light of these differences, we assumed that the dissimilar cognitive impairments in both illnesses would manifest differently in the spatial organization of their motor behaviors. Specifically, OCD patients were expected to pay more attention and have more confined and focused motor behavior, whereas schizoOCD patients were expected to be more disoriented, paying less attention to details, and featuring dispersed motor behavior. A comparison of OCD and schizo-OCD behavior may facilitate the nosology of OC spectrum disorders and OCD, and may facilitate the separation of these disorders with overt motor signs, adding a different and new perspective to the effort to resolve the nosological dilemma of whether schizo-OCD is an independent entity or merely a combination of its basic parent disorders. Methods Participants Ten motor tasks of OCD patients, 10 tasks of patients suffering from schizo-OCD, and 20 tasks of normal controls were extracted from video files. Patients met Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) and SCID (structural clinical interview for DSM-IV) criteria for OCD, both without or with schizophrenia disorder. All patients have demonstrated compulsions with obvious motor rituals. In the frequent case of comorbidity, OCD was the primary disorder among all anxiety and/or mood disorders. None of the participants had either Tourette disorder or multiple tic disorders. The 10 OCD tasks were contributed by 7 patients, with 3 of them performing 2 tasks each and 4 performing 1 task each. The 10 schizo-OCD tasks were contributed by 6 patients, 3 of them performing 2 Behavior in OCD with and without schizophrenia tasks each, and the other 3 patients performing 1 task each. The themes of the tasks were determined by the patients, with each performing a behavior that was prevalent in her/his recent behavior. Each of the above OCD and schizo-OCD patients was matched with a healthy control individual of the same gender and age, who was requested to perform the same motor task that the patient performed. The patients’ background and task characteristics are depicted in Table 1. Tics not meeting criteria for Tourette disorder were observed in patient #15. Patients from both groups did not differ in age (F1,11 5 1.42; P 5 0.26), number of mental diagnoses (F1,11 5 0.38; P 5 0.55), and Y-BOCS score (F1,11 5 1.5; P 5 0.24). Patients were recruited from an Israeli regional psychiatric outpatient clinic and an anxiety disorder and cognitive behavioral therapy (CBT) unit at the Geha Mental Health Center, Israel. The study was approved by the Helsinki Committee of Geha Mental Health Center. Participants signed an informed consent. Procedure Patients and their respective controls were each videotaped by the psychiatrist and experimenter at their homes, where they routinely perform their motor behavior. Assessment of each patient was made by a senior clinical psychiatrist using the Y-BOCS (Yale–Brown Obsessive Compulsive Scale) questionnaire. Afterward, a short conversation about the patient’s current mental state and the compulsive behaviors commonly performed in the recent period led to a decision about the specific tasks, which would be video-recorded for analysis. The patients were then asked to perform the task on camera in the same manner as they do in their everyday life. Each control individual was requested to perform the same task as her/his respective patient. Data acquisition and analysis A task was defined as the set of acts executed by the patients or control individuals. Each of them set the beginning and end of their task. For example, the start was set when a patient said he was showing how he ‘‘washes hands,’’ and ended when he said that he was done. Similarly, the matched control was requested to show how he washed his hands, until he said that he was done. All the acts performed between the beginning and end of each task were listed and scored. Acts were scored according to the location or object on which they were performed. For example, in the task of ‘‘washing hands,’’ the act ‘‘turn on’’ was performed on the object ‘‘tap’’ and the act ‘‘take’’ was performed on the object ‘‘soap’’; in the task ‘‘going out from home,’’ the act ‘‘turning lights on and off’’ was performed at two locations: ‘‘the bedroom’’ and ‘‘the 3 living room.’’ According to this procedure, the patients, by setting the beginning and end of the task, also set the task domain to include all the objects/locations on which they performed acts during the task. The acts and the locations/objects at which they were performed were scored using the Observer XT 10.1 (Noldus Information Technology, the Netherlands), a software program for ethological description. The Observer output contained a sequential list of the acts and objects/locations. Acts underwent further classification in accordance with the proximity to the performer, as follows: 1. Self—acts that were performed on the patient’s body while the patient was stationary. An example of an act with self proximity is ‘‘rubbing hands’’ or checking a trouser’s pocket. 2. Stationary—acts performed on objects other than the patient’s body, while she/he did not move from their place. An example of an act with stationary proximity is ‘‘touching the doorknob.’’ 3. Travel—acts performed on an object/location requiring the patient to walk to that location/ object. This category was further divided into two subcategories: i. Nearby travel—a travel trajectory of up to 2 steps (up to 75cm). ii. Far travel—a travel trajectory of more than 2 steps (further than 75 cm). This definition was based on a step-length of ca. 32 cm (http:// www.footlab.co.il/03_walk/19_measures.asp). Statistics A two-way analysis of variance (ANOVA) with repeated measure (ANOVA-RM) was used to analyze the differences among OCD, schizo-OCD, and normal control groups (between-group factor) and the spatial categories of acts (proximity—self, stationary, and travel; within-group factor). Post-hoc Tukey HSD (honestly significant difference) tests were used as needed to further analyze the ANOVAs results. A comparison of the number of locations/objects in a task and the number of visits in each location/object was carried out by means of a one-way ANOVA. A comparison of the number of steps each individual executed in the ritual was carried out by means of a one-way ANOVA. Significance was determined at p , 0.05. Continuous data are presented as mean and standard error (±SEM). Findings OCD and schizo-OCD patients differed in their spatial behavior but not in the OC rituals Figure 1 depicts the distribution of the proximity of acts in OCD, schizo-OCD, and control individuals. 4 A. Gershoni et al. Table 1. Characteristics and motor tasks in obsessive-compulsive disorder (OCD) patients with and without schizophrenia. Patient no. Type of OCD Motor task Age Age of OCD onset 1 2 3 OCD OCD OCD Clean phone Lock door Go out 50 31 68 25 12 25 4 OCD Go out 26 13 5 OCD 54 12 6 OCD 62 27 OCD; Generalized anxiety disorder; MDD; simple phobic disorder (panic & agoraphobia) OCD; Panic; IBS; Agoraphobia; MDD 7 OCD 21 18 11 Schizo-OCD Wash hands Lock door Clean cloth Clean closet Lock door Wash hands Make tea 28 Not known 12 Schizo-OCD 42 6 13 14 Schizo-OCD Schizo-OCD 47 32 18 10 15 Schizo-OCD 36 12 16 Schizo-OCD 23 14 Go out Arrange closet Wash hands Go out Clean sink Go out Clean table Lock door Medication mg/day Diagnoses OCD; MDD OCD OCD; Compulsive shopping; Dysthymia; Agoraphobia; Borderline personality; MDD; Hypochondriasis OCD; MDD; Nail Biting Y-BOCS Clomipramine 300; quetiapine 400 Clomipramine 300 ; mazoril 150 Amantadine 100; lamotrigine 350; flouxetine 60 25 19 22 Clomipramine 300; olanzepine 15; citalopram 20 Fluvoxamine 100; diazepam 5; sulpiride 200 30 14 Eltroxin 50; flouxetine 40–50; olanzepine 26 OCD; GSP; IBS; DSPS; Stuttering Sertraline 200 21 OCD; Schizophrenia; BDD Clotiapine 160; paroxetine 80; carbamezapine 400 ; clonazepam 1.5 Lithium 1500; trihexyphenidyl 5; levomepromazine 500 Sulpiride 100; clozapine 500; citalopram 20 Clomipramine 300; risperidone 4 36 21 22 Amisulpride 100; trazodone 50 21 Olanzepine 15; flouxetine 20 25 OCD; Schizophrenia; Borderline personality disorder OCD; Schizophrenia OCD; Schizophrenia; SP; s/p MDD; s/p BDD OCD; Schizophrenia; SP; Trichotillomania; Tics OCD; Schizophrenia 34 Other disorders noted in the table are as follows: MDD–major depressive disorder; IBS–irritable bowel syndrome; GSP–generalized social phobia; DSPS–delayed sleep phase syndrome; BDD–body dysmorphic disorder; SP–social phobia; Y-BOCS–Yale–Brown obsessive compulsive scale.41 Behavior in OCD with and without schizophrenia 5 Figure 1. Proportion of acts according to their proximity in OCD, schizo-OCD, and control individuals. All the acts that comprised each motor task were divided into self, stationary, and travel acts. The proportion of act proximity is depicted as the average (± SEM) percentage of all acts in each motor task. The asterisk indicates a significant difference in travel acts between the schizo-OCD and OCD groups. revealed that the percentage of ‘‘travel’’ acts in schizoOCD patients was significantly greater than in OCD patients and control individuals. ‘‘Travel’’ acts underwent further classification into ‘‘nearby’’ and ‘‘far’’ acts (see Methods section). The relative number of these subtypes was compared by means of ANOVA-RM, which revealed a significant difference between OCD, schizo-OCD, and control individuals (between-group effect; F2,37 5 17.25, p , 0.0001), a significant difference between nearby and far acts (within-group effect; F1,37 5 26.32, p , 0.0001), but no significant interaction (F2,37 5 0.28, p 5 0.69). Notably, there were no ‘‘far’’ acts in any of the 10 OCD motor tasks (Figure 2). Thus, while OCD patients were more stationary than control individuals, schizo-OCD patients traveled further compared to control individuals when performing the same activity. The number of steps taken by the participating individuals during the task differed significantly between OCD, schizo-OCD, and control groups (oneway ANOVA, F2,37 5 20.3, p , 0.0001). The Tukey HSD test revealed a significant difference between OCD and schizo-OCD patients and between the schizo-OCD and the control groups, but no significant difference between OCD patients and control individuals. These results highlighted the contribution of schizophrenia to the spreading out of the motor activity in schizo-OCD patients, as manifested in the increased number of steps. Indeed, OCD patients and control individuals performed fewer steps compared with schizo-OCD patients, with the latter taking significantly more steps and covering a greater area (Figure 3). In the present analysis, spatial behavior is considered as a set of locations or objects that the tested individuals visited during the activity, and the set of acts performed Figure 2. ‘‘Nearby’’ and ‘‘far’’ traveling in each motor task. These are depicted as the percent average (± SEM) of each travel category (nearby/far) out of the total travel acts. The asterisk indicates a difference between nearby acts in schizoOCD compared with all other act types and groups in this figure; # indicates a significant difference between far acts in schizo-OCD and OCD patients. Figure 3. The number of steps taken by OCD, schizo-OCD, and control individuals. The asterisk indicates significant difference between schizo-OCD compared with OCD and control individuals. ANOVA-RM revealed that there was a significant difference between the three diagnostic groups (F2,37 5 4.78, p 5 0.014), a significant difference between proximities (F2,74 5 52.58, p , 0.0001), and a significant interaction (disorder 3 proximity; F4,74 5 2.94, p 5 0.025). The interaction implies a difference in proximity among the three groups (schizo-OCD, OCD, and control individuals). A Tukey HSD test revealed that the share of stationary acts in OCD behavior was significantly higher than that of both self and travel acts (71%, 20%, and 8%, respectively; Figure 1). In schizo-OCD behavior, the share of stationary acts was smaller, along with an increase in ‘‘travel’’ (55%, 15%, and 30%, respectively; Figure 1). Control behavior matched that of OCD rituals (70%, 17%, and 13%, respectively; Figure 1). Tukey HSD tests 6 A. Gershoni et al. at each such object/location. A one-way ANOVA revealed a significant difference in both the number of objects/locations and in the total number of visits to these objects/locations (F2,37 5 5.55, p 5 0.007 and F2,37 5 4.59, p 5 0.016 for locations and for visits, respectively; Figure 4). A Tukey HSD revealed that the control and schizo-OCD groups differed significantly, whereas the OCD group featured an intermediate rank. These results illustrate a trend of increased spatial activity that reached significance in only the schizo-OCD group. It should be noted that the index for the wider task domain in schizo-OCD Figure 4. The number of objects/locations and the number of visits to each object/location. Asterisks indicate a significant difference between the number of visits and objects/locations in control individuals compared with schizo-OCD patients. behavior is the proximity among objects or locations (Figures 1–3), whereas the number of objects/locations and the visits to these objects/locations (Figure 4) is an index of activity rather than for the spatial distribution of this activity. The above results demonstrate that OCD activity was focused and confined in space, with the patients being mostly stationary; in contrast, activity in schizo-OCD was dispersed over a greater area. This is illustrated in Figure 5 (and the supplementary file), which displays an animation of one OCD and one schizo-OCD patient showing the same motor activity that they had both described as ‘‘going out from the apartment.’’ As shown, the OCD patient was mostly stationary, standing in one place and checking the contents of his pockets and then taking the keys and mobile phone and going to the door. In contrast, the schizo-OCD patient traveled around in the apartment, first going to switching on and off lights in the toilets, taking the keys and phone and going to the door, but then returning to scan the bedroom, then taking again the keys and phone and going to the door, but returning again to empty the ashtray, taking again the keys and phone and going to the door, and so on. Altogether, the differences between the stationary nature of OCD behavior compared with the dispersed activity in schizo-OCD are apparent in this exemplary animation. Figure 5. The trajectories and acts in exemplary OCD and schizo-OCD patients, each performing the motor tasks of ‘‘going out from the home.’’ The location of each circle represents an object/location, while circle size represents the number of acts that took place at that location/object. The green line represents the trajectories of each individual between the locations. Behavior in OCD with and without schizophrenia OCD did not differ from schizo-OCD patients in the structural components of their rituals In contrast with the discernible above differences between OCD and schizo-OCD patients in terms of their spatial behavior, these patients did not differ significantly in any of the 24 parameters that characterize obsessive-compulsive motor behavior29–31; however, each group of patients significantly differed in these parameters from their respective control groups. This is illustrated in Table 2, which lists the 9 most important obsessive-compulsive behavioral parameters (according to Eilam et al.31). The finding implies that both schizo-OCD and OCD patients share similar obsessive-compulsive characteristics that differ from normal behavior; but also differ from one another in the spatial distribution of this obsessive-compulsive behavior. OCD patients are known to have numerous repetitions and additions of unnecessary acts in their motor activity, which makes their behavior nonfunctional.30 Here we found that compared with their respective controls, OCD and schizo-OCD patients seemed equally nonfunctional when performing similar motor tasks. Tables 3 and 4 depict a ‘‘clean object’’ motor task, and Tables 5 and 6 depict a ‘‘going out’’ task. Each of these motor tasks is described for both the OCD and schizoOCD patients, compared with their respective control individuals. Each column in these tables stands for the object/location at which each of the specified acts took place. The order of act performance is given left-to-right and top-to-bottom. Altogether, these tables illustrate the similarity between OCD and schizo-OCD behavior. The activity displayed in Tables 3–6 is summarized in Table 7, which demonstrates the cumulative differences between OCD and schizo-OCD motor behavior. Clearly, compared with the control individuals, both OCD and schizo-OCD patients displayed more elaborate activity that included more repetitions and the addition of unnecessary acts, as well as more 7 objects/locations. However, these OC properties did not greatly differ between OCD and schizo-OCD, suggesting that the difference between these disorders is in the spatial organization of behavior. Discussion In our study, schizo-OCD patients traveled more across the room compared with the OCD or normal controls who performed similar motor tasks. Schizo-OCD patients also displayed a ritualistic behavior reminiscent of that of OCD patients without schizophrenia. We suggest that these features indicate that traits of both OCD and schizophrenia occur in schizo-OCD patients, supporting the notion of comorbidity. More specifically, we found that the overall level of OC activity did not differ between schizo-OCD and OCD patients, but that the spatial distribution of their activity greatly differed. Indeed, OCD patients were mostly stationary when performing motor tasks, whereas schizo-OCD patients were much more mobile, wandering over a large area. Control individuals had a mixture of both stationary and nonstationary behavior. In the following discussion, we suggest that the difference in spatial behavior between OCD and schizo-OCD patients offers a reliable reflection of the mental differences between OCD and schizophrenia, and that such a difference may facilitate the nosology of OC spectrum disorders and OCD.5,8,9,32 Obsessions, disturbed thought processes, and their manifestation in OCD and schizophrenia OCD and schizophrenia seem to represent two extremes on a continuum of disrupted thought processes.14 In OCD, the patients suffer from obsessions that refer to recurring, persistent thoughts, impulses, or images that inappropriately intrude into awareness and cause marked distress or anxiety. In response to obsessions, OCD patients may display compulsions, which are over-repetition of physical behaviors such as checking, Table 2. Structural components of motor activity in OCD compared with Schizo-OCD patients (values are mean ± SEM). Results of Man-Whitney test are depicted for each parameter (U and P values). Parameter Task duration (sec.) Number of visits in a task (repetitions included) Visit duration (sec.) Number of different locations/objects (repetitions excluded) Visit repetition Number of acts in a task (repetitions included) Act duration Number of different acts (repetitions excluded) Act repetition OCD Schizo-OCD U P 56.1 ± 24.3 12.8 ± 5.1 13.8 ± 4.8 9.4 ± 3.6 2.1 ± 0.2 8.0 ± 3.8 23.3 ± 8.4 6.2 ± 2.4 15.0 ± 8.8 89.5 ± 37.1 22.4 ± 9.1 24.8 ± 10.0 14.4 ± 5.5 3.0 ± 0.6 19.5 ± 9.1 38.4 ± 14.5 8.4 ± 3.2 24.8 ± 9.1 29 31 29 32 35 25 44 27 33 0.11 0.15 0.11 0.19 0.26 0.06 0.65 0.08 0.20 8 A. Gershoni et al. Table 3. Exemplary set of acts of an OCD patient and the respective control, both performing a cleaning task. Objects/locations are listed in the top row and the sequence of acts performed at each object/location is given by reading left to right and top to bottom. Objects/locations Body Rag Headset Phone Notepad Numbers Line Paper Control individual Bend over Lift Hold 3 2 Turn Move forward Bend over Touch Wipe with rag 3 2 Lift Wipe with rag Bend over Put down Straighten Move back OCD patient Lift Lift Lift Put down Wipe with rag 3 8 Hands hold 3 2 Move Wipe with rag Wipe with rag 3 2 Move Turn over Wipe with rag 3 4 Wipe with rag Move Put down 3 2 Lift Wipe with rag 3 2 Lift Move 3 2 Wipe with rag Put down Hand hold Move Move Put down or mental behaviors such as counting things.3 Schizophrenia includes delusions and disorganized behavior, trouble with thinking and concentration, and difficulty in paying attention and making decisions.33 Here we suggest that the distinctive cognitive properties of each disorder are also manifested in the overt motor behavior, as revealed in the present and previous studies. Specifically, a high or exaggerated attentional focus and over-concentration is a salient feature of OCD patients when they display their motor tasks.27–30,34 In other words, we suggest that OCD patients demonstrated restricted spatial motor behavior as a reflection of their high concentration in performing their highly organized motor routines.27 The present results contribute to this by revealing that the high concentration and focusing on performance by OCD patients are accompanied by their being stationary and relatively immobile. In contrast, schizophrenia patients Behavior in OCD with and without schizophrenia 9 Table 4. Exemplary Schizo-OCD (bottom) and control (top) individuals performing a cleaning task. Objects/locations are listed in the top row. The structure of the table is similar to that in Table 3. Objects/locations Body Dispenser Top part table Short end table Ashtray Button right side Button left side Control individual Move forward Take out soap Bend over Put down Rise up Bend over Wipe with rag Lift Rise up Move forward Schizo-OCD patient Bend over Wipe with rag Wipe with rug Move Wipe with rag Move back Bend over Wipe with rag Move forward Wipe with rag Rise up Wipe with rag Wipe with rag Rise up Move back Move forward Wipe with rag Bend over Rise up Move forward Band over Wipe with rag Wipe with rag Wipe with rag Rise up Wipe with rug Move forward demonstrated extensive exploratory behavior, traveling back and forth across the room.26 Furthermore, compared with normal controls, these latter patients are more active in the center of the room and spend more time walking during their exploration.26 Accordingly, schizo-OCD patients seem to combine motor features from both OCD and schizophrenia. Our study thus suggests that schizo-OCD patients combine on the one hand the addition and repetition of acts that are reminiscent of OCD, and on the other hand, they travel back and forth during their ritual in a manner that is reminiscent of schizophrenia, thus supporting the notion of comorbidity. Attention deficits in OCD and schizo-OCD OCD and schizophrenia patients experience opposite impairments in their attention abilities. While OCD patients are obsessed with recurring thoughts or rituals, schizo-OCD patients are disorganized in their thoughts and behavior.28,35 In other words, OCD is a disorder of incessant repetition of thoughts and 10 A. Gershoni et al. Table 5. Exemplary OCD (bottom) and control (top) of individuals going out from home. Objects/locations are listed in the top row. The structure of the table is similar to that in Table 3. Objects/locations Door Touching the door/handle Body Touching or turning the key Upper lock Walls Pushing the carpet with one of the legs Control individual Open Right hand Move forward Turning Close Right hand Right hand Turning Locking Schizo-OCD patient Move forward Opening Left hand Pushing Move forward Turning Left hand Move back Left hand Move forward Left hand Open Right hand Turning Touching Left hand Pushing Right hand Close Touching Left hand Turning Taking Touching Right leg Move back Right leg 3 2 Move back Move forward Right leg Move back Right leg 3 4 Turning Move forward activities, whereas schizophrenia is a disorder of continuous shifting from one thought/activity to the next. Indeed, early studies in schizophrenia patients showed a remarkable characteristic of attention deficit35 that correlates with the severity of the disorder and remains constant in time.36 In contrast, a salient feature of OCD patients is their high attention when displaying their motor tasks.27–30,34,37 In other words, OCD patients have difficulty in shifting their attention from one part of the motor task to another, resulting in Behavior in OCD with and without schizophrenia 11 Table 6. Exemplary schizo-OCD (bottom) and control (top) individuals going out from home. Objects/locations are listed in the top row. The structure of the table is similar to that in Tables 3–5. Objects/locations Door Touching the door/handle Body Touching or Holding and touching turning the key then keychain Turning lock Right hand Control individual Left hand Open Move forward Hold Turning Left hand Close Touching Turning Touching Move back Holding OCD patient Left hand Open Move forward Turning Close Left hand Touching Turning Touching Holding Holding Left hand Touching Turning Left hand Turning Right hand Open and close Right hand Back and forward Turning Holding Move forward a delay in task performance.22 Furthermore, OCD patients perform significantly better than schizophrenia patients in a simple attention task.38 Compared with schizophrenic patients, schizo-OCD patients had a lower score in tests for attention abilities.22 Nonetheless, both schizo-OCD and schizophrenia patients demonstrate the same category of impaired attention in contrast with OCD patients, indicating a similar origin of cognitive deficits. Considering that behavior is a direct manifestation of brain activity, we suggest that the focused and confined activity in OCD compared with the divergent activity over a large area 12 A. Gershoni et al. Table 7. Comparison between the OCD, schizo-OCD, and control individuals who displayed the activities show in Tables 3–6 Going out from home Cleaning task Control Schizo-OCD Control OCD Control Schizo-OCD Control OCD 9 1.3 5 1 38 2.7 7 8 12 1 5 8 23 1.6 7 6 10 1.4 3 3 27 3 7 9 16 1.3 4 8 39 1.6 6 24 Number Average Number Number of acts (repetitions included) rate of act repetition of objects/locations of unique acts Data for each individual are depicted along the columns. The data column of each patient is followed by the data of his or her respective control. in schizo-OCD is a reflection of the focused attention in the former and the continuously shifting attention in the latter. In other words, the attentional deficit in the schizo-OCD patients is an overt schizophrenia feature. Cognitive deficits in the executive function in OCD and schizo-OCD Attention is the foundation of other high cognitive abilities, such as executive functions and memory performance.35 Executive functioning is an umbrella term for cognitive processes, such as attention, working memory, and planning.39 Therefore, cognitive dysfunction can be manifested in the impairment of executive functions.35 Such an impairment could be differentially manifested in OCD and schizophrenia.16,40 Schizophrenia patients experience deficits in the integration of cognitive activity and the inability to pay attention to details. In contrast, OCD patients demonstrate a different type of deficit in executive functions, as manifested in dysfunction of impulse control and regulation of behavior.40 In light of this difference, it was suggested that schizo-OCD patients would represent a more severe executive function impairment that combines both types of deficits, due to the comorbid nature of their disorder.40 For example, in a task of ‘‘going out from home,’’ the schizo-OCD patient took his key, walked to the door, then went back inside to check the lights in the bedroom, went back to the door, returned back to check the bathroom light, then went back to the door, and so on. The OCD patient did not go back and forth, but stood at the light switch and checked it repeatedly. In all, schizo-OCD patient cognitive impairments in both the fields of attention and of regulation additionally support the notion of comorbidity. Conclusion The present findings demonstrate that the spatial distribution of motor activity varies between OCD and schizo-OCD patients, with the former being mostly stationary and the latter wandering over a large space. We suggest that these overt differences reflect the differences between OCD and schizophrenia in cognition, attention, and brain malfunctioning. These behavioral differences may serve as bedside signs and facilitate the nosology of OC spectrum disorders and OCD. Disclosures Naomi Fineberg has the following disclosures: Servier advisor, support fees, research, research support; Lundbeck advisor, consulting fees; Transept consultant, consulting fees. The other authors have nothing to disclose. Supplementary materials To view supplementary material for this article, please visit http://dx.doi.org/ 10.1017/S1092852913000424 References 1. 2. 3. 4. 5. 6. Poyurovsky M, Koran L. Obsessive-compulsive disorder (OCD) with schizotypy vs. schizophrenia with OCD: diagnostic dilemmas and therapeutic implications. J Psychiatr Res. 2005; 39: 399–408. Poyurovsky M, Zohar J, Glick I, et al. Obsessivecompulsive symptoms in schizophrenia: implications for future psychiatric classifications. Compr Psychiatry. 2012; 53: 480–483. American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychological Association; 2000. Jenike MA, Baer L, Minichiello WE. Obsessive-Compulsive Disorders: Theory and Management, 2nd ed. Chicago: Year Book Medical Publishers, Inc.; 1990. Hollander E. Obsessive-Compulsive Related Disorders. Washington, DC: American Psychiatric Press; 1993. du Toit PL, van Kradenburg J, Niehaus D, Stein DJ. Comparison of obsessive-compulsive disorder patients with and without comorbid putative obsessive-compulsive spectrum disorders using a Behavior in OCD with and without schizophrenia 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. structured clinical interview. Compr Psychiatry. 2001; 42: 291–300. Fineberg NA, Saxena S, Zohar J, Craig KJ. Obsessivecompulsive disorder: boundary issues. CNS Spectr. 2007; 12: 359–375. Hollander E, Friedberg JP, Wasserman S, Yeh CC, Iyengar R. The case for the OCD spectrum. In: Abramowitz JS, Houts AC, eds. Handbook of Controversial Issues in Obsessive-Compulsive Disorder. Kluwer Academic Press, New York; 2005. McElroy SL, Phillips KA, Keck PE. Obsessive compulsive spectrum disorder. J Clin Psychiatry. 1994; 55: 33–51. Bottas A, Cooke RG, Richter MA. Comorbidity and pathophysiology of obsessive–compulsive disorder in schizophrenia: is there evidence for a schizo-obsessive subtype of schizophrenia? J Psychiatry Neurosci. 2005; 30: 187–193. Pallanti S, Castellini G, Chamberlain SR, et al. Cognitive event-related potentials differentiate schizophrenia with obsessive-compulsive disorder (schizo-OCD) from OCD and schizophrenia without OC symptoms. Psychiatry Res. 2009; 170: 52–60. Pallanti S, Grassi G, Sarrecchia ED, Cantisani A, Pellegrini M. Obsessive–compulsive disorder comorbidity: clinical assessment and therapeutic implications. Front Psychiatry. 2011; 2: 70–87. Poyurovsky M, Weizman A, Weizman R. Obsessivecompulsive disorder in schizophrenia: clinical characteristics and treatment. CNS Drugs. 2004; 18: 989–1010. Kitis A, Akdede BBK, Alptekin K, et al. Cognitive dysfunctions in patients with obsessive-compulsive disorder compared to the patients with schizophrenia patients: relation to overvalued ideas. Prog Neuropsychopharmacol Biol Psychiatry. 2007; 31: 254–261. Tynes LL, White K, Steketee GS. Toward a new nosology of obsessive compulsive disorder. Compr Psychiatry. 1990; 31: 465–480. Tumkaya S, Karadag F, Oguzhanoglu NK, et al. Schizophrenia with obsessive-compulsive disorder and obsessive-compulsive disorder with poor insight: a neuropsychological comparison. Psychiatry Res. 2009; 165: 38–46. Mukhopadhaya K, Krishnaiah R, Taye T, et al. Obsessive-compulsive disorder in UK clozapine-treated schizophrenia and schizoaffective disorder: a cause for clinical concern. J Psychopharmacol. 2009; 23: 6–13. Tibbo P, Kroetsch M, Chue P, Warneke L. Obsessivecompulsive disorder in schizophrenia. J Psychiatr Res. 2000; 34: 139–146. Nechmad A, Ratzoni G, Poyurovsky M, et al. Obsessivecompulsive disorder in adolescent schizophrenia patients. Am J Psychiatry. 2003; 160: 1002–1004. Ohta M, Kokai M, Morita Y. Features of obsessive–compulsive disorder in patients primarily diagnosed with schizophrenia. Psychiatry Clin Neurosci. 2003; 57: 67–74. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 13 Poyurovsky M, Kriss V, Weisman G, et al. Comparison of clinical characteristics and comorbidity in schizophrenia patients with and without obsessivecompulsive disorder: schizophrenic and OC symptoms in schizophrenia. J Clin Psychiatry. 2003; 64: 1300–1307. Patel D, Laws K, Padhi A, et al. The neuropsychology of the schizo-obsessive subtype of schizophrenia: a new analysis. Psychol Med. 2010; 40: 921–933. Phillips KA, Pinto A, Hart AS, et al. A comparison of insight in body dysmorphic disorder and obsessive–compulsive disorder. J Psychiatr Res. 2012; 46: 1293–1299. Peralta V, Campos MS, De Jalón EG, Cuesta MJ. Motor behavior abnormalities in drug-naı̈ve patients with schizophrenia spectrum disorders. Mov Disord. 2010; 25: 1068–1076. Pulford BD, Johnson AB, Awaida M. A cross-cultural study of predictors of self-handicapping in university students. Personality and Individual Differences. 2005; 39: 727–737. Perry W, Minassian A, Henry B, et al. Quantifying overactivity in bipolar and schizophrenia patients in a human open field paradigm. Psychiatry Res. 2010; 178: 84–91. Boyer P, Lienard P. Why ritualized behavior? Precaution systems and action parsing in developmental, pathological and cultural rituals. Behav Brain Sci. 2006; 29: 595–650. Eilam D. Ritualized behavior in animals and humans: time, space and attention. Behav Brain Sci. 2006; 29: 616–617. Zor R, Hermesh H, Szechtman H, Eilam D. Turning order into chaos through repetition and addition of elementary acts in obsessive compulsive disorder (OCD). World J Biol Psychiatry. 2009; 10(4 Pt 2): 480–487. Zor R, Keren H, Hermesh H, et al. Obsessive-compulsive disorder (OCD): a disorder of pessimal (non-functional) motor behavior. Acta Psychiatr Scand. 2009; 120: 288–298. Eilam D, Zor R, Fineberg N, Hermesh H. Animal behavior as a conceptual framework for the study of obsessive-compulsive disorder (OCD). Behav Brain Res. 2012; 231: 289–296. Jenike MA. Illnesses related to obsessive-compulsive disorder. In: Jenike MA, Baer LB, Minichiello WE, eds. Obsessive Compulsive Disorders: Theory and Management. Chicago: Year Book Medical; 1990: 39–60. Graybiel AM, Rauch SL. Toward a neurobiology review of obsessive-compulsive disorder. Neuron. 2000; 28: 343–347. Keren H, Boyer P, Mort J, Eilam D. Pragmatic and idiosyncratic acts in human everyday routines: the counterpart of compulsive rituals. Behav Brain Res. 2010; 212: 90–95. Bowie CR, Harvey PD. Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin North Am. 2005; 28: 613–633. Menzies L, Chamberlain SR, Laird AR, et al. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the 14 37. 38. A. Gershoni et al. orbitofronto-striatal model revisited. Neurosci Biobehav Rev. 2008; 32: 525–549. Kuelz AK, Hohagen F, Voderholzer U. Neuropsychological performance in obsessive-compulsive disorder: a critical review. Biol Psychol. 2004; 65: 185–236. Martin V, Huber M, Rief W, Exner C. Comparative cognitive profiles of obsessive-compulsive disorder and schizophrenia. Arch Clin Neuropsychol. 2008; 23: 487–500. 39. 40. 41. Hutton S, Puri B, Duncan LJ, et al. Executive function in first-episode schizophrenia. Psychol Med. 1998; 28: 463–473. Spitznagel MB, Suhr JA. Executive function deficits associated with symptoms of schizotypy and obsessive– compulsive disorder. Psychiatry Res. 2002; 110: 151–163. Goodman WK, Price L, Rasmussen SA, et al. The YaleBrown obsessive-compulsive scale 1. Development, use, and reliability. Arch Gen Psychiatry. 1989; 46: 1006–1011.