* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 3_Gram Negative Bacteria of Medical Importance
Survey
Document related concepts
Sociality and disease transmission wikipedia , lookup
Urinary tract infection wikipedia , lookup
Infection control wikipedia , lookup
Neonatal infection wikipedia , lookup
Vaccination wikipedia , lookup
Typhoid fever wikipedia , lookup
Hepatitis B wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
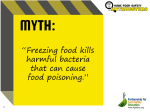
Gastroenteritis wikipedia , lookup
Globalization and disease wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
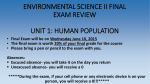
Transcript
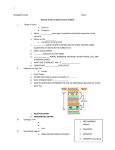
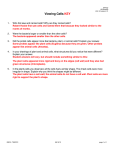
ZaidKhalid MBBS220 Gram Negative Bacteria of Medical Importance Gram Negative Bacteria Curved rods Coccus Aerobic Niesseria Moraxella Anaerobic Rods Vibrio Campylobacter Helicobacter Veillonella Aerobic Anaerobic Fastidious Oxidase Test Bacteriodes Haemophilus Porphyromonas Bordetella Prevotella Brucella Legionella Positive Negative Pseudomonas Enterobacteriacae Stenotrophomonas Burkholderia Lactose Fermenter Non-lactose fermenter Klebsiella Samonella Escherichia Shigella Eneterobacter ZaidKhalid MBBS220 COCCUS Name of Lab Characteristics bacteria Neisseria 1. Non-motile 1. Gonorrhoea 2. Diplococci 2. Meningitidis 3. Fastidious a. Capnophilic 4. Grow on a. Chocolate agar b. Thayer-Martin agar 5. Neisseria gonorrhoeae a. Enriched media with VCNT i. Vancomycin ii. Colistin iii. Nystatin iv. Trimethoprim 6. Oxidase positive 7. Encapsulated a. Meningitidis-yes b. Gonorrhoeae-no 8. Way to differentiate them a. Meningitidis – glucose+maltose b. Gonorrhoeae-glucose Virulence factors 1. Gonorrhoeae a. Pili for adhesins b. Endotoxin c. Outer membrane protein d. Protease production e. Resistance to i. Phagocytosis ii. IgA protease 2. Meningitidis a. Polysaccharide capsule b. Endotoxin c. IgA protease resistant Transmission Clinical diseases Treatment 1. Only available in human being 2. Gonorrhoeae a. Genital tract b. Nasopharynx c. Anus d. Spreads thru sexual intercourse 3. Meningitidis a. Pharynx b. Spreads thru droplets of water Gonorrhoeae 1. Gonorrhoea 2. Pelvic inflammatory disease 3. Salphingitis 4. In infant(gets from infected mom) a. Ophthalmia nonatorum Meningitidis 1. Meningitis 2. Septicaemia Gonorrhoeae 1. NonPPNG=Penicillin 2. PPNG= a. Ceftriaxone b. Spectinomycin c. Ciprofloxacin 3. No vaccine Meningitidis 1. Rifampicin for prophylaxis 2. Tetravalent vaccine available ZaidKhalid MBBS220 CURVED RODS Name of bacteria Vibrio Types of vibrio 1. Cholerae 2. Parahaemol yticus Lab Characteristics 1. Highly motile; single flagellum 2. Grow in alkaline condition a. Alkaline peptone water 3. TCBS forms a. Yellow (cholera) b. Green (parahaemolyticus) 4. Oxidase positive Name of bacteria Campylobacter jejuni Lab Characteristics 1. 2. 3. 4. Slender curved Microaerophilic Motile, polar flagellum Skirrow’s medium with antibiotic a. Incubation for 24-72 hrs at 42oC i. 5% O2 ii. 10%CO2 5. Colonies= water drops Virulence factors Transmission Clinical diseases Treatment Cholerae 1. Cholerae 1. Mucinase a. Contaminated 2. Adhesins food and water 3. Enterotoxins 2. Parahaemolyticus a. Chromosomally a. Contaminated mediated seafood and fish b. Binds to ganglioside receptors c. Activate adenyl cyclase d. Causing fluid loss e. Massive watery diarrhoea Parahaemolyticus 1. Cytotoxin Virulence factors Transmission 1. Cholerae a. Cholera 2. Parahaemolyticus a. Food poisoning 1. Fluid replacement therapy 2. Tetracycline to shorten the infection 3. Oral vaccine available 4. Prevention of cholera is based from good sanitary management 5. No specific Tx for parahaemolyticus diarrhoea Clinical diseases Treatment 1. Cytotoxin 2. Infection and destruction of gut mucosa 1. Gastroenteritis 2. Bacteremia 1. Animal reservoir 2. Contaminated food and milk 3. Person to person spread is very rare 1. No specific Tx for diarrhoea 2. Erythromycin for bacteremia 3. Good food hygiene ZaidKhalid MBBS220 Name of bacteria Helicobacter pylori Lab Characteristics 1. Spiral shape 2. Motile, multiple flagellum 3. Skirrow’s medium with antibiotic a. Incubation for 24-72 hrs at 42oC i. 5% O2 4. Microaerophilic 5. Differentiated from campylobacter by a. Nitrate reduction i. Campyl-positive ii. Helico-negative b. Urease i. Helico-positive ii. Campyl-negative Virulence factors 1. Produces a. Protease i. Modifies gastric mucus ii. Reduce ability of acid to diffuse thru mucus b. Potent urease i. Yields ammonia ii. Buffering more acid Transmission 1. Person to person transmission 2. Faecal-oral transmission 3. Infections observed in multiple family members Clinical diseases 1. 2. 3. 4. Antral gastritis Peptic ulcer Gastric ulcer Gastric carcinoma Treatment 1. PPI plus antibiotics a. Clarithromycin b. Metronidazole c. Tetracycline 2. PPI is a potent urease inhibitor 3. Triple treatment with a. Metronidazole+ Bismuth subsalicylate/ bismuth salicylate + amoxy/tetra ZaidKhalid MBBS220 RODS Aerobic/Oxidase test positive Name of bacteria Pseudomonas aeruginosa Lab Characteristics 1. Motile; polar flagella 2. Does not ferment carb 3. Grows readily in routine media, characteristic smell 4. Pigmentation a. Pyocynin i. Blue b. Pyoverdin i. Yellow c. Pyorubin i. Red d. Pyomelanin i. Black 5. Oxidase positive Virulence factors Transmission 1. Endotoxin 2. Exotoxin A 3. Extracellular polysaccharide prevent phagocytosis 4. Pigment a. Pyoverdin as siderophore 1. Found in hospital settings 2. Widespread easily in a moist area such as hospital 3. Infected thru directly or indirectly to the environment Clinical diseases 1. Opportunistic pathogens 2. Skin infection and burns 3. Cystic fibrosis 4. Pneumonia in ventilated patient 5. UTI 6. Septicaemia Treatment 1. Resistant to many antibiotic 2. Resistance develops rapidly during Tx 3. Combination antibiotic based on susceptibility test a. Aminoglycosides b. B lactam antibiotics 4. Prevention a. Good hospital aseptic technique b. Avoid unnecessary and prolonged use of antibiotic ZaidKhalid MBBS220 RODS Aerobic/Oxidase test Negative Lactose fermenter Name of bacteria Escherichia coli Lab Characteristics 1. 2. 3. 4. 5. 6. Motile Sometimes encapsulated Facultative anaerobe Bile tolerant Grows well in blood agar Ferments lactose a. Pink- McConkey agar b. Yellow-CLED 7. Commercial kit-API 20E Virulence factors 1. Powerful toxin 2. Enterotoxin (coded on plasmids) a. Heat sensitive b. Heat labile 3. Colonization factor antigen 4. Plasmid coded pili 5. Verotoxin that can cause haemorrhagic diarrhoea Name of bacteria Klebssiella sp. Enterobacter sp. Serratia sp. Transmission 1. Endogenous 2. Exogenous Clinical diseases 1. Types of E.coli can cause diarrhoea a. Enteropathogenic (EPEC) b. Enteroinvasive (EIEC) c. Enterotoxigenic (ETEC) d. Enterohaemorrhagic (EHEC) e. Enteroaggregrative (EAEC) 2. UTI Explanation 1. Found in human a. Intestine b. Respiratory tract 2. Nasocomial infection in immunocompromised pts on a. Ventilator b. IV catheter 3. Serratia marcescens a. Produces magenta colony b. Fatal to i. Neonates ii. Immunocompromised pts iii. Debilitated pts ZaidKhalid MBBS220 RODS Aerobic/Oxidase test Negative Non-Lactose fermenter Name of bacteria 1. Salmonella a. Typhi b. Parathypi Name of bacteria Shigella 1. Dysnteriae 2. Sonnei 3. Flexneri 4. Boydii Lab Characteristics 1. Motile 2. Non-forming spore 3. Salmonella typhi is NONCAPSULATED 4. Facultative anaerobes 5. Non-lactose fermenter Lab Characteristics 1. No – motile 2. Noncapsulated 3. Non lactose fermenter ; sonnei slow lactose fermenter 4. Commercial kits of API20e Virulence factors 1. Antigen O –somatic 2. Antigen H – flagellum 3. Antigen Vi – virulence, notably found in typhi Virulence factors 1. Invade ileum and colon 2. Intense inflammatory response, bloody diarrhoea 3. Exotoxin is neurotoxin Clinical diseases 1. Enteric fever a. Typhoid fever b. Paratyphoid fever 2. Gastroenteritis a. Due to salmonella enteritidis b. Due to the consumption of highly contaminated i. Food ii. Beverage 3. Septicaemia a. Fatal disease b. Pneumonia, meningitis and osteomyelitis are secondary Transmission Clinical diseases 1. Live only in 1. Dysentery human intestines 2. Feacal-oral in crowded area 3. Minute dose of organisms can cause disease Treatment 1. Proper cooking a. Food form animal resources 2. Typhoid fever vaccine a. Killed salmonella typhi suspension b. Oral attenuated salmonella typhi TY21a Treatment 1. Fluid and electrolyte replacement Tx 2. Antibiotics should be avoided; multiple resistant found 3. Personal hygiene and proper sanitation ZaidKhalid MBBS220 RODS Anaerobic Name of bacteria Bacteriodes fragilis Lab Characteristics 1. Pleomorphic coccobacilli 2. Blood agar, incubated anaerobically a. Kept for 48hrs at 37oC for them to be visible 3. Have foul odour, fatty acid Virulence factors 1. Polysaccharide capsule 2. Extracellular enzyme Transmission 1. Contamination of gut contents /faeces Clinical diseases 1. 2. 3. 4. 5. Intra-abdominal sepsis Liver abscesses Aspiration pneumonia Brain abscesses Wound infection Treatment 1. Metronidazole 2. B lactam antibiotic resistant 3. Surgical technique can be employed ZaidKhalid MBBS220 RODS Fastidious Name of bacteria Haemophilus sp 1. Influenzae 2. Ducreyi Live in human upper respiratory tract Name of bacteria Bordetella pertussis Lab Characteristics Virulence factors 1. Identification 1. Polysaccharide a. Influenzae capsule i. Factor X (+) 2. Endotoxin ii. Factor V (+) 3. Outer b. Ducreyi membrane i. Factor X (+) protein ii. Factor V (-) 2. Coccobacilli 3. Capnophilic 4. Encapsulated 5. Grows on chocolate agar 6. Larger colonies with S. Aureus 7. Type b antigen is pathogenic Lab Characteristics 1. Slow growing 2. Fastidious 3. Grows on enriched media a. Bordet-Gengou media b. Blood charcoal agar 4. Identify by specific antisera Virulence factors 1. Tracheal cytotoxin 2. Fimbrial antigen 3. Lymphocytic promoting factor Transmission 1. Person to person; airborne Transmission 1. Airborne spread 2. No healthy carrier documented Clinical diseases 1. Influenzae a. Meningitis b. Osteomyelitis c. Acute apiglotitis d. Otitis media 2. Ducreyi a. Chancroid/genital tract infection Clinical diseases 1. Whooping cough (pertussis) Treatment 1. Amoxicillin 2. 3rd generation cephalosporin a. Ceftriaxone 3. Children are immunized by a. H.inlfuenzae serotype b polysaccharide vaccine 4. Rifampicin for prophylaxis in H.influenzae meningitis Treatment 1. Erythromycin 2. May reduce infectivity and incidence of superinfection 3. Vaccine together with tetanus and diphtheria 4. Newer subunit vaccines are also effective ZaidKhalid MBBS220 Name of bacteria Lab Characteristics Virulence factors Transmission Clinical diseases Treatment Brucella 1. Abortus-cattle 2. Suis-pig 3. Canis-dog 4. Melitensis-goat Causing the zoonotic infection 1. Coccobacilli 2. Require complex nutrition for growth 3. Castaneda bottles containing both broth and blood 4. Requires 3-5days of incubation in CO2 enriched media, some up to 4 weeks 1. Can survive intracellular in a. Bone marrow b. Liver c. Spleen 1. Zoonotic infection a. Consumption of contaminated milk/unpasteur ised dairy product b. Direct contact; occupational hazard 1. Undulant fever a. Can be chronic if not treated adequately 1. Doxycyline alone 2. Doxycycline plus a. Streptomycin b. Rifampicin 3. Vaccination of live stocks and pasteurisation of milk Name of bacteria Lab Characteristics Clinical diseases Treatment Legionella pneumophilla 1. Pleomorphic 2. Coccobacilli 3. Need enriched media with iron and cysteine, and charcoal to remove fatty acid (BCYE) 4. Incubate for 3-5 days; produce small tenacious colonies Virulence factors 1. Intracellular survival in alveolar macrophage 2. Predisposing factors a. Smoker b. Chronic lung disease c. Immunocompromised 1. 2. 3. 4. Legionnaire disease Atypical pneumonia Pontiac disease Diagnosis based on antibody detection 1. Erythromycin plus a. Ciprofloxacin b. Rifampicin 2. No vaccine available 3. Prevention thru proper maintenance of a. Hot water b. Air cond