* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Inflammatory Pain Models
Survey
Document related concepts
Transcript
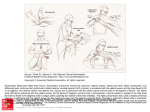
Pain Models: Ra.onale, tes.ng and interpreta.on Inflammatory Pain Models Kathryn M Albers, PhD Professor Department of Neurobiology Pain and Inflamma=on – recogni=on of neural-‐immune interac=ons Aulus Cornelius Celsus (~25 BC-‐50 BC) is credited with recording the cardinal signs of inflamma=on: dolor (pain), calor (warmth), tumor (swelling) rubor (redness and hyperaemia). De Medicina Why study inflammatory pain • Adequate pain relief for chronic pain due to inflammatory condi=ons is lacking. • Exis=ng therapies (NSAIDs, opiates) may be limited in scope and have dose-‐limi=ng side effects. • Iden=fica=on of inflammatory mediators, their temporal and spa=al ac=on and their rela=on to abnormal pain states remains unclear. What is Inflammatory Pain? • Pain associated with =ssue injury and inflamma=on (arthri=s, pancrea==s, coli=s, cys==s), autoimmune disease or exposure to irrita=ng agents. • Occurs in response to release of inflammatory mediators from injured =ssue that ac=vate and sensi=ze the nocicep=ve system…. • Causing hyperalgesia and allodynia, heat, redness, swelling of =ssue and loss of func=on. Physiological pain-‐ acute response to noxious s=muli Marchand, Perretti and McMahon. 2005. Nature Reviews Neuroscience 6:521. Inflammatory pain – =ssue damage ac=vates local and infiltra=ng immune cells. Genera=on of Inflammatory Pain PAMPs/DAMPs activate toll-‐ like receptor signaling Immune/glial cells produce algogens (ATP, bradykinin, growth factors, cytokines, lipids, serotonin, PGs) that sensi=ze nerve terminals. Ellis and Bennett. 2013 British J of Anaesthesia 111:26. Aberrant ac=vity of nociceptor neurons also drive inflamma=on through an=dromic axon reflexes that release neuropep=des at terminals. Chiu et al., (2012). Nature Neurosci 15:1063. Purpose of Inflammatory Pain Models • To understand chronic pain mechanisms at molecular, cellular, electrophysiological and anatomical levels. • To understand pathophysiological mechanisms that underlie pain in acute and chronic condi=ons. • To allow preclinical evalua=on of poten=al analgesics and therapeu=c approaches (viral vector, siRNA, cogni=ve, surgical) for blocking pain. Measure of Inflammatory Pain • Outcomes: measure of responses to applied s=muli; thermal, mechanical, chemical. • Endpoints: behavioral escape behavior, withdrawal reflex, vocaliza=on, all without =ssue damage. Assays include: – – – – – Hargreaves method Hot plate Tail flick Von Frey filaments Grip force/strength assays Nocicep=ve tests: (Hargreaves) From Barrot (2012). Tests and models of nociception and pain in rodents. Neuroscience 211:39. Inflammatory Pain Models should: • Elicit a localized inflammatory reac=on in response to a noxious chemical or surgery that provokes =ssue irrita=on – Carrageenan, CFA, zymosan, capsaicin, bee venom, formalin, mustard oil • Produce behavioral sensi=vity, primarily on treated side • Tissue swelling, redness and infiltra=on of immune cells, dependent on challenge/model. • Mimic the human inflammatory experience. Chemical/irritant induced inflamma=on models Cutaneous system Carrageenan injec=on • Sulfated polysaccharides from seaweed. • Originally developed to test activity of NSAIDs (Winter, Risley and Nuss, 1962) • Light anesthesia; Inject test compd (e.g., analgesic) 2h post hind paw injection • Produces thermal and mechanical hyperalgesia/allodynia for hours to days post injection (unless repeat injections) Peak effect 3-‐7h post injection • Strengths – Short lived but strong effect on behavioral response – Alters T cell-‐mediated immune response, edema (due to prostacyclin-‐mediated vasodilata=on) and effects are NSAID sensi=ve. • Weaknesses -‐ High dose (1 mg/IP) is immunosuppressive (block an=body produc=on, kills macrophages) -‐ Toxic to liver/kidney -‐ Promotes tumor growth. -‐ Relevance to human chronic pain? Complete Freund’s Adjuvant (CFA or FCA) • Suspension of heat-‐killed Mycobacterium butyricum or Mycobacterium tuberculosum in mineral oil diluted 1:1 with PBS. • Dual syringe used to make emulsion for injection. – Use 3-‐way stopcock between 2 syringes to emulsify Complete Freund’s Adjuvant cont. • Produces thermal and mechanical hyperalgesia and edema for days – weeks post injection. Zhang & Ren. (2011). Animal Models of Pain, Neuromethods 49:23. • Dose dependent action Increased hindpaw Decreased thermal diameter withdrawal latency • Activates immune system; robust in`iltration of immune cells in tissue. • Minimal reduction in weight, normal motor/ grooming/open `ield exploratory behavior. Strengths • Single injec=on effects changes in =ssue and behavior out to 5-‐6 days in mouse. • Repeated injec=on prolongs effect • Obvious =ssue swelling and immune cell (macrophage, PMNs) infiltra=on • Responsive to NSAID/prednisolone treatment Weaknesses • Reliability and reproducibility, par=cularly in mouse • Variable response less so in some strains (DBA/1, C57BL/6) Zymosan • Beta-‐glucan – glucose polymer from cell wall of yeast (Saccharomyces cerevisiae & Candida albicans). • Self resolving model of acute inflamma=on • Intraplantar injec=on of zymosan produces dose-‐ and =me-‐dependent hyperalgesia. • 24h thermal hyperalgesia; 3d mechanical Zymosan cont., Belichard et al (2000) Immunopharmacology. • Has associated edema/inflamma=on. • Use in cutaneous (Meller & Gebhart, 1997), visceral, muscle and nerve models Zymosan an=gens ac=vate macrophages via Dec=n-‐1 receptor. Zymosan induces immune responses that are dec=n-‐1 and TLR2-‐dependent. Dec=n-‐1 binds, internalizes glucan, media=ng produc=on of ROS and NF-‐kB ac=va=on pro-‐inflammatory cytokine/ chemokine produc=on. Strengths -‐ Zymosan acts as a PAMP. -‐ Produces thermal and mech hyperalgesia -‐ Produces spontaneous pain behaviors (30-‐45 min dura=on) -‐ Applicable to chronic pain condi=ons Candida infec=on • Pain secondary to infec=on is suspected to underlie idiopathic chronic pain condi=ons, i.e., urogenital (vulvodynia, endometriosis, prosta==s), inters==al cys==s, and IBS. • Repeated or extended C. albicans (or zymosan) infec=on in mouse inflammatory response and persistent mechanical sensi=vity of vulva. Sci Transl Med 2011 3:101. Formalin test • Protein cross-‐linking agent. • Ac=vates TRPA1 ion channel • Considered a short-‐term inflammatory pain model. Interphase depression 2: licking, biting, shaking 1: elevation 0: no elevation Tonic, in`lammatory phase (partly dependent on 1st phase) Strengths – Fast ac=ng – Produces spontaneous pain behaviors – Used to study analgesics, e.g., opioids suppress both phases, NSAIDs only effec=ve in 2nd phase Weaknesses – Poor reliability and reproducibility in producing thermal and mechanical hyperalgesia. – Typically without edema – Relevance of phasic response to human chronic pain condi=ons Capsaicin • Ac=vates TRPV1 receptors • Model of neurogenic inflamma=on, produces hyperalgesia, allodynia and neurogenic inflamma=on • Primary site of injec=on plus flare zone involvement • Decreases heat and mechanical latencies in a dose-‐dependent manner Strengths – Allows mechanis=c studies of TRPV1, primary afferent signaling, desensi=za=on, neurogenic inflamma=on…. – Produces central changes in dorsal horn neurons, glia Weaknesses – Complex biology – not specific to pain neurons – Neurotoxin – An=-‐tumor ac=on – An=-‐inflammatory ac=on?? • Fernandes et al (2012) TRPV1 dele=on enhances local inflamma=on and accelerates the onset of systemic inflammatory response syndrome. J Immunol 188:5741. Ren and Dubner, 1999. ILAR J 40:111. Cutaneous injec=on of individual or mixed algogens: Growth factors – NGF, TNF Bradykinin, histamine, leukotrienes Cytokines Prostaglandins Serotonin Substance P Muscle/Joint Pain • Deep =ssue is a major site of injury, inflamma=on (e.g., rheumatoid arthri=s) and degenera=ve disease (osteo arthri=s). • In contrast to cutaneous, the major sensa=on from deep =ssue is pain; dull, aching and poorly localized. • Myosi=s, twis=ng, hipng or compression of muscle/ joint (ligaments and fibrous capsule) evokes pain. • Low back pain, fibromyalgia and myofascial pain are considered muscle pain disorders. Muscle afferents • Fiber types – Group Ia, II – proprioceptors (muscle spindle) – Group III –thinly myelinated Ad fibers – Group IV -‐ unmyelinated C fibers • III and IV respond to metabolite (chemosensi=ve), thermo-‐ and mechano s=muli. • Innervate vasculature of muscle, CT stroma Models of Muscle Inflamma=on • Carrageenan injec=on into gastrocnemius muscle produces pain, inflamma=on, reduced grip strength. • Mustard oil injec=on into deep masseter or tongue muscle of the rat. • CFA injec=on into masseter produces persistent inflamma=on (and c-‐fos). • Injec=on of immune modulators (IL6, TNF, PGs, BK) or metabolites (ATP, lactate, protons). Muscle pain models cont., • Repeated injec=ons of pH4 saline. Causes mech allodynia without inflamma=on. • Exercise induced – Exercise plus acid, e.g., pH 5 saline injec=ons with 2h wheel running. • Prolonged ischemia (15-‐60 min) Kehl and Fairbanks. (2003)31:188. Zhang and Ren Models of inflammatory disease states of the joints Neugebauer et al., 2007. Techniques for assessing knee joint pain in arthri=s. Molecular Pain. Gregory et al., (2012) A review of transla=onal animal models for knee osteoarthri=s. Arthri=s doi:10.1155/2012/764621. Arthri=s – a prevalent, chronic disease; leading cause of disability. OA – most common form of arthri=s. Car=lage on the ends of bones wears away, overgrowth of bone. Movement/weight bearing pain is defining feature of OA. RA-‐ autoimmune disease, inflamma=on of joint connec=ve =ssues (i.e., synovial membrane). Pain, swelling and joint erosion over =me. Pain improves with movement. Gout – uric acid crystal accumula=on in joints Models of osteoarthri=s disease • Spontaneous/strain speci`ic (ColA21 KO mouse; Dunkin-‐ Hartley guinea pig ) • Chemical induction • intra-‐articular injection of papain or monosodium iodoacetate (MIA); inhibits chrondrocyte metabolism. • Injection of collagenase to damage ligaments and tendons. • Surgical induction • Meniscextomy combined with cut of collateral and/or cruciate ligaments femur tibia Models of acute inflammatory OA • Injec=on of kaolin(clay)/carrageenan into knee joint – Produces a use-‐dependent monoarthri=s within hours, car=lage damage, synovial inflamma=on. Persists for weeks. – Pathological, behavioral, electrophysiological changes, persists for weeks – Used in mouse, rat, cat, non-‐human primates • Carrageenan alone – milder phenotype OA models cont., • Zymosan – acute vascular permeability, edema, neutrophil infiltra=on. Persists for weeks leading to synovi=s (macrophage, lymphocytes), fibrovascular =ssue. • CFA into knee – single or repeated injec=on. Monoarthri=s with synovial hypertrophy, neutrophils, erosion of car=lage and bone. • CFA tail injec=on induces polyarthri=s/systemic disease and is not a good model for pain assessment. Gout models • Injec=on of monosodium urate crystals dissolved in saline • Uric acid in mineral oil • Knee joint inflamma=on within 2-‐3h that resolves aqer 3-‐7 days. Summary of knee joint pain models Gregory et al., (2012) A review of transla=onal animal models for knee osteoarthri=s. Arthri=s doi:10.1155/2012/764621. Measure of knee joint pain Indirect -‐ weight bearing – sta=c and dynamic -‐ foot posture, gait analysis -‐ spontaneous mobility – uses telemetry or ac=vity box -‐ sensi=vity to mechanical or thermal s=muli on foot of affected side Direct -‐ sensi=vity to mechanical (compression) or thermal s=muli -‐ knee extension angle measures -‐ vocaliza=on evoked by knee s=mula=on OA Model and Drug Development • An=-‐NGF Does not alter CFA-‐ induced histopathology of knee joint… Or CFA-‐induced hypervasculariza=on Ghilardi et al (2012) Arthritis and Rheumatism. 64:2223. An=-‐ngf does reduce CFA-‐induced sprou=ng of sensory and sympathe=c fibers And reduces pain-‐related behaviors Anti-‐NGF (Tanezumab) relieves OA pain experience while walking in a dose dependent manner. Which inflammatory pain model is best? Depends on: • The ques=on being asked: – Mechanis=c – Tissue/disease specific – Therapeu=c • If effect being study (e.g., new therapeu=c) targets acute or chronic pain. Does drug have acute affect or require days of treatment? • Pathophysiology – =ssue dependence; cutaneous, muscle, joints, visceral. • Cost and feasibility • Ul=mate transla=on of findings to clinic