* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Age prevalence of H. pylori in Western countries
Traveler's diarrhea wikipedia , lookup
Atherosclerosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Germ theory of disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Kawasaki disease wikipedia , lookup
Chagas disease wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Appendicitis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Infection control wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Behçet's disease wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Gastroenteritis wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Inflammatory bowel disease wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
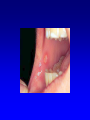
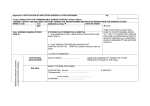
Management of Acute Severe Colitis Dr Jayne Eaden Consultant Gastroenterologist, UHCW Symptoms • Bloody diarrhoea (urgency & tenesmus) • Abdominal pain • Weight loss • Obstructive symptoms • Abdominal mass (esp RIF) Warning Signs • Fever > 37.8 oC • Dehydration – Tachycardia (P>90), Hypotension • Abdominal pain and tenderness (beware toxic dilatation and perforation) • Patients can look well if been on steroids - beware Other Signs • • • • • • Mouth ulcers Perianal disease Erythema nodosum Pyoderma gangrenosum Eye disease Arthropathy (large joints, asymmetrical and non-deforming) Truelove & Witts Criteria Defines severe Ulcerative Colitis Bowels open > 6 times per 24 hours Plus any one or more of the systemic manifestations • Haemoglobin < 10.5 • ESR > 30 • Pulse rate > 90 • Temperature > 37.5 Differential Diagnoses • Bacterial infection – C. diff, Campylobacter, Salmonella, Shigella, E. coli 0157 • Viral infection if immuno-compromised (CMV) • Amoeba especially if travel history • Crohn’s colitis and ischaemia • Diverticulitis can occasionally mimic Investigations on Admission Bloods • FBC • ESR & CRP • U&E, creat • LFT (albumin) • Blood cultures (if temp > 38°) • Glucose • (Mg+ and Cholesterol) Investigations on Admission • Stool Culture and Microscopy • C. Diff (3 separate samples) • AXR: look for stool-free colon (indicates extent involved); severe disease indicated by mucosal oedema (thickened wall), mucosal islands, dilated small bowel loops, colonic dilatation (diameter > 6cm) • Inform the surgeons on call if the colon is dilated Colectomy more likely if: -Mucosal islands present -Dilated small bowel loops Investigations on Admission • Arrange a sigmoidoscopy and rectal biopsy. DO NOT prescribe bowel prep – should be done within 24 - 48 hours of admission • Avoid colonoscopy and barium enema in patients with acute, severe colitis Daily Investigations • Bloods – FBC – U&E, creat (particularly watch the potassium) – LFT – CRP (a vital prognostic guide) • AXR for severe extensive colitis (any of fever, tachycardia, tenderness, dilatation on initial films) – in absence of these criteria less frequent AXR is OK • Results must be reviewed the same day (esp potassium) particularly if abdominal X-ray is requested. Extra Investigations • In appropriate patients, send Amoebic Fluorescent Antibody test • Check CMV titre if patient is not responding after 3 days (EDTA sample) Daily Monitoring • Temperature and pulse • Stool chart – Frequency – Colour / blood content – Estimate of volume (record even if only passed blood or mucus) • Abdo examination findings – tenderness, bowel sounds • Note increasing pulse / temp / abdominal pain or tenderness may indicate deterioration or frank perforation and requires appropriate urgent investigation and d/w SpR / consultant. Management • Rehydrate with IV fluids • Correct electrolyte imbalance (in particular potassium) • Nutrition : Low residue diet (IV fluids if vomiting) • Inform colorectal surgeons & IBD nurse Management • Corticosteroids: Hydrocortisone 100mg QDS IV until remission achieved. May use Predsol/Predfoam PR once or twice per day (mainly for distal disease) • Antibiotics (if febrile / toxic dilatation) • Severely anaemic patients (Hb < 9g / dl) should be considered for transfusion • DVT prophylaxis e.g enoxaparin 40mg od Management • Look for and treat proximal constipation • If stop 5-ASA, restart on discharge DO NOT • Use opiates / codeine phosphate/ loperamide (may precipitate paralytic ileus, megacolon and proximal constipation) • Use anti-cholinergics Travis Criteria After three days of intravenous hydrocortisone, the presence of either • Stool frequency > 8 times per 24 hours or • Stool frequency > 3 times + CRP > 45 gives an 85% likelihood of requiring colectomy on the same admission The Management of Acute Severe UC: options for rescue....... If no improvement by day 3 make plans for day 5! – Surgery or – Cyclosporine or – Infliximab • MUST be discussed with a Consultant Gastroenterologist Indications for colectomy • Toxic dilatation with failure to improve clinically / radiologically within 24 hrs • Perforation • Uncontrolled lower GI haemorrhage • Failure to respond after 3 days IV steroids • Deterioration at any stage Acute severe UC: the role of cyclosporine • Only use if stool cultures negative • Toxic drug – safety is paramount – IV hydrocortisone is continued – Check Mg+ and ensure cholesterol >3 – Be aware of side effects (seizures) – Care in elderly / hypertensive / impaired renal function Acute severe UC: the role of cyclosporine What dose? • 2mg/kg as IV infusion in 500mls glucose over 2-6 hrs • Monitor levels (100-200mcg/l trough) – Levels monitored at UHCW Mon-Fri • Rapid steroid wean once clinical response • If responded switch to oral after 3-5 days: – 5mg/kg/day in 2 divided doses Acute severe UC: the role of cyclosporine – long term outcome • Clinical experience from Oxford – 76 pts from 1996-2003 followed 2.9 yrs – 54 received 4mg/kg, 22 oral 5mg/kg – 74% entered clinical remission and left hospital – BUT 65% relapse at 1 yr, 90% at 3 yrs – 58% of those came to colectomy at 7 yrs Acute severe UC: the role of cyclosporine – exit strategy • Azathioprine naive vs refractory........ • • • • Ideally check TPMT levels on admission Commence Azathioprine at discharge Wean off Cyclosporine after 6-8 weeks Septrin 960mg alt days – prophylaxis against opportunistic infection • Early follow up to check remission and bloods Acute severe UC: the role of infliximab – safety issues • Possible risk of lymphoma & malignancy – Increased if pt on other immunosuppressants • Infectious complications (VZV, candida) – Serious in 3% • TB reactivation (PPD & CXR required prior to treatment) • Interactions tacrolimus / live vaccines Acute severe UC: the role of infliximab – safety issues • Contraindications: – Sepsis – Significantly raised LFTs (x3), – Hypersensitivity to infliximab – Active TB – Pregnancy } avoid for 6 months after – Breast Feeding } stopping treatment • Cautions: – Previous TB – Hepatic Impairment – Renal Impairment – Heart Failure – Mouse allergies – > 14 weeks since last infusion Infliximab for chronic active UC: can we predict who will respond? • Serum albumin <30g/l: 67% vs 23% colectomy OR 6.86 (1.03-45.6) p=0.05 (Lees et al APT 2007) • No effect of smoking status, age, stool frequency or disease extent Management of acute severe UC: summary of evidence • Acute severe UC requires specialist care within an experienced MDT • Confirm diagnosis and exclude infection • Non responders should be identified early and salvage therapy considered • Controlled trials of cyclosporine vs infliximab are awaited Management of acute severe UC: a multi disciplinary model Physicians Surgeons Theapproach Combined Patient Nurses Radiologists Dieticians Pathologists Pharmacists