* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dipeptidyl peptidase4 inhibitors in the treatment of type 2
Survey
Document related concepts
Discovery and development of direct Xa inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of dipeptidyl peptidase-4 inhibitors wikipedia , lookup
Transcript
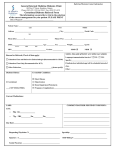
Diabetes, Obesity and Metabolism 13: 7–18, 2011. © 2010 Blackwell Publishing Ltd Dipeptidyl peptidase-4 inhibitors in the treatment of type 2 diabetes: a comparative review C. F. Deacon Department of Biomedical Sciences, University of Copenhagen, Panum Institute, Copenhagen N, Denmark The dipeptidyl peptidase (DPP)-4 inhibitors are a new class of antihyperglycaemic agents which were developed for the treatment of type 2 diabetes by rational drug design, based on an understanding of the underlying mechanism of action and knowledge of the structure of the target enzyme. Although they differ in terms of their chemistry, they are all small molecules which are orally available. There are some differences between them in terms of their absorption, distribution, metabolism and elimination, as well as in their potency and duration of action, but their efficacy, both in terms of inhibiting plasma DPP-4 activity and as antidiabetic agents, appears to be similar. They improve glycaemic control, reducing both fasting and postprandial glucose levels to lower HbA1c levels, without weight gain and with an apparently benign adverse event profile. At present, there seems to be little to distinguish between the different inhibitors in terms of their efficacy as antidiabetic agents and their safety. Long-term accumulated clinical experience will reveal whether compound-related characteristics lead to any clinically relevant differences. Keywords: alogliptin, antidiabetic drug, diabetes mellitus, DPP-4, GLP-1, glycaemic control, incretin, linagliptin, saxagliptin, sitagliptin, vildagliptin Date submitted 14 July 2010; date of first decision 8 September 2010; date of final acceptance 14 September 2010 Introduction Therapies for type 2 diabetes (T2DM) based on the actions of the incretin hormone, glucagon-like peptide-1 (GLP-1), were first introduced in 2005. GLP-1 is an intestinal hormone, which has been shown to play an important role in the normal regulation of glucose homeostasis. It has a number of effects that contribute to the maintenance of glucose tolerance, such as improvements in α- and β-cell function, including the glucosedependent stimulation of insulin and suppression of glucagon secretion, as well as non-pancreatic effects such as delaying gastric emptying and suppression of appetite [1]. These actions are preserved in patients with T2DM, and the first clinicalproof-of-concept study, published in 2002, showed that GLP-1 could reduce HbA1c levels in T2DM patients when given by continuous subcutaneous infusion [2]. GLP-1 is, however, a labile peptide and is rapidly removed from the circulation by a combination of degradation and renal clearance. The enzyme that is responsible for the initial cleavage of GLP-1 (whereby it loses its insulinotropic action) in vivo is the serine protease dipeptidyl peptidase (DPP)-4. The identification of its key role in the metabolic clearance of GLP-1 in humans provided the rationale for inhibiting the enzyme (in order to increase the levels of endogenous intact GLP-1) as a therapy of T2DM [3]. Preclinical studies showing that DPP-4 inhibition could prevent the degradation of GLP-1 in vivo, leading to increased insulinotropic activity [4], were followed Correspondence to: Carolyn F. Deacon, Department of Biomedical Sciences, University of Copenhagen, Panum Institute, Blegdamsvej 3, DK-2200 Copenhagen N, Denmark. E-mail: [email protected] by the first demonstration in humans, that a DPP-4 inhibitor could improve glycaemic control in subjects with T2DM [5]. The principle of using DPP-4 inhibitors as therapy of T2DM [1,6] is now firmly established, and numerous inhibitors are in varying stages of clinical development, with four already approved: sitagliptin in 2006, vildagliptin in 2007 and more recently, saxagliptin in 2009 and alogliptin in 2010 (presently only in Japan). The purpose of this article is to review briefly the five leading compounds in the DPP-4 inhibitor class (sitagliptin, vildagliptin, saxagliptin, alogliptin and linagliptin, currently in phase 3 clinical development), with special emphasis on any features which may help to distinguish between them. Chemistry As a therapeutic class, the DPP-4 inhibitors comprise a diverse group of compounds, which can be broadly divided into those that mimic the dipeptide structure of DPP-4 substrates and those which are non-peptidomimetic. Compounds such as sitagliptin (β-amino acid based) [7–9], and vildagliptin [10–12] and saxagliptin [13,14], which are nitrilecontaining inhibitors, belong to the former class, whereas alogliptin (modified pyrimidinedione) [15,16] and linagliptin (xanthine-based) [17,18] are members of the latter (figure 1, Table 1). The compounds which have been developed for therapeutic use are all competitive reversible inhibitors, which display high affinity for DPP-4, resulting in inhibition constants (Ki ) in the low nanomolar range [13,19–21]. There are, however, differences in the way in which they interact with the enzyme. review article review article review article DIABETES, OBESITY AND METABOLISM Figure 1. Structures of dipeptidyl peptidase (DPP)-4 inhibitors approved or in late stage clinical development. Thus, sitagliptin, alogliptin and linagliptin form non-covalent interactions with residues in the catalytic site [7,15,17]. In contrast, inhibition of DPP-4 by vildagliptin and saxagliptin has been described as a two-step process that involves the formation of a reversible covalent enzyme–inhibitor complex in which there is a slow rate of inhibitor binding and a slow rate of inhibitor dissociation, resulting in the enzyme slowly equilibrating between the active and inactive forms [22–24]. This means that the catalytic activity will be inhibited even after the free drug has been cleared from the circulation and may help to explain why vildagliptin and saxagliptin inhibit DPP-4 activity for longer than their relatively short half-lives would suggest. This may have repercussions in terms of their durations of action and dosing frequencies (see below). Potency and DPP-4 Inhibitory Efficacy Although the described DPP-4 inhibitors are all competitive reversible inhibitors, it can be difficult to compare them using data reported in individual studies, because these are influenced by differences in the assay conditions used to estimate the extent of DPP-4 inhibition. However, one study in which the inhibitors were directly compared under identical experimental conditions reported that all five inhibitors showed similar efficacy (i.e. maximal effect) for inhibition of DPP-4 in vitro, but that there were differences in potency (i.e. amount of compound needed; IC50 = ∼1 nM for linagliptin vs. 19, 62, 50 and 24 nM, for sitagliptin, vildagliptin, saxagliptin and alogliptin, respectively) [19]. With regard to half-life, there are also differences between the various inhibitors. Vildagliptin [12,25] and saxagliptin [14,26] are cleared from the plasma relatively quickly, whereas sitagliptin [9,27], alogliptin [28] and linagliptin [29] have much longer survival times (Table 2, figure 2). These differences are reflected in the therapeutic doses, which range from 5 mg for saxagliptin to 100 mg for sitagliptin, and in the dosing frequency (once daily for most of them, twice daily for vildagliptin; Table 2). Nevertheless, despite the differences in potency, when used at their therapeutic doses, the effects of the inhibitors, in terms of the extent of DPP-4 inhibition in vivo, are broadly Table 1. Chemistry, metabolism and elimination of dipeptidyl peptidase (DPP)-4 inhibitors. Inhibitor Chemistry Metabolism Sitagliptin [7–9] β-amino acid-based Vildagliptin [10–12] Cyanopyrrolidine Renal (∼80% unchanged as parent) Renal (22% as parent, 55% as primary metabolite) Saxagliptin [13,14] Renal (12–29% as parent, 21–52% as metabolite) Alogliptin [15,16] Linagliptin [17,18] 8 Deacon Not appreciably metabolized Hydrolysed to inactive metabolite (P450 enzyme independent) Cyanopyrrolidine Hepatically metabolized to active metabolite (via P450 3A4/5) Modified pyrimidinedione Not appreciably metabolized Xanthine-based Not appreciably metabolized Elimination route Renal (>70% unchanged as parent) Biliary (>70% unchanged as parent); <6% via kidney Volume 13 No. 1 January 2011 review article DIABETES, OBESITY AND METABOLISM Table 2. Half-life, potency (dose) and dipeptidyl peptidase (DPP)-4 inhibitory efficacy of DPP-4 inhibitors. Inhibitor Compound t1/2 (h) Dosing DPP-4 inhibition∗ Sitagliptin [9,27] Vildagliptin [12,25] Saxagliptin [14,26] Alogliptin [28] Linagliptin [29] 8–24 1 1/2 –4 1/2 2–4 (parent) 3–7 (metabolite) 12–21 10–40 100 mg qd 50 mg bid 5 mg qd 25 mg qd 5 mg qd (anticipated) Max ∼97%; >80% 24 h postdose Max ∼95%; >80% 12 h postdose Max ∼80%; ∼70% 24 h postdose Max ∼90%; ∼75% 24 h postdose Max ∼80%; ∼70% 24 h postdose ∗ DPP-4 activity measured in human plasma ex vivo; not corrected for sample dilution in the assay. similar. Over 90% inhibition is attained within 15 min of inhibitor administration, with around 70–90% inhibition being sustained at 24 h postdose (Table 2, figure 2); for vildagliptin, although the extent of plasma DPP-4 inhibition drops to around 50% after 24 h with the 50 mg dose, the twice daily therapeutic dosing regimen maintains plasma DPP-4 inhibition at >80% over the full 24-h period. However, it should be pointed out that plasma DPP-4 activity is assessed ex vivo (i.e. in plasma samples taken after in vivo dosing) and is generally not corrected for the inherent dilution of the sample in the assay. Hence, the true extent of DPP-4 inhibition in vivo is probably higher than the measured values suggest. Selectivity DPP-4 is a member of a family of proteases, two of which (DPP-8 and -9) have been implicated in preclinical toxicities and suppression of T-cell activation and proliferation in some [30,31], but not all [20] studies; in order to minimize any potential off-target side effects, the inhibitors intended to be used therapeutically have, therefore, been chosen with this in mind (Table 3). Thus, in this respect, sitagliptin and alogliptin can both be described as being highly selective; they essentially show no inhibitory activity against other members of the DPP-4 family when tested in vitro [7,15]. Vildagliptin and saxagliptin are somewhat less selective with regard to inhibition of DPP-8/9 in vitro [20,21], although whether this has any significance in vivo is questionable because DPP-8/9 are located intracellularly. Linagliptin, while being selective with regard to DPP-8/9, is less selective with regard to fibroblast activation protein-α (FAPα)/seprase [19]. FAPα is an extracellular enzyme which is not generally present in normal adult tissue (although it is expressed in stromal fibroblasts and upregulated during tissue remodelling) [32]. However, the extent of any FAPα inhibition in vivo with the therapeutic dose of linagliptin in humans has not been reported. Figure 2. Extent of plasma dipeptidyl peptidase (DPP)-4 activity in humans after DPP-4 inhibitor administration. (A) Vildagliptin, modified from He et al. [25]; (B) saxagliptin, modified from Boulton et al. [26]; (C) sitagliptin, modified from Bergman et al. [27]; (D) alogliptin, modified from Covington et al. [28] and (E) linagliptin, modified from Heise et al. [29]. None of the inhibitors have been reported to have any significant inhibitory activity on a panel of different enzymes, including the CYP450 enzymes (sitagliptin [7]; vildagliptin [12]; saxagliptin [14]; alogliptin [15] and linagliptin [19]), although linagliptin was reported to inhibit CYP3A4 activity weakly in a competitive manner (Ki = 115 μM) and to be a poor-tomoderate mechanism-based inhibitor of CYP3A4 [18]. Table 3. In vitro selectivity of dipeptidyl peptidase (DPP)-4 inhibitors (fold selectivity for DPP-4 vs. other enzymes). Inhibitor Selectivity QPP/DPP-2 PEP FAPα DPP-8 DPP-9 Sitagliptin [7] Vildagliptin [10,20] Saxagliptin [21] Alogliptin [15] Linagliptin [19] High Moderate Moderate High Moderate >5550 >100 000 >50 000 >14 000 >100 000 >5550 60 000 Not reported >14 000 >100 000 >5550 285 >4000 >14 000 89 >2660 270 390 >14 000 40 000 >5550 32 77 >14 000 >10 000 QPP, quiescent cell proline dipeptidase; PEP, prolyl endopeptidase; FAPα, fibroblast activation protein-α. Volume 13 No. 1 January 2011 doi:10.1111/j.1463-1326.2010.01306.x 9 review article Absorption The DPP-4 inhibitors are all orally available and are rapidly absorbed (figure 2), with significant inhibition of plasma DPP-4 activity being seen within 5 min of administration. Oral biovailability in humans is generally high (∼87% for sitagliptin [33], 85% for vildagliptin [34] and ∼67% for saxagliptin [35]), although somewhat lower for linagliptin (∼30%) [36]. Distribution Where available, data indicate that the volume of distribution of the various inhibitors in humans is greater than the total body water (∼70 l for vildagliptin [12], 198 l for sitagliptin [9], 300 l for alogliptin [28] and ∼2.7 l/kg for saxagliptin [35]), suggesting that these compounds distribute widely into the tissues. However, although their chemistries suggest that they are unlikely to diffuse freely over the cell membrane, whether or not they actually cross the cell membrane has not been studied in detail and no information is available for sitagliptin, alogliptin or linagliptin. The intrinsic membrane permeability of saxagliptin is reported to be very low, and neither saxagliptin nor its major metabolite (BMS-510849) is a prominent substrate for multidrug resistance P-glycoprotein (Pgp) transporters or for cellular uptake transporters [26]. There is some indirect evidence that vildagliptin may be able to cross the cell membrane. Thus, it has been reported that at very high doses (>600 times the human dose), vildagliptin inhibits DPP-8/9 in vivo in rats [20]; because DPP-8/9 are located in the cytosol, this would suggest that vildagliptin does have some access to the intracellular compartment, but it is unclear whether this occurs in humans with the therapeutic dose. In the plasma, most of the inhibitors display low, reversible protein binding (38% for sitagliptin [33], 10% for vildagliptin [11,12] and negligible for saxagliptin [14]). In contrast, linagliptin binds extensively to plasma proteins in a concentration-dependent manner and it has been calculated that at the therapeutic dose (5 mg) most of the drug will be protein bound (primarily to DPP-4) [37]. Preclinical studies have revealed that the highest concentrations of the drugs are found in the intestines, kidney and liver [9,12,14,38], which, notably, are also the tissues with the highest expression of DPP-4. Available information indicates that very low levels of the inhibitors are found in the brain (saxagliptin and its primary metabolite [35], vildagliptin [12] and linagliptin [38]), suggesting that the compounds may not cross the blood–brain barrier. However, they do appear to be able to cross the placenta freely (saxagliptin [14], vildagliptin [12] and sitagliptin [9]). Metabolism Sitagliptin, alogliptin and linagliptin do not undergo appreciable metabolism in vivo in humans; around 80% of the dose is eliminated unchanged as the parent compound (Table 1). For sitagliptin, the limited metabolism produces six metabolites in trace amounts (each accounting for <1% to 7% of sitagliptin-related material in plasma), with in vitro studies indicating that the primary enzyme responsible is CYP3A4 10 Deacon DIABETES, OBESITY AND METABOLISM with a lesser contribution from CYP2C8 [8]. Three of these metabolites (M1, M2 and M5) are active, but are not expected to contribute to the pharmacodynamic profile of sitagliptin because of the combination of low plasma concentration and low affinity for DPP-4 [8,9]. For alogliptin, the parent molecule accounts for >80% of alogliptin-related material in plasma and two minor metabolites have been identified, N-demethylated (active) and N-acetylated (inactive) alogliptin, accounting for less than 1% and approximately 5%, respectively [16]. In the case of linagliptin, the parent compound made up around 70% of drug-related material in plasma, while exposure to the major metabolite (CD1790, identified as S-3-hydroxypiperidinyl derivative of linagliptin) was around 18% of that of the parent compound. Formation of CD1790, which is pharmacologically inactive, is dependent upon CYP3A4. In addition, seven minor metabolites (each accounting for 0.3 to <5% of linagliptinrelated material in plasma) were identified [18]. In contrast, both vildagliptin and saxagliptin undergo extensive metabolism in humans (Table 1). The major metabolic pathway for vildagliptin is hydrolysis at its cyano moiety, which occurs in the liver and other tissues via a CYP450 -independent mechanism, to produce a carboxylic acid metabolite (M20.7/LAY151) and four minor metabolites. The parent molecule and the major metabolite, which is pharmacologically inactive, account for the majority of vildagliptin-related material in the plasma (approximately 22 and 55%, respectively) [11,12]. Saxagliptin is hepatically metabolized by CYP 3A4/5 to produce a major metabolite (5hydroxy saxagliptin; BMS-510849), which is also a competitive, reversible inhibitor of DPP-4 with approximately 50% of the potency of the parent drug. Systemic exposure to saxagliptin-related material is accounted for by the parent molecule (22%) and BMS-510849 plus other unidentified minor monohydroxylated metabolites (76%) [14]. Excretion Generally, the DPP-4 inhibitors are eliminated primarily via the kidney, with the rate of renal clearance exceeding glomerular filtration, suggesting that active transport is involved. For sitagliptin, around 70% of the dose is excreted as the parent molecule and active transport has been shown to account for around 50% of its clearance [39]; the human organic anion transporter (OAT)-3, organic anion transporting polypeptide (OATP)-4C1 and Pgp transporters in the proximal tubule have been indicated to be involved [40]. Alogliptin (and its minor metabolites) is renally eliminated, with around 60–70% of the dose appearing in the urine as the parent compound [28,41]. Clearance of alogliptin is greater than normal glomerular filtration, but the renal transporters involved have not been identified, although drug-interaction studies suggest that Pgp is unlikely to be involved [28]. Similarly, both saxagliptin and its primary metabolite (BMS-510849) are primarily renally eliminated, accounting for 24 and 36% of the dose, respectively [14]. Again, renal clearance of the parent compound is greater than the glomerular filtration rate, indicating the involvement of active renal secretion, but the mechanism is unknown; saxagliptin is reported not to be a substrate for OAT1, OAT3, OATPA, OATPC, OATP8, organic cation transporter Volume 13 No. 1 January 2011 DIABETES, OBESITY AND METABOLISM (OCT)-1, OCT2, sodium taurocholate co-transporting peptide or peptide transporters (PepT1 and PepT2) [14]. In contrast, clearance of BMS-510849 is similar to the glomerular filtration, suggesting that this is a main mechanism involved in its elimination [14]. Data for vildagliptin also indicate the kidneys to be the predominant route of elimination, with 22% of the dose appearing in the urine unchanged and 50% appearing as the major metabolite (M20.7); active transport in addition to glomerular filtration was indicated to be involved in the elimination of both compounds [11]. Linagliptin is the exception, with <6% of the dose being excreted in the urine [29]. This may be, at least in part, because of the high degree of protein binding [37], meaning that the drug escapes glomerular filtration. Rather, linagliptin has a hepatic route of elimination, with 78% appearing in the faeces unchanged. Renal excretion of the primary metabolite (CD1790) is negligible; this undergoes further metabolism and is also eliminated in the faeces [18]. Potential for Drug–Drug Interactions In general, the DPP-4 inhibitors have not been reported to result in any meaningful activation or inhibition of the CYP enzyme system, suggesting that they are unlikely to be involved in clinically meaningful drug interactions involving these systems. There are data suggesting that there is no great propensity for the DPP-4 inhibitors to be involved in any clinically relevant drug–drug interactions with other commonly prescribed medications [9,12,14], including metformin [42–45], pioglitazone [46–48], rosiglitazone [49], glyburide [46,47,50] and simvastatin [51–53], suggesting that these agents can be co-administered with the DPP-4 inhibitors without the need for dose adjustment of either drug. As mentioned, CYP3A4/5 is involved in the conversion of saxagliptin to the active metabolite (BMS-510849), and strong inhibitors of CYP3A4/5, such as ketoconazole, increase the exposure to the parent compound. For this reason, dose reduction by half (2.5 mg qd) is recommended when saxagliptin is co-administered with strong CYP3A4/5 inhibitors [54]. Linagliptin is also a substrate for CYP3A4, and ketoconazole prevents the generation of the metabolite, CD1790. However, because this is of only minor importance in the clearance of linagliptin, inhibition or induction of CYP3A4 by concomitantly administered drugs was not considered likely to alter the overall exposure to linagliptin [18]. Additionally, linagliptin has been identified as a weak competitive and a poor-tomoderate mechanism-based inhibitor of CYP3A4, resulting in a decrease in the clearance of other compounds metabolized by this pathway by less than twofold; linagliptin was therefore considered to have only a weak potential for clinically relevant interactions with drugs metabolized by this system [18]. Safety/Tolerability Some differences between the different DPP-4 inhibitors have arisen from preclinical safety studies and observations made during the course of the clinical trial programmes. Thus, vildagliptin and saxagliptin, but not sitagliptin or alogliptin, were reported to be associated with adverse skin Volume 13 No. 1 January 2011 review article toxicology in monkeys. However, this may be a finding which is specific to monkeys, as it has not been observed in other preclinical species, and importantly, there have been no reports of skin problems in the clinical trials with any of the inhibitors [12,14,55–57]. For saxagliptin, small, reversible, dose-dependent reductions in absolute lymphocyte count have been noted in some of the clinical trials, but this has not been reported for the other DPP-4 inhibitors. The effect was more apparent at saxagliptin doses ≥20 mg (which is greater than the therapeutic dose), but values still remained within normal limits [14,58]. There was no effect on white blood cell or neutrophil count and no evidence of altered immune function. At present, the clinical significance of this (if any) remains unknown. At the time of initial registration of vildagliptin (in EU), a meta-analysis of the clinical trial data revealed that the 100 mg qd dose was associated with small numerical elevations in liver transaminases compared to placebo or 50 mg bid. For this reason, the recommended therapeutic dose was changed to 50 mg bid, with the recommendation that liver function tests be performed before initiation and at three monthly intervals for the first year of treatment and periodically thereafter [12,59]. Subsequently, the trend for mild increases (greater than three times the upper limit of normal) in liver enzymes was confirmed in the larger pooled safety analysis, but notably, this was not associated with any increased incidence of actual hepatic adverse events [56]. Nevertheless, liver function tests are still recommended and vildagliptin is not approved for use in patients with hepatic insufficiency (see later). Despite the above observations, overall, the DPP-4 inhibitors as a class appear to be very well tolerated, and rates of adverse effects have been low, and generally not different to placebo or comparator. An early meta-analysis of incretinbased therapies (in which inhibitor data were available only for sitagliptin and vildagliptin) did, however, suggest that there was an increased risk of some infections (urinary tract infections with both inhibitors and nasopharyngitis more evident with sitagliptin) and headache (more evident with vildagliptin) [60,61]. Since then, updated safety analyses (each >10 000 patients, exposed for up to 2 years) of the sitagliptin and vildagliptin clinical trials have been published, showing no increased risk for urinary tract or respiratory infections or headache (and indeed, no increased risk of any other adverse effect) with the DPP-4 inhibitors compared to placebo or comparator [55,56]. Notably, recent debate over potential links between some antidiabetic medications and cancer [62] or bone fracture [63] does not seem to extend to the DPP-4 inhibitors, with no evidence for increased signals being observed in the safety analyses [55,56]. Cardiovascular safety of new drugs, including antihyperglycaemic agents, has also been the focus of concern, with the FDA requiring pharmaceutical companies to show that new agents to not increase the risk of adverse cardiovascular events. Retrospective analyses of data from the clinical development programmes of sitagliptin, vildagliptin and saxagliptin do not appear to indicate any increased cardiovascular risk with the DPP-4 inhibitors relative to comparators [55,64,65], but large prospective trials, designed specifically to evaluate the effect of sitagliptin, saxagliptin and doi:10.1111/j.1463-1326.2010.01306.x 11 review article DIABETES, OBESITY AND METABOLISM Table 4. Prescribing characteristics of dipeptidyl peptidase (DPP)-4 inhibitors. Renal insufficiency∗ Inhibitor Sitagliptin (launched EU, USA) Vildagliptin‡ (launched EU) Saxagliptin§ (launched EU, USA) Alogliptin (launched Japan) Linagliptin (not yet approved) Mild (CrCl ≥50 ml/min) √ √ √ √ √ (likely) Hepatic insufficiency Moderate (CrCl ≥30–<50 ml/min) Severe/ESRD (CrCl <30 ml/min) Presently not recommended (EU) 1/2 dose (USA)† Presently not recommended† Presently not recommended (EU) 1/2 dose (USA)† 1/2 dose Presently not recommended (EU) 1/4 dose (USA)† Presently not recommended† Presently not recommended (EU) 1/2 dose (USA)† 1/4 dose √ √ (likely) (likely) Mild/moderate √ Not recommended √ (Moderate: use with caution) √ Unknown Dose adjustment? / not recommended? Severe Presently not recommended† Not recommended Presently not recommended† Presently not recommended† Unknown Dose adjustment? / not recommended? CrCl, creatinine clearance; ESRD, end-stage renal disease. ∗ Assessment of renal function recommended prior to initiation of treatment and periodically thereafter. † Not studied/no clinical experience. ‡ Assessment of hepatic function recommended prior to initiation of vildagliptin and periodically thereafter. § Dose reduction (2.5 mg) when saxagliptin co-administered with strong cytochrome P 450 3A4/5 inhibitors (e.g. ketoconazole). alogliptin on cardiovascular outcomes are underway. There has also been some debate over whether incretin-based therapies, including the DPP-4 inhibitors, are associated with elevated risk of pancreatitis [66]. This does not seem to be borne out by the pooled safety analyses [56,67] or retrospective analyses of large healthcare data bases [68,69]. Continued vigilance and longer term reports are still needed to confirm these observations. Use in Patient Subpopulations Renal Insufficiency Because most of the described DPP-4 inhibitors are eliminated renally, it might be expected that their pharmacokinetic profile would be influenced by impairments in renal function. In line with this, exposure to sitagliptin increased proportionately to the degree of renal failure, but the drug was well tolerated, even in patients with end-stage renal disease (ESRD), including those on dialysis; the fraction removed by dialysis was small (∼13% for haemodialysis started at 4 h postdose) [70]. Based on this study, it was concluded that no dose adjustment was necessary in subjects with mild renal insufficiency [creatinine clearance (CrCl) 50–80 ml/min]. However, in order to maintain plasma sitagliptin exposure comparable to that in subjects with normal renal function, in subjects with moderate renal insufficiency (CrCl 30–50 ml/min) or severe renal insufficiency (CrCl <30 ml/min)/ESRD, dose reductions of 50 and 75%, respectively, are required [70]. In T2DM patients with moderate or severe chronic renal insufficiency (including those with ESRD on dialysis), sitagliptin provided effective glycaemic control over 1 year and was generally well tolerated [71]. Exposure to vildagliptin and saxagliptin is also similarly increased in subjects with impaired renal function [12,14], and as for sitagliptin, vildagliptin is reported to be well tolerated in patients with mild renal insufficiency, with the rate of adverse events being similar 12 Deacon to comparators [56]; no data are yet available in patients with moderate or severe renal impairment (Table 4). On the bais of these observations, sitagliptin, vildagliptin and saxagliptin have been approved for use in subjects with mild renal insufficiency without dose adjustment, and where the indication is approved, sitagliptin and saxagliptin can be used in patients with moderate or severe renal insufficiency/ESRD with appropriate dose adjustment (Table 4). Alogliptin is also eliminated renally and can be used in subjects with moderate or severe renal impairment with dose reduction (Table 4). Because linagliptin is not predominantly eliminated via the kidneys, it could be anticipated that this drug might be able to be used in renal disease patients, including those with severe renal insufficiency/ESRD without the need for any dose adjustment [72]. Hepatic Insufficiency The DPP-4 inhibitors generally appear to be well tolerated in patients with hepatic impairment and there seems to be no clinically meaningful impact of hepatic insufficiency on their pharmacokinetics. Thus, in subjects with moderate hepatic impairment, exposure to sitagliptin was slightly, but nonsignificantly increased [73], whereas exposure to alogliptin was slightly decreased [74]. For vildagliptin, exposure to the parent drug showed non-significant trends to decrease in patients with mild or moderate hepatic impairment and to increase in patients with severe hepatic impairment, whereas exposure to the primary (inactive) metabolite (M20.7) increased nonsignificantly in all groups, compared with healthy subjects [75]. In line with its hepatic metabolism, saxagliptin exposure increased and that of the active metabolite (BMS-510849) decreased in subjects with hepatic impairment [14]. Overall, these studies suggested that no dose adjustment will be necessary in patients with hepatic impairment. Vildagliptin Volume 13 No. 1 January 2011 review article DIABETES, OBESITY AND METABOLISM is, however, not recommended for use in patients with hepatic insufficiency or those with pretreatment alanine aminotransferase or aspartate aminotransferase at greater than three times the upper limit of normal (because of the association of vildagliptin with mild increases in hepatic transaminases; see above). The other DPP-4 inhibitors which have been approved can be used in patients with mild/moderate hepatic insufficiency without dose adjustment (Table 4), although because hepatic impairment increases exposure to saxagliptin (in accord with its hepatic metabolism; see above), caution is required if used in subjects with moderate hepatic insufficiency [14]. At present, limited data in subjects with severe hepatic impairment mean that the DPP-4 inhibitors are currently not recommended for use in this patient group. Because the liver is the primary route of elimination for linagliptin, it could be anticipated that linagliptin may require dose adjustment or may not be recommended for use in subjects with hepatic impairment. Antidiabetic Efficacy As might be expected from their similar efficacy in inhibiting DPP-4 activity (see above), broadly speaking, the DPP-4 inhibitors all seem to show similar efficacy in lowering HbA1c levels, although it must be stressed that these are observations made in different studies and so must be interpreted with some caution (figure 3). At present, data are available only from one direct head-to-head comparison between the inhibitors, in which the efficacy of saxagliptin and sitagliptin as addon therapy in metformin-treated patients was compared [76]. This showed non-inferiority of saxagliptin to sitagliptin in terms of HbA1c lowering (−0.5 vs. −0.6% from a baseline of ∼7.7%; i.e. from 60 to 55 mmol/mol for saxagliptin vs. from 61 to 54 mmol/mol for sitagliptin) at week 18, Figure 3. HbA1c lowering efficacy of dipeptidyl peptidase (DPP)-4 inhibitors in relation to baseline HbA1c levels, as monotherapy or add-on therapy (open symbols) or initial combination therapy (closed symbols) in studies of ≥12 weeks duration (see Appendix for references). Triangle, sitagliptin (100 mg qd); circle, vildagliptin (50 mg bid or 100 mg qd); square, saxagliptin (5 mg qd); diamond, alogliptin (25 mg qd) and star, linagliptin (5 mg qd). Volume 13 No. 1 January 2011 with similar proportions of subjects (26 vs. 29%) reaching target HbA1c levels of <6.5% (<48 mmol/mol). However, in terms of the reduction in fasting plasma glucose, it did appear that there might be a small difference, with sitagliptin being more efficacious (−0.6 vs. −0.9 mmol/l; difference 0.30 ± 0.115 mmol/l, 95% confidence interval: 0.08–0.53); this could potentially be related to differences in the half-life of the compounds (Table 2, figure 2). In other direct headto-head studies, the DPP-4 inhibitors have shown similar efficacy to metformin [77,78], the sulphonylureas [79,80], the glitazones [81,82] and the alpha-glucosidase inhibitors [83]. In line with other antidiabetic agents [84], greater reductions in HbA1c are seen in subjects with higher baseline levels (figure 3). Conclusions The DPP-4 inhibitors are the first new therapeutic class of oral antihyperglycaemic drug for T2DM for many years. They were designed for the treatment of the disease based on prior knowledge of the physiology of the incretin hormone GLP-1 and an understanding of the target (DPP-4), contrasting with the development of other antidiabetic agents whose blood glucose-lowering effects were initially discovered more by chance than by design without fully knowing the underlying mechanisms (e.g. metformin, sulphonylureas and glitazones). Identification of the 3-dimensional/tertiary structure of the DPP-4 protein allowed the rational design of small molecule inhibitors which interact only with the catalytic site without interfering in any of the other functions of the DPP-4/CD26 molecule. This, together with the understanding of the role of GLP-1 in glucose homeostasis and its unique susceptibility to cleavage by DPP-4, probably accounts for the remarkable lack of adverse effects so far associated with the therapeutic use of the DPP-4 inhibitors. As a class, the DPP-4 inhibitors comprise of a group of chemically diverse compounds, which differ in terms of their potency to inhibit the DPP-4 enzyme, their duration of action and their metabolism and elimination, as well as isolated compound-specific characteristics (Table 5). They are all apparently well tolerated (side-effect profile resembles placebo) and result in clinically meaningful reductions in blood glucose (fasting and postprandial) and HbA1c levels, with minimal risk of hypoglycaemia and without weight gain—in this latter respect, they are better than all other agents except metformin and the incretin mimetics. They are used without the need for dose titration and give broadly similar HbA1c lowering efficacy to other oral antidiabetic agents; they are compatible with first-line therapy and they give predictable additivity to other agents, where they can be used without dose adjustment of either agent. At present, although there are some practical differences between the different DPP-4 inhibitors with respect to dosing frequency and their ability to be used in different patient subpopulations, there seems to be little to distinguish between them in terms of their efficacy as antidiabetic agents and their safety. Only long-term accumulated clinical experience will reveal whether compound-related characteristics lead to any clinically relevant differences. doi:10.1111/j.1463-1326.2010.01306.x 13 review article DIABETES, OBESITY AND METABOLISM Table 5. Differences and similarities between dipeptidyl peptidase (DPP)-4 inhibitors. 11. He H, Tran P, Yin H et al. Absorption, metabolism, and excretion of [14C]vildagliptin, a novel dipeptidyl peptidase 4 inhibitor, in humans. Drug Metab Dispos 2009; 37: 536–544. Differences Similarities Chemical structures In vitro selectivity Metabolism (changed/unchanged, active/inactive metabolite) Elimination (renal/hepatic) Preclinical toxicities Potency (therapeutic dose) Dosing frequency (once/twice daily) Use in patient subpopulations (e.g. impaired renal/hepatic function) Efficacy (HbA1c lowering) Tolerability Safety 12. European Medicines Agency (EMEA). Galvus (vildagliptin)—European public assessment report (EPAR)—scientific discussion. Available from URL: http://www.emea.europa.eu/humandocs/PDFs/EPAR/galvus/H771-en6.pdf. Accessed 5 July 2010. Conflict of Interest As this is a single author review, C. F. Deacon was responsible for all aspects of the manuscript. CFD has received consultancy/lecture fees from companies with an interest in developing and marketing incretin-based therapies for the treatment of type 2 diabetes (Astra Zeneca/BMS, Lilly, Merck, Novartis, Novo Nordisk, Servier). Spouse is employed by Merck and holds stock options in Merck and Novo Nordisk. References 1. Deacon CF. Therapeutic strategies based on glucagon-like peptide 1. Diabetes 2004; 53: 2181–2189. 2. Zander M, Madsbad S, Madsen JL, Holst JJ. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and betacell function in type 2 diabetes: a parallel-group study. Lancet 2002; 359: 824–830. 3. Deacon CF, Nauck MA, Toft-Nielsen M, Pridal L, Willms B, Holst JJ. Both subcutaneously and intravenously administered glucagon-like peptide I are rapidly degraded from the NH2-terminus in type II diabetic patients and in healthy subjects. Diabetes 1995; 44: 1126–1131. 4. Deacon CF, Hughes TE, Holst JJ. Dipeptidyl peptidase IV inhibition potentiates the insulinotropic effect of glucagon-like peptide 1 in the anesthetized pig. Diabetes 1998; 47: 764–769. 5. Ahrén B, Simonsson E, Larsson H et al. Inhibition of dipeptidyl peptidase IV improves metabolic control over a 4-week study period in type 2 diabetes. Diabetes Care 2002; 25: 869–875. 6. Holst JJ, Deacon CF. Inhibition of the activity of dipeptidyl-peptidase IV as a treatment for type 2 diabetes. Diabetes 1998; 47: 1663–1670. 7. Kim D, Wang L, Beconi M et al. (2R)-4-Oxo-4-[3-(trifluoromethyl)-5,6dihydro[1,2,4]triazolo[4,3-a]pyrazin-7(8H)-yl]-1-(2,4,5-trifluorophenyl) butan-2-amine: a potent, orally active dipeptidyl peptidase IV inhibitor for the treatment of type 2 diabetes. J Med Chem 2005; 48: 141–151. 8. Vincent SH, Reed JR, Bergman AJ et al. Metabolism and excretion of the dipeptidyl peptidase 4 inhibitor [14C]sitagliptin in humans. Drug Metab Dispos 2007; 35: 533–538. 9. European Medicines Agency (EMEA). Januvia (sitagliptin)—European public assessment report (EPAR)—scientific discussion. Available from URL: http://www.emea.europa.eu/humandocs/PDFs/EPAR/januvia/H722-en6.pdf. Accessed 5 July 2010. 10. Villhauer EB, Brinkman JA, Naderi GB et al. 1-[[(3-hydroxy-1-adamantyl) amino]acetyl]-2-cyano-(S)-pyrrolidine: a potent, selective, and orally bioavailable dipeptidyl peptidase IV inhibitor with antihyperglycemic properties. J Med Chem 2003; 46: 2774–2789. 14 Deacon 13. Augeri DJ, Robl JA, Betebenner DA et al. Discovery and preclinical profile of Saxagliptin (BMS-477118): a highly potent, long-acting, orally active dipeptidyl peptidase IV inhibitor for the treatment of type 2 diabetes. J Med Chem 2005; 48: 5025–5037. 14. European Medicines Agency (EMEA). Onglyza (saxagliptin)—European public assessment report (EPAR)—CHMP Assessment Report. Available from URL: http://www.emea.europa.eu/humandocs/PDFs/EPAR/ onglyza/H-1039-en6.pdf. Accessed 5 July 2010. 15. Feng J, Zhang Z, Wallace MB et al. Discovery of alogliptin: a potent, selective, bioavailable, and efficacious inhibitor of dipeptidyl peptidase IV. J Med Chem 2007; 50: 2297–2300. 16. Karim A, Bridson WE, Fleck P et al. Disposition of the dipeptidyl peptidase-4 inhibitor [14C]alogliptin benzoate ([14C]SYR-322) after oral administration to healthy male subjects (Abstract). AAPS Annual Meeting and Exposition, 9–15 November 2007. 17. Eckhardt M, Langkopf E, Mark M et al. 8-(3-(R)-aminopiperidin-1-yl)7-but-2-ynyl-3-methyl-1-(4-methyl-quinazolin-2-ylmethyl)-3,7-dihydropurine-2,6-dione (BI 1356), a highly potent, selective, long-acting, and orally bioavailable DPP-4 inhibitor for the treatment of type 2 diabetes. J Med Chem 2007; 50: 6450–6453. 18. Blech S, Ludwig-Schwellinger E, Gräfe-Mody EU, Withopf B, Wagner K. The metabolism and disposition of the oral dipeptidyl peptidase-4 inhibitor, linagliptin, in humans. Drug Metab Dispos 2010; 38: 667–678. 19. Thomas L, Eckhardt M, Langkopf E, Tadayyon M, Himmelsbach F, Mark M. (R)-8-(3-amino-piperidin-1-yl)-7-but-2-ynyl-3-methyl-1-(4-methylquinazolin-2-ylmethyl)-3,7-dihydro-purine-2,6-dione (BI 1356), a novel xanthine-based dipeptidyl peptidase 4 inhibitor, has a superior potency and longer duration of action compared with other dipeptidyl peptidase-4 inhibitors. J Pharmacol Exp Ther 2008; 325: 175–182. 20. Burkey BF, Hoffmann PK, Hassiepen U, Trappe J, Juedes M, Foley JE. Adverse effects of dipeptidyl peptidases 8 and 9 inhibition in rodents revisited. Diabetes Obes Metab 2008; 10: 1057–1061. 21. Kirby MS, Dorso C, Wang A et al. In vitro enzymologic characteristics of saxagliptin, a highly potent and selective DPP4 inhibitor with ‘‘slow binding’’ characteristic (Abstract). Clin Chem Lab Med 2008; 46: A79. 22. Brandt I, Joossens J, Chen X et al. Inhibition of dipeptidyl-peptidase IV catalyzed peptide truncation by Vildagliptin ((2S)-{[(3-hydroxyadamantan1-yl)amino]acetyl}-pyrrolidine-2-carbonitrile). Biochem Pharmacol 2005; 70: 134–143. 23. Burkey BF, Russell M, Wang K, Trappe J, Hughes TE. Vildagliptin displays slow tight-binding to dipeptidyl peptidase (DPP)-4, but not DPP-8 or DPP-9 (Abstract 0788). Diabetologia 2006; 49(Suppl. 1): 477. 24. Kim YB, Kopcho LM, Kirby MS et al. Mechanism of Gly-Pro-pNA cleavage catalyzed by dipeptidyl peptidase-IV and its inhibition by saxagliptin (BMS-477118). Arch Biochem Biophys 2006; 445: 9–18. 25. He YL, Wang Y, Bullock JM et al. Pharmacodynamics of vildagliptin in patients with type 2 diabetes during OGTT. J Clin Pharmacol 2007; 47: 633–641. 26. Boulton DW, Geraldes M. Safety, tolerability, pharmacokinetics and pharmacodynamics of once daily oral doses of saxagliptin for 2 weeks in type 2 diabetic and healthy subjects (Poster 0606-P). Diabetes 2007; 56(Suppl. 1): A161. 27. Bergman AJ, Stevens C, Zhou Y et al. Pharmacokinetic and pharmacodynamic properties of multiple oral doses of sitagliptin, a dipeptidyl Volume 13 No. 1 January 2011 DIABETES, OBESITY AND METABOLISM peptidase-IV inhibitor: a double-blind, randomized, placebo-controlled study in healthy male volunteers. Clin Ther 2006; 28: 55–72. 28. Covington P, Christopher R, Davenport M et al. Pharmacokinetic, pharmacodynamic, and tolerability profiles of the dipeptidyl peptidase-4 inhibitor alogliptin: a randomized, double-blind, placebo-controlled, multiple-dose study in adult patients with type 2 diabetes. Clin Ther 2008; 30: 499–512. 29. Heise T, Graefe-Mody EU, Hüttner S, Ring A, Trommeshauser D, Dugi KA. Pharmacokinetics, pharmacodynamics and tolerability of multiple oral doses of linagliptin, a dipeptidyl peptidase-4 inhibitor in male type 2 diabetes patients. Diabetes Obes Metab 2009; 11: 786–794. 30. Lankas GR, Leiting B, Roy RS et al. Dipeptidyl peptidase IV inhibition for the treatment of type 2 diabetes: potential importance of selectivity over dipeptidyl peptidases 8 and 9. Diabetes 2005; 54: 2988–2994. 31. Reinhold D, Goihl A, Wrenger S et al. Role of dipeptidyl peptidase IV (DP IV)-like enzymes in T lymphocyte activation: investigations in DP IV/CD26-knockout mice. Clin Chem Lab Med 2009; 47: 268–274. review article 44. Karim A, Covington P, Christopher R et al. Pharmacokinetics of alogliptin when administered with food, metformin, or cimetidine: a two-phase, crossover study in healthy subjects. Int J Clin Pharmacol Ther 2010; 48: 46–58. 45. Graefe-Mody EU, Padula S, Ring A, Withopf B, Dugi KA. Evaluation of the potential for steady-state pharmacokinetic and pharmacodynamic interactions between the DPP-4 inhibitor linagliptin and metformin in healthy subjects. Curr Med Res Opin 2009; 25: 1963–1972. 46. Serra D, He YL, Bullock J et al. Evaluation of pharmacokinetic and pharmacodynamic interaction between the dipeptidyl peptidase IV inhibitor vildagliptin, glyburide and pioglitazone in patients with Type 2 diabetes. Int J Clin Pharmacol Ther 2008; 46: 349–364. 47. Karim A, Laurent A, Munsaka M, Wann E, Fleck P, Mekki Q. Coadministration of pioglitazone or glyburide and alogliptin: pharmacokinetic drug interaction assessment in healthy participants. J Clin Pharmacol 2009; 49: 1210–1219. 33. Herman GA, Stein PP, Thornberry NA, Wagner JA. Dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes: focus on sitagliptin. Clin Pharmacol Ther 2007; 81: 761–767. 48. Graefe-Mody U, Friedrich C, Jungnik A, Dugi KA. Lack of pharmacokinetic interactions between the novel DPP-4 inhibitor linagliptin (BI 1356) and pioglitazone in healthy subjects (abstract 13). Poster presented at 38th Annual Meeting of the American College of Clinical Pharmacology, San Antonio; September 2009. 34. He YL, Sadler BM, Sabo R et al. The absolute oral bioavailability and population-based pharmacokinetic modelling of a novel dipeptidylpeptidase-IV inhibitor, vildagliptin, in healthy volunteers. Clin Pharmacokinet 2007; 46: 787–802. 49. Mistry GC, Bergman AJ, Luo WL et al. Multiple-dose administration of sitagliptin, a dipeptidyl peptidase-4 inhibitor, does not alter the singledose pharmacokinetics of rosiglitazone in healthy subjects. J Clin Pharmacol 2007; 47: 159–164. 35. Fura A, Khanna A, Vyas V et al. Pharmacokinetics of the dipeptidyl peptidase 4 inhibitor saxagliptin in rats, dogs, and monkeys and clinical projections. Drug Metab Dispos 2009; 37: 1164–1171. 50. Mistry GC, Bergman AJ, Zheng W et al. Sitagliptin, an dipeptidyl peptidase4 inhibitor, does not alter the pharmacokinetics of the sulphonylurea, glyburide, in healthy subjects. Br J Clin Pharmacol 2008; 66: 36–42. 36. Dittberner S, Duval V, Staab A, Troconiz I, Graefe-Mody U, Jaehde U. Determination of the absolute bioavailability of BI 1356, a substance with nonlinear pharmacokinetics, using a population pharmacokinetic modelling approach (abstract 1110). Poster presented at 16th Annual Meeting of the Population Approach Group in Europe, København, Denmark; June 2007. Available from URL: http://www.page-meeting.org/?abstract=1110. Accessed 5 July 2010. 51. Ayalasomayajula SP, Dole K, He YL et al. Evaluation of the potential for steady-state pharmacokinetic interaction between vildagliptin and simvastatin in healthy subjects. Curr Med Res Opin 2007; 23: 2913–2920. 32. O’Brien P, O’Connor BF. Seprase: an overview of an important matrix serine protease. Biochim Biophys Acta 2008; 1784: 1130–1145. 37. Fuchs H, Tillement JP, Urien S, Greischel A, Roth W. Concentrationdependent plasma protein binding of the novel dipeptidyl peptidase 4 inhibitor BI 1356 due to saturable binding to its target in plasma of mice, rats and humans. J Pharm Pharmacol 2009; 61: 55–62. 38. Fuchs H, Binder R, Greischel A. Tissue distribution of the novel DPP-4 inhibitor BI 1356 is dominated by saturable binding to its target in rats. Biopharm Drug Dispos 2009; 30: 229–240. 39. Herman GA, Stevens C, Van Dyck K et al. Pharmacokinetics and pharmacodynamics of sitagliptin, an inhibitor of dipeptidyl peptidase IV, in healthy subjects: results from two randomized, double-blind, placebo-controlled studies with single oral doses. Clin Pharmacol Ther 2005; 78: 675–688. 40. Chu XY, Bleasby K, Yabut J et al. Transport of the dipeptidyl peptidase-4 inhibitor sitagliptin by human organic anion transporter 3, organic anion transporting polypeptide 4C1, and multidrug resistance P-glycoprotein. J Pharmacol Exp Ther 2007; 321: 673–683. 41. Christopher R, Covington P, Davenport M et al. Pharmacokinetics, pharmacodynamics, and tolerability of single increasing doses of the dipeptidyl peptidase-4 inhibitor alogliptin in healthy male subjects. Clin Ther 2008; 30: 513–527. 52. Bergman AJ, Cote J, Maes A et al. Effect of sitagliptin on the pharmacokinetics of simvastatin. J Clin Pharmacol 2009; 49: 483–488. 53. Graefe-Mody U, Huettner S, Stähle H, Ring A, Dugi KA. Effect of linagliptin (BI 1356) on the steady-state pharmacokinetics of simvastatin. Int J Clin Pharmacol Ther 2010; 48: 367–374. 54. Onglyza prescribing information. Available from URL: http://package inserts.bms.com/pi/pi onglyza.pdf. Accessed 5 July 2010. 55. Williams-Herman D, Engel SS, Round E et al. Safety and tolerability of sitagliptin in clinical studies: a pooled analysis of data from 10,246 patients with type 2 diabetes. BMC Endocr Disord 2010; 10: 7. 56. Ligueros-Saylan M, Foley JE, Schweizer A, Couturier A, Kothny W. An assessment of adverse effects of vildagliptin versus comparators on the liver, the pancreas, the immune system, the skin and in patients with impaired renal function from a large pooled database of Phase II and II clinical trials. Diabetes Obes Metab 2010; 12: 495–509. 57. Sato K, Ozaki H, Salamon CM, Christopher RJ, Yamamoto M. Lack of dermal toxicity with the highly selective dipeptidyl peptidase-4 inhibitor alogliptin in monkeys (Abstract). Diabetes 2008; 57(Suppl. 1): A580. 58. Rosenstock J, Sankoh S, List JF. Glucose-lowering activity of the dipeptidyl peptidase-4 inhibitor saxagliptin in drug-naive patients with type 2 diabetes. Diabetes Obes Metab 2008; 10: 376–386. 42. Herman GA, Bergman A, Yi B, Kipnes M. Tolerability and pharmacokinetics of metformin and the dipeptidyl peptidase-4 inhibitor sitagliptin when co-administered in patients with type 2 diabetes. Curr Med Res Opin 2006; 22: 1939–1947. 59. Press Release, 4th February 2008: Galvus®, a new treatment for patients with type 2 diabetes, receives European approval for label update paving the way for EU launches. Available from URL: http:// www.medicalnewstoday.com/articles/95931.php. Accessed 5 July 2010. 43. He YL, Sabo R, Picard F et al. Study of the pharmacokinetic interaction of vildagliptin and metformin in patients with type 2 diabetes. Curr Med Res Opin 2009; 25: 1265–1272. 60. Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA 2007; 298: 194–206. Volume 13 No. 1 January 2011 doi:10.1111/j.1463-1326.2010.01306.x 15 review article 61. Richter B, Bandeira-Echtler E, Bergerhoff K, Lerch CL. Dipeptidyl peptidase4 (DPP-4) inhibitors for type 2 diabetes mellitus. Cochrane Database Syst Rev 2008; CD006739. 62. Pocock SJ, Smeeth L. Insulin glargine and malignancy: an unwarranted alarm. Lancet 2009; 374: 511–513. 63. Bodmer M, Meier C, Kraenzlin ME, Meier CR. Risk of fractures with glitazones: a critical review of the evidence to date. Drug Saf 2009; 32: 539–547. 64. Schweizer A, Dejager S, Foley JE, Couturier A, Ligueros-Saylan M, Kothny W. Assessing the cardio-cerebrovascular safety of vildagliptin: meta-analysis of adjudicated events from a large phase III type 2 diabetes population. Diabetes Obes Metab 2010; 12: 485–494. 65. Frederich R, Alexander JH, Fiedorek FT et al. A systematic assessment of cardiovascular outcomes in the saxagliptin drug development program for type 2 diabetes. Postgrad Med 2010; 122: 16–27. 66. Butler PC, Matveyenko AV, Dry S, Bhushan A, Elashoff R. Glucagon-like peptide-1 therapy and the exocrine pancreas: innocent bystander or friendly fire? Diabetologia 2010; 53: 1–6. 67. Engel SS, Williams-Herman DE, Golm GT et al. Sitagliptin: review of preclinical and clinical data regarding incidence of pancreatitis. Int J Clin Pract 2010; 64: 984–990. DIABETES, OBESITY AND METABOLISM inadequately controlled on metformin monotherapy. Diabetes Obes Metab 2009; 11: 157–166. 80. Nauck MA, Meininger G, Sheng D, Terranella L, Stein PP. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trial. Diabetes Obes Metab 2007; 9: 194–205. 81. Bolli G, Dotta F, Rochotte E, Cohen SE. Efficacy and tolerability of vildagliptin vs. pioglitazone when added to metformin: a 24-week, randomized, double-blind study. Diabetes Obes Metab 2008; 10: 82–90. 82. Scott R, Loeys T, Davies MJ, Engel SS. Efficacy and safety of sitagliptin when added to ongoing metformin therapy in patients with type 2 diabetes. Diabetes Obes Metab 2008; 10: 959–969. 83. Pan C, Yang W, Barona JP et al. Comparison of vildagliptin and acarbose monotherapy in patients with Type 2 diabetes: a 24-week, double-blind, randomized trial. Diabet Med 2008; 25: 435–441. 84. Bloomgarden ZT, Inzucchi SE. New treatments for diabetes. N Engl J Med 2007; 356: 2219–2220. Appendix 68. Dore DD, Seeger JD, Arnold Chan K. Use of a claims-based active drug safety surveillance system to assess the risk of acute pancreatitis with exenatide or sitagliptin compared to metformin or glyburide. Curr Med Res Opin 2009; 25: 1019–1027. List of references to studies where HbA1c lowering efficacy is included in figure 3. 69. Herrera V, Aubert R, Tully L et al. Pancreatitis in patients treated with exenatide or sitagliptin. 69th Scientific Sessions of the American Diabetes Association, 2009; Late-breaking abstract no. 10-LB. Available from URL: http://professional.diabetes.org/Abstracts Display.aspx?TYP=1&CID =74851. Accessed 5 July 2009. Sitagliptin 70. Bergman AJ, Cote J, Yi B et al. Effect of renal insufficiency on the pharmacokinetics of sitagliptin, a dipeptidyl peptidase-4 inhibitor. Diabetes Care 2007; 30: 1862–1864. 71. Chan JC, Scott R, Arjona Ferreira JC et al. Safety and efficacy of sitagliptin in patients with type 2 diabetes and chronic renal insufficiency. Diabetes Obes Metab 2008; 10: 545–555. 72. Graefe-Mody U, Friedrich C, Port A et al. Linagliptin, a novel DPP-4 inhibitor: no need for dose adjustment in patients with renal impairment (Abstract 822). Diabetologia 2010; 53(Suppl. 1): S326. 73. Migoya EM, Stevens CH, Bergman AJ et al. Effect of moderate hepatic insufficiency on the pharmacokinetics of sitagliptin. Can J Clin Pharmacol 2009; 16: e165–e170. 74. Karim A, Fleck P, Dorsey D, Zhang W, Mekki Q, Preston RA. Single-dose pharmacokinetics of alogliptin benzoate (SYR-322), a highly selective dipeptidyl peptidase-4 inhibitor, in subjects with moderate hepatic impairment (Abstract 107). J Clin Pharmacol 2007; 47: 9. 75. He YL, Sabo R, Campestrini J et al. The influence of hepatic impairment on the pharmacokinetics of the dipeptidyl peptidase IV (DPP-4) inhibitor vildagliptin. Eur J Clin Pharmacol 2007; 63: 677–686. 76. Scheen AJ, Charpentier G, Ostgren CJ, Hellqvist A, Gause-Nilsson I. Efficacy and safety of saxagliptin in combination with metformin compared with sitagliptin in combination with metformin in adult patients with type 2 diabetes mellitus. Diabetes Metab Res Rev 2010; 26: 540–549. 77. Aschner P, Katzeff HL, Guo H et al. Efficacy and safety of monotherapy of sitagliptin compared with metformin in patients with type 2 diabetes. Diabetes Obes Metab 2010; 12: 252–261. 78. Schweizer A, Dejager S, Bosi E. Comparison of vildagliptin and metformin monotherapy in elderly patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabetes Obes Metab 2009; 11: 804–812. 79. Ferrannini E, Fonseca V, Zinman B et al. Fifty-two-week efficacy and safety of vildagliptin vs. glimepiride in patients with type 2 diabetes mellitus 16 Deacon Aschner P, Katzeff HL, Guo H et al. Efficacy and safety of monotherapy of sitagliptin compared with metformin in patients with type 2 diabetes. Diabetes Obes Metab 2010; 12: 252–261. Aschner P, Kipnes MS, Lunceford JK, Sanchez M, Mickel C, Williams-Herman DE. Effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care 2006; 29: 2632–2637. Bergenstal RM, Wysham C, Macconell L et al. Efficacy and safety of exenatide once weekly versus sitagliptin or pioglitazone as an adjunct to metformin for treatment of type 2 diabetes (DURATION-2): a randomised trial. Lancet. 2010; 376: 431–439. Charbonnel B, Karasik A, Liu J, Wu M, Meininger G. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes inadequately controlled with metformin alone. Diabetes Care 2006; 29: 2638–2643. Goldstein BJ, Feinglos MN, Lunceford JK, Johnson J, Williams-Herman DE. Effect of initial combination therapy with sitagliptin, a dipeptidyl peptidase-4 inhibitor, and metformin on glycemic control in patients with type 2 diabetes. Diabetes Care 2007; 30: 1979–1987. Hanefeld M, Herman GA, Wu M, Mickel C, Sanchez M, Stein PP. Once-daily sitagliptin, a dipeptidyl peptidase-4 inhibitor, for the treatment of patients with type 2 diabetes. Curr Med Res Opin 2007; 23: 1329–1339. Hermansen K, Kipnes M, Luo E, Fanurik D, Khatami H, Stein P. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab 2007; 9: 733–745. Nauck MA, Meininger G, Sheng D, Terranella L, Stein PP. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trial. Diabetes Obes Metab 2007; 9: 194–205. Pratley RE, Nauck M, Bailey T et al. Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet 2010; 375: 1447–1456. Volume 13 No. 1 January 2011 review article DIABETES, OBESITY AND METABOLISM Raz I, Chen Y, Wu M et al. Efficacy and safety of sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes. Curr Med Res Opin 2008; 24: 537–550. Raz I, Hanefeld M, Xu L, Caria C, Williams-Herman D, Khatami H. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy in patients with type 2 diabetes mellitus. Diabetologia 2006; 49: 2564–2571. Reasner CA, Olansky L, Seck TL et al. Initial therapy with the fixed-dose combination (FDC) of sitagliptin and metformin (JANUMET™) in patients with type 2 diabetes mellitus (T2DM) provides superior glycemic control and A1C goal attainment with lower rates of abdominal pain and diarrhea vs. metformin alone (Abstract 610-P). Diabetes 2009; 58(Suppl. 1): A164. Rosenstock J, Brazg R, Andryuk PJ, Lu K, Stein P. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin added to ongoing pioglitazone therapy in patients with type 2 diabetes: a 24-week, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Clin Ther 2006; 28: 1556–1568. Scott R, Loeys T, Davies MJ, Engel SS. Efficacy and safety of sitagliptin when added to ongoing metformin therapy in patients with type 2 diabetes. Diabetes Obes Metab 2008; 10: 959–969. Vilsbøll T, Rosenstock J, Yki-Järvinen H et al. Efficacy and safety of sitagliptin when added to insulin therapy in patients with type 2 diabetes. Diabetes Obes Metab 2010; 12: 167–177. Yoon KH, Shockey GR, Teng R et al. Initial combination therapy with sitagliptin and pioglitazone improves glycemic control and measures of β-cell function compared with pioglitazone alone in patients with type 2 diabetes (Abstract 522-P). Diabetes 2009; 58(Suppl. 1): A139. Scheen AJ, Charpentier G, Ostgren CJ, Hellqvist A, Gause-Nilsson I. Efficacy and safety of saxagliptin in combination with metformin compared with sitagliptin in combination with metformin in adult patients with type 2 diabetes mellitus. Diabetes Metab Res Rev 2010; 26: 540–549. Vildagliptin Ahrén B, Pacini G, Foley JE, Schweizer A. Improved meal-related betacell function and insulin sensitivity by the dipeptidyl peptidase-IV inhibitor vildagliptin in metformin-treated patients with type 2 diabetes over 1 year. Diabetes Care 2005; 28: 1936–1940. Blonde L, Dagogo-Jack S, Banerji MA et al. Comparison of vildagliptin and thiazolidinedione as add-on therapy in patients inadequately controlled with metformin: results of the GALIANT trial—a primary care, type 2 diabetes study. Diabetes Obes Metab 2009; 11: 978–986. Bolli G, Dotta F, Rochotte E, Cohen SE. Efficacy and tolerability of vildagliptin vs. pioglitazone when added to metformin: a 24-week, randomized, double-blind study. Diabetes Obes Metab 2008; 10: 82–90. Bosi E, Camisasca RP, Collober C, Rochotte E, Garber AJ. Effects of vildagliptin on glucose control over 24 weeks in patients with type 2 diabetes inadequately controlled with metformin. Diabetes Care 2007; 30: 890–895. Bosi E, Dotta F, Jia Y, Goodman M. Vildagliptin plus metformin combination therapy provides superior glycaemic control to individual monotherapy in treatment-naive patients with type 2 diabetes mellitus. Diabetes Obes Metab 2009; 11: 506–515. Dejager S, Razac S, Foley JE, Schweizer A. Vildagliptin in drug-naı̈ve patients with type 2 diabetes: a 24-week, double-blind, randomized, placebo-controlled, multiple-dose study. Horm Metab Res 2007; 39: 218–223. Fonseca V, Schweizer A, Albrecht D, Baron MA, Chang I, Dejager S. Addition of vildagliptin to insulin improves glycaemic control in type 2 diabetes. Diabetologia 2007; 50: 1148–1155. Garber AJ, Foley JE, Banerji MA et al. Effects of vildagliptin on glucose control in patients with type 2 diabetes inadequately controlled with a sulphonylurea. Diabetes Obes Metab 2008; 10: 1047–1056. Garber AJ, Schweizer A, Baron MA, Rochotte E, Dejager S. Vildagliptin in combination with pioglitazone improves glycaemic control in patients with Volume 13 No. 1 January 2011 type 2 diabetes failing thiazolidinedione monotherapy: a randomized, placebocontrolled study. Diabetes Obes Metab 2007; 9: 166–174. Pan C, Yang W, Barona JP et al. Comparison of vildagliptin and acarbose monotherapy in patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabet Med 2008; 25: 435–441. Pi-Sunyer FX, Schweizer A, Mills D, Dejager S. Efficacy and tolerability of vildagliptin monotherapy in drug-naı̈ve patients with type 2 diabetes. Diabetes Res Clin Pract 2007; 76: 132–138. Ristic S, Byiers S, Foley J, Holmes D. Improved glycaemic control with dipeptidyl peptidase-4 inhibition in patients with type 2 diabetes: vildagliptin (LAF237) dose response. Diabetes Obes Metab 2005; 7: 692–698. Rosenstock J, Baron MA, Dejager S, Mills D, Schweizer A. Comparison of vildagliptin and rosiglitazone monotherapy in patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabetes Care 2007; 30: 217–223. Rosenstock J, Kim SW, Baron MA et al. Efficacy and tolerability of initial combination therapy with vildagliptin and pioglitazone compared with component monotherapy in patients with type 2 diabetes. Diabetes Obes Metab 2007; 9: 175–185. Scherbaum WA, Schweizer A, Mari A et al. Efficacy and tolerability of vildagliptin in drug-naı̈ve patients with type 2 diabetes and mild hyperglycaemia. Diabetes Obes Metab 2008; 10: 675–682. Schweizer A, Couturier A, Foley JE, Dejager S. Comparison between vildagliptin and metformin to sustain reductions in HbA(1c) over 1 year in drug-naı̈ve patients with type 2 diabetes. Diabet Med 2007; 24: 955–961. Schweizer A, Dejager S, Bosi E. Comparison of vildagliptin and metformin monotherapy in elderly patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabetes Obes Metab 2009; 11: 804–812. Saxagliptin Chacra AR, Tan GH, Apanovitch A, Ravichandran S, List J, Chen R. Saxagliptin added to a submaximal dose of sulphonylurea improves glycaemic control compared with uptitration of sulphonylurea in patients with type 2 diabetes: a randomised controlled trial. Int J Clin Pract 2009; 63: 1395–1406. DeFronzo RA, Hissa MN, Garber AJ et al. The efficacy and safety of saxagliptin when added to metformin therapy in patients with inadequately controlled type 2 diabetes with metformin alone. Diabetes Care 2009; 32: 1649–1655. Hollander P, Li J, Allen E, Chen R. Saxagliptin added to a thiazolidinedione improves glycemic control in patients with type 2 diabetes and inadequate control on thiazolidinedione alone. J Clin Endocrinol Metab 2009; 94: 4810–4819. Jadzinsky M, Pfützner A, Paz-Pacheco E, Xu Z, Allen E, Chen R. Saxagliptin given in combination with metformin as initial therapy improves glycaemic control in patients with type 2 diabetes compared with either monotherapy: a randomized controlled trial. Diabetes Obes Metab 2009; 11: 611–622. Rosenstock J, Aguilar-Salinas C, Klein E, Nepal S, List J, Chen R. Effect of saxagliptin monotherapy in treatment-naı̈ve patients with type 2 diabetes. Curr Med Res Opin 2009; 25: 2401–2411. Rosenstock J, Sankoh S, List JF. Glucose-lowering activity of the dipeptidyl peptidase-4 inhibitor saxagliptin in drug-naive patients with type 2 diabetes. Diabetes Obes Metab 2008; 10: 376–386. Scheen AJ, Charpentier G, Ostgren CJ, Hellqvist A, Gause-Nilsson I. Efficacy and safety of saxagliptin in combination with metformin compared with sitagliptin in combination with metformin in adult patients with type 2 diabetes mellitus. Diabetes Metab Res Rev 2010; 26: 540–549. Alogliptin Bosi E, Ellis G, Moneuse P, Wilson C, Fleck P. Addition of alogliptin vs uptitration of pioglitazone dose in type 2 diabetes mellitus (T2DM) patients on metformin plus pioglitazone therapy (Abstract 545). Diabetes 2010; 59(Suppl. 1): A148. doi:10.1111/j.1463-1326.2010.01306.x 17 review article DeFronzo RA, Burant CF, Fleck P, Wilson C, Mekki Q, Pratley RE. Effect of alogliptin combined with pioglitazone on glycemic control in metformintreated patients with type 2 diabetes (Abstract 752-P). Diabetologia 2009; 52(Suppl. 1): S295. DeFronzo RA, Fleck PR, Wilson CA, Mekki Q. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin in patients with type 2 diabetes and inadequate glycemic control: a randomized, double-blind, placebo-controlled study. Diabetes Care 2009; 31: 2315–2317. Nauck MA, Ellis GC, Fleck PR, Wilson CA, Mekki Q. Efficacy and safety of adding the dipeptidyl peptidase-4 inhibitor alogliptin to metformin therapy in patients with type 2 diabetes inadequately controlled with metformin monotherapy: a multicentre, randomised, double-blind, placebo-controlled study. Int J Clin Pract 2009; 63: 46–55. DIABETES, OBESITY AND METABOLISM Rosenstock J, Rendell MS, Gross JL, Fleck PR, Wilson CA, Mekki Q. Alogliptin added to insulin therapy in patients with type 2 diabetes reduces HbA(1C) without causing weight gain or increased hypoglycaemia. Diabetes Obes Metab 2009; 11: 1145–1152. Linagliptin Del Prato S, Barnett A, Huisman H, Neubacher D, Woerle HJ, Dugi KA. Linagliptin monotherapy improves glycemic control and measures of β-cell function in type 2 diabetes (Abstract 695). Diabetes 2010; 59(Suppl. 1): A189. Gomis R, Espadero RM, Jones R, Woerle HJ, Dugi KA. Efficacy and safety of initial combination therapy with linagliptin and pioglitazone in patients with inadequately controlled type 2 diabetes (Abstract 551). Diabetes 2010; 59(Suppl. 1): A150. Pratley RE, Kipnes MS, Fleck PR, Wilson C, Mekki Q. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin in patients with type 2 diabetes inadequately controlled by glyburide monotherapy. Diabetes Obes Metab 2009; 11: 167–176. Owens DR, Swallow R, Jones P, Woerle HJ, Dugi KA. Linagliptin improves glycemic control in type 2 diabetes patients inadequately controlled by metformin and sulfonylurea without weight gain and low risk of hypoglycemia (Abstract 548). Diabetes 2010; 59(Suppl. 1): A149. Pratley RE, Reusch JE, Fleck PR, Wilson CA, Mekki Q. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor alogliptin added to pioglitazone in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled study. Curr Med Res Opin 2009; 25: 2361–2371. Taskinen MR, Rosenstock J, Tamminen I et al. Efficacy and safety of linagliptin in type 2 diabetes inadequately controlled on metformin monotherapy (Abstract 579). Diabetes 2010; 59(Suppl. 1): A158. Rosenstock J, Inzucchi SE, Seufert J, Fleck PR, Wilson CA, Mekki Q. Initial combination therapy with alogliptin and pioglitazone in drug-naı̈ve patients with type 2 diabetes. Diabetes Care 2010; [epub ahead of print]. 18 Deacon Uhlig-Laske B, Ring A, Graefe-Mody U et al. Linagliptin, a potent and selective DPP-4 inhibitor, is safe and efficacious in patients with inadequately controlled type 2 diabetes despite metformin therapy (Abstract 535-P). Diabetes 2009; 58(Suppl. 1): A143. Volume 13 No. 1 January 2011