* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biopharmaceutics 2nd
Polysubstance dependence wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Tablet (pharmacy) wikipedia , lookup
Orphan drug wikipedia , lookup
Compounding wikipedia , lookup
Psychopharmacology wikipedia , lookup
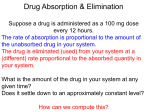
Plateau principle wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug design wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
1 WHAT IS BIOPHARMACEUTICS? Biopharmaceutics can be defined as the study of how • the physicochemical properties of drugs, • dosage forms and • routes of administration affect the rate and extent of drug absorption. Bioavailability is therefore defined as: the rate and extent of drug absorption 2 If a drug is given intravenously it is administered directly into the blood, and therefore we can be sure that all the drug reaches the systemic circulation. The drug is therefore said to be 100% bioavailable All other routes of administration where a systemic action is required, involve the absorption of the drug into the blood. 3 Plasma Concentration Absorption phase Elimination phase MSC Cmax MEC Therapeutic range (window) AUC tmax Time A typical blood plasma concentration-time curve obtained following the peroral administration of a single dose of a drug in a tablet 4 Cmax: the highest plasma drug concentration observed. Tmax: the time at which Cmax occurs following administration of an extravascular dose. AUC: Area under the curve MSC: Maximum safe concentration MEC: Minimum effective concentration Therapeutic range: The range of plasma concentrations between the minimally effective concentration and the maximum safe concentration Absorption phase: Absorption rate > Elimination rate Elimination phase: Elimination rate > Absorption rate 5 Routes of drug administration The route of administration determines the site of application of the drug product. Often the goal is to attain a therapeutic drug concentration in plasma from which drug enters the tissue (therapeutic window between toxic concentration and minimal effective concentration). 6 Routes of administration are classified into: ENTERAL and PARENTERAL Enteral means through the GI tract and includes oral, buccal, and rectal. Parenteral means not through the alimentary canal and commonly refers to injections such as IV, IM, and SC; but could also include topical and inhalation 7 A. Enteral Routes 1. Sublingual (buccal) Certain drugs are best given beneath the tongue (sublingual) or retained in the cheek pouch (buccal) and are absorbed from these regions into the local circulation. 8 These vascular areas are ideal for lipid-soluble drugs that would be metabolized in the gut or liver, since the blood vessels in the mouth bypass the liver (do not undergo first pass liver metabolism), and drain directly into the systemic circulation. This route is usually reserved for nitrates and certain hormones. 9 Diagram of first pass effect metabolised drug biliary tract liver to circulation portal vein unmetabolised drug gut 10 2. Oral By far the most common route. The passage of drug from the gut into the blood is influenced by biologic and physicochemical factors and by the dosage form. For most drugs, 2- to 5-fold differences in the rate or extent of gastrointestinal absorption can occur, depending on the dosage form. Generally, the bioavailability of oral drugs follows the order: solution > suspension > capsule > tablet > coated tablet. 11 3. Rectal The administration of suppositories is usually reserved for situations in which oral administration is difficult. This route is more frequently used in small children. It by-passes the liver 12 B. Parenteral Routes 1. Intravenous injection Used when a rapid clinical response is necessary, e.g., an acute asthmatic episode. This route allows one to achieve relatively precise drug concentrations in the plasma, since bioavailability is 100%. 13 Most drugs should be injected over 1-2 minutes in order to prevent the occurrence of very high drug concentrations in the injected vein, possibly causing adverse effects. Some drugs, particularly those with narrow therapeutic indices or short half-lives, are best administered as a slow IV infusion or drip. 14 2. Intramuscular injection Drugs may be injected into the arm (deltoid), thigh (vastus lateralis) or buttocks (gluteus maximus). Because of differences in vascularity, the rates of absorption differ, with arm > thigh > buttocks. Drug absorption may be slow and erratic. Lipid solubility and degree of ionization influence absorption. It should not be assumed that the IM route is as reliable as the IV route. 15 3. Subcutaneous injection Some drugs, notably insulin, are routinely administered SC. Drug absorption is generally slower SC than IM, WHY? due to poorer vascularity. Absorption can be facilitated by heat, massage or vasodilators. It can be slowed by coadministration of vasoconstrictors, a practice commonly used to prolong the local action of local anesthetics. As above, arm > thigh. 16 17 4. Topical application a. Eye For desired local effects. b. Intravaginal For infections or contraceptives. c. Intranasal For alleviation of local symptoms. Directly from nasal capillaries into circulation. 18 d. Skin Systemic absorption does occur and varies with the area, site, drug, and state of the skin. Dimethyl sulfoxide (DMSO) enhances the percutaneous absorption of many drugs. e. Drug patches (drug enters systemic circulation by zero order kinetics – a constant amount of drug enters the circulation per unit time). 19 5. Inhalation Volatile anesthetics, as well as many drugs which affect pulmonary function, are administered as aerosols. The large alveolar area and blood supply lead to rapid absorption into the blood. Drugs administered via this route are not subject to first-pass liver metabolism. 20 6. Other ROA's Other routes of administration include: • intra-arterial for cancer chemotherapy to maximize drug concentrations at the tumor site • intrathecal directly into the cerebrospinal fluid. 21 Why are there different routes? 1.Solubility or stability of the drug 2.The absorption from the different sites. Many drugs are absorbed from stomach and small intestine and not absorbed rectally. 3.Toxic when given by certain routes. 4.Ineffective, destroyed or inactivated in certain organs e.g. penicillin in stomach. 5.Convenience of the patient 22 Route for Administration Time until Effect IV 30-60 sec Inhalation 2-3 min Sublingual 3-5 min IM 10-20 min SC 15-30 min Rectal 5-30 min Ingestion 30-90 min Transdermal (Topical) Variable (minutes-hours) 23 The concentration of the drug in blood plasma depends on LADME L = Liberation the release of the drug from it's dosage form. A = Absorption the movement of drug from the site of administration to the blood circulation. D = Distribution the process by which drug diffuses or is transferred from intravascular space to extravascular space (body tissues). 24 The concentration of the drug in blood plasma depends on LADME M = Metabolism the chemical conversion or transformation of drugs into compounds which are easier to eliminate. E = Excretion the elimination of unchanged drug or metabolite from the body via renal, biliary, or pulmonary processes. 25 26 27 28 Absorption The absorption of a drug from the GIT is the passage of the substance from the lumen through several membranes into the blood stream. Main factors affecting oral absorption: • Physiological factors • Physical-chemical factors • Formulation factors GIT BLOOD 29 1. Physiological Factors Affecting Oral Absorption A- Membrane physiology B- Passage of drugs across membranes Active transport Facilitated diffusion Passive diffusion Pinocytosis Pore transport Ion pair formation 30 C- Gastrointestinal physiology GIT physiology and drug absorption Gastric emptying time and motility Effect of food on drug absorption Enterohepatic circulation First pass effect 31 A. Membrane physiology Membrane structure (Fluid Mosaic Model) The biologic membrane consists mainly of a lipid bilayer containing primarily phospholipids and cholesterol, with imbedded proteins. The membrane contains also small aqueous channels or pores. 32 Phospholipid Bilayers Phospholipids are amphiphilic in nature. Polar heads are oriented toward the water and the fatty acid tails are oriented toward the inside of the bilayer. The fatty acid tails are flexible, causing the lipid bilayer to be flexible. At body temperature, membranes are a liquid with a consistency that is similar to cooking oil. 33 Cholesterol Cholesterol is a major membrane lipid. It may be equal in amount to phospholipids. It is similar to phospholipids in that one end is hydrophilic the other end is hydrophobic. Cholesterol makes the membrane less permeable to most biological molecules. Proteins Proteins are scattered throughout the membrane. They may be attached to inner surface, embedded in the bilayer, or attached to the outer surface. 34 35 Functions of Membrane Proteins Channel 36 A. Channel proteins A protein that allows a particular molecule or ion to freely cross the membrane as it enters or leaves the cell. B. Carrier proteins A protein that selectively interacts with a specific molecule or ion so that it can cross the cell membrane to enter or exit the cell. 37 C. Receptor proteins A protein that has a specific shape so that specific molecules can bind to them. The binding of a molecule, such as a hormone, can influence the metabolism of the cell. D. Enzyme proteins An enzyme that catalyzes a specific reaction. 38 E. Cell-recognition proteins Glycoproteins that identify the cell. They make up the cellular fingerprint by which cells can recognize each other. F. Cell Adhesion Proteins Adjacent cells stick together via interlocking proteins on their membranes 39 B. Passage of Drugs Across Membranes The membrane can be viewed as a semipermeable lipoidal sieve that allows the passage of: - lipid-soluble molecules across it by passive lipid diffusion - water and small hydrophilic molecules through its numerous aqueous pores. -other molecules by a number of transporter proteins or carrier molecules that exist in the membrane. 40 There are two main mechanisms of drug transport across the gastrointestinal epithelium: Paracellular: i.e. between the cells. Transcellular: i.e. across the cells The transcellular pathway is further divided into simple passive diffusion, carrier-mediated transport (active transport and facilitated diffusion) and endocytosis. 41 1. Passive Transport Most (many) drugs cross biological membranes by passive diffusion. • Diffusion occurs when the drug concentration on one side of the membrane is higher than that on the other side (according to concentration gradient). • Drug diffuses across the membrane in an attempt to equalize the drug concentration on both sides of the membrane. 42 • The rate of transport of drug across the membrane can be described by Fick's first law of diffusion:- D: diffusion coefficient This parameter is related to: • the size of the drug • lipid solubility of the drug • viscosity of the diffusion medium, the membrane. As lipid solubility increases or molecular size decreases then D increases and thus diffusion rate also increases. 43 A: surface area As the surface area increases the rate of diffusion also increase. The surface of the intestinal lining (with villae and microvillae) is much larger than the stomach. Therefore absorption is generally faster from intestine compared to stomach. x: membrane thickness The smaller the membrane thickness the quicker the diffusion process. e.g. the membrane in the lung is quite thin thus inhalation absorption can be quite rapid. 44 (Ch -Cl): concentration difference. Since V, the apparent volume of distribution, is at least four liters and often much higher the drug concentration in blood or plasma will be quite low compared with the concentration in the GI tract. It is this concentration gradient which allows the rapid complete absorption of many drug substances. Normally Cl << Ch then:Thus the absorption of many drugs from the G-I tract can often appear to be first-order. 45 2. Facilitated Transport • Is also the movement of molecules from a high concentration to a low concentration. • Lipid insoluble substances such as glucose and amino acids are taken across by "carrier proteins". • No chemical energy is required in this process, WHY? • eg. amino acids, glucose and other breakdown products of food are absorbed by the small intestine facilitated diffusion 46 Active Transport 3. Active Transport It is the movement of molecules across a living membrane from an area of low concentration to an area of high concentration with the aid of a carrier protein and using energy or ATP . The rate of drug absorption increases with drug concentration until the carrier molecules are completely saturated, the rate then remains constant 47 48 Mechanism of Drug Transport ? 49 4. Endocytosis Surrounding a substance with the cell membrane and the subsequent formation of a vesicle to bring these substances into the cell. This process is energy dependent. 50 There are two main kinds of Endocytosis: a. Phagocytosis (cell eating) - involves the ingestion of particles larger than 500 nm. This process is important in the absorption of polio and other vaccines from the GIT. b. Pinocytosis (cell drinking) - involves the ingestion of fluids or dissolved particles. Fat soluble vitamins A, D, E and K are absorbed via pinocytosis 51 5. Pore Transport • Very small molecules (hydrophilic, water soluble such as water, urea and sugar) are able to rapidly cross cell membrane as if the membrane contained pores or channels. • This model of transportation is used to explain renal excretion of drugs and uptake of drugs into the liver. • A certain type of protein may form an open channel across the lipid membrane of cell. 52 Ion pair formation Strong electrolyte drugs are highly ionized and maintain their charge at physiological pH. • These drugs penetrate membranes poorly, WHY? • When linked up with an oppositely charged ion, an ion pair is formed in which the overall charge of the pair is neutral. • The neutral complex diffuses more easily across the membrane, WHY? • An example of this in case of propranolol, a basic drugs that forms an ion pair with oleic acid. 53 Paracellular Transport Two pathways exist for the passage of water and electrolytes across the intestinal mucosa, transcellular and paracellular. The transcellular pathway allows the passage of hyrophilic molecules of low molecular weight and with small molecular size through the water filled pores in the cell membranes. 54 The paracellular pathway allows access of larger molecules through the junction between the cells. Although the intercellular spaces occupy less than 1% of the surface area of the epithelium it is by this way the hydrophilic drug molecules are absorbed e.g. ranitidine , acyclovir. 55 C. Gastrointestinal (GI) Physiology I- Characteristics of GI physiology and Drug Absorption The gastrointestinal tract is a muscular tube approximately 6 m in length with varying diameters. It stretches from the mouth to the anus and consists of four main anatomical areas: - oesophagus - stomach - small intestine - large intestine or colon. The luminal surface of the tube is not smooth but very rough, thereby increasing the surface area for absorption.56 57 Organs pH Membrane Blood Supply Surface Area Transit Time Bypass liver Buccal approx 6 thin Good, fast absorption with low dose small Short unless controlled yes Esophagus 6-7 Very thick no absorption - small short, a few seconds, - Stomach 1.7-4.5 normal good small 30 min delayed stomach emptying intestinal absorption no Duodenu m 5-7 normal good very large very short (6" long), no Small Intestine 6 -7 normal good very large about 3 hours no Large Intestine 6.8 - 7 - good not very large long, up to 24 hr lower colon, rectum 58 yes II. Gastric emptying and motility Generally drugs are better absorbed in the small intestine, WHY? (because of the larger surface area) than in the stomach, therefore quicker stomach emptying will increase drug absorption. e.g. a good correlation has been found between stomach emptying time and peak plasma concentration for acetaminophen. The quicker the stomach emptying the higher the plasma concentration. 59 Also slower stomach emptying can cause increased degradation of drugs in the stomach's lower pH; e.g. L-dopa. 60 Factors Affecting Gastric Emptying Volume of Ingested Material Type of Meal Bulky material tends to empty more slowly than liquids Fatty food Decrease Carbohydrate Decrease Temperature Increase in temperature, increase in emptying of Food rate Body Position Lying on the left side decreases emptying rate. Standing versus lying (delayed) Drugs Anticholinergics (e.g. atropine), Decrease Narcotic (e.g. morphine, alfentanil), Analgesic (e.g. aspirin) Metoclopramide, Domperidone, Erythromycin, Bethanchol Increase 61 III. Effect of Food The presence of food in the gastrointestinal tract can influence the rate and extent of absorption Complexation of drugs with components in the diet e.g. Tetracycline forms non-absorbable complexes with calcium and iron (don’t take milk or iron preparations at the same time of day as the tetracycline WHY?). 62 Alteration of pH In general, food tends to increase stomach pH by acting as a buffer. This is liable to decrease the rate of dissolution and subsequent absorption of a weakly basic drug and increase that of a weakly acidic one. Alteration of gastric emptying Particularly fatty foods, and some drugs, tend to reduce gastric emptying and thus delay the onset of action of certain drugs. 63 Stimulation of gastrointestinal secretions e.g. pepsin produced in response to food may result in the degradation of drugs that are susceptible to enzymatic metabolism, and hence in a reduction in their bioavailability. Food, particularly fats, stimulates the secretion of bile. Bile salts are surface active agents and can increase the dissolution of poorly soluble drugs, thereby enhancing their absorption. e.g. Griseofulvin (antifungal) 64 Competition between food components and drugs for specialized absorption mechanisms In the case of those drugs that have a chemical structure similar to nutrients required by the body for which specialized absorption mechanisms exist, there is a possibility of competitive inhibition of drug absorption. 65 Increased viscosity of gastrointestinal contents The presence of food in the gastrointestinal tract provides a viscous environment which may result in a reduction in the rate of drug dissolution and the rate of diffusion of a drug in solution from the lumen to the absorbing membrane. 66 Food-induced changes in presystemic metabolism Certain foods may increase the bioavailability of drugs that are susceptible to presystemic intestinal metabolism by interacting with the metabolic process. e.g. Grapefruit juice is capable of inhibiting the intestinal cytochrome P450 and thus, taken with drugs that are susceptible to cytochrome P450 metabolism, is likely to result in their increased bioavailability. 67 IV. Enterohepatic circulation (Biliary recycling) •Some drugs when absorbed from intestine they are carried via the portal vein into the liver. •In the liver they are metabolized and secreted into the bile 68 • As a conjugated drug they are transported again via bile duct into intestine (In the conjugated form they are not absorbed again from intestine). • After meals the secretion of bile is stimulated. The bile release the drug from its conjugate, thus it will be reabsorbed again as if a new dose was given. • Biliary recycling of a drug results in prolonging drug action. 69 Diagram of biliary recycling conjugated drug biliary tract liver portal vein to circulation unconjugated drug gut 70 IV. First pass effect Is a phenomenon of drug metabolism whereby the concentration of a drug is greatly reduced before it reaches the systemic circulation. After a drug is swallowed, it is absorbed by the digestive system and enters the hepatic portal system. It is carried through the portal vein into the liver before it reaches the rest of the body. 71 The liver metabolizes many drugs, sometimes to such an extent that only a small amount of active drug emerges from the liver to the rest of the circulatory system . This first pass through the liver thus greatly reduces the bioavailability of the drug. 72 Diagram of first pass effect 73 2. Physicochemical Factors Affecting Oral Absorption • pH-partition theory • Lipid solubility of drugs • Dissolution and pH • Salts • Crystal form • Drug stability and hydrolysis in GIT • Complexation • Adsorption 74 A. pH - Partition Theory The pH - partition theory explains the influence of GI pH and drug pKa on the extent of drug absorption. As most drugs are weak electrolytes, the unionized form of weakly acidic or basic drugs (i.e. the lipid- soluble form) will pass across the gastrointestinal epithelia, whereas the gastrointestinal epithelia is impermeable to the ionized (i.e. poorly lipid-soluble) form of such drugs. 75 According to the pH-partition hypothesis, the absorption of a weak electrolyte will be determined chiefly by the extent to which the drug exists in its unionized form at the site of absorption. 76 The extent to which a weakly acidic or basic drug ionizes in solution in the gastrointestinal fluid is determined by: its pKa & the pH at the absorption site and may be calculated using the appropriate form of the Henderson- Hasselbach equation 77 What is acid? acid is a substance that liberates hydrogen ions [H+] in solution. What is a base? A base is a substance that can bind H+ and remove them from solution. pH = - log [H+] Strong acids, strong bases, as well as strong electrolytes are essentially completely ionized in aqueous solution. Weak acids and weak bases are only partially ionized in aqueous solution and yield a mixture of the 78 undissociated compound and ions. In solutions equilibria undissociated of exist weak acids between molecules HA H+ + A- and their ions. The ionization constant Ka of a weak acid can be obtained by applying the Law of Mass Action: Ka = [H+] [A-] [HA] 79 pKa = the negative logarithm of Ka pKa = pH - log For acidic drugs, the lower [A-] [HA] the pKa the stronger the acid From the pKa, one can calculate the proportions of drug in the charged and uncharged forms at any pH: log [A-] [HA] = pH - pKa Henderson - Hasselbalch Equation 80 Some Typical pKa Values for Weak Acids at 25 °C Weak Acid pKa Acetic 4.76 Acetylsalicyclic 3.49 Boric 9.24 Penicillin V 2.73 Phenytoin 8.1 Salicyclic 2.97 Sulfathiazole 7.12 81 In solutions of weak bases equilibria exist between undissociated B + H+ BH+ molecules and their ions. The ionization constant Ka of a protonated weak base can be obtained by applying the Law of Ka = [H+] [B] [BH+] Mass Action: 82 pKa = the negative logarithm of Ka For basic drugs, the higher the pKa = pH - log [B] [BH+] pKa the stronger the base From the pKa, one can calculate the proportions of drug in the charged and uncharged forms at any pH: log [B] [BH+] = pH - pKa Henderson - Hasselbalch Equation 83 Therefore, according to these equations: a weakly acidic drug, pKa 3.0, will be: predominantly unionized in gastric fluid at pH 1.2 (98.4%) and almost totally ionized in intestinal fluid at pH 6.8 (99.98%), a weakly basic drug, pKa 5, will be: almost entirely ionized (99.98%) at gastric pH of 1.2 and predominantly unionized at intestinal pH of 6.8 (98.4%). 84 This means that, according to the pH-partition hypothesis, a weakly acidic drug is more likely to be absorbed from the stomach where it is unionized, and a weakly basic drug from the intestine where it is predominantly unionized. However, in practice, other factors need to be taken into consideration. 85 Lipid solubility :weak acids and weak bases HA <==> H+ + A[ UI ] [I] pKa=pH + log (HA/A-) ASPIRIN pKa = 4.5 (weak acid) 100mg orally 0.1 = [ I ] Stomach pH = 2 99.9 = [ UI ] Blood pH = 7.4 [ UI ] Aspirin is reasonably absorbed from stomach (fast action) B + HCl <==> BH+ + Cl[ UI ] [I] pKa= pH + log(BH+/B) STRYCHNINE pKa = 9.5 (weak base) 100mg orally 99.9 = [ I ] Stomach pH = 2 0.1 = [ UI ] Blood pH = 7.4 [ UI ] Strychnine not absorbed until 86 enters duodenum Limitations of the pH-partition hypothesis Weak acids are also absorbed from the small intestine due to: The significantly larger surface area that is available for absorption in the small intestine in contrast to stomach The longer small intestinal residence time The microclimate pH, that exists at the surface of the intestinal mucosa and is lower than that of the luminal pH of the small intestine 87 The pH -partition hypothesis cannot explain the fact that certain drugs (e.g. tetracyclines) are readily absorbed despite being ionized over the entire pH range of the gastrointestinal tract. One suggestion for this is that such drugs interact with endogenous organic ions of opposite charge to form an absorbable neutral species - an ion pair - which is capable of partitioning into the lipoidal GIT barrier and be absorbed via passive diffusion. 88 B. Lipid Solubility of Drugs Barbitone and thiopentone, have similar dissociation constants - pKa 7.8 and 7.6, respectively - and therefore similar degrees of ionization at intestinal pH. However, thiopentone is absorbed much better than barbitone. WHY? the absorption of drugs is also affected by the lipid solubility of the drug. Thiopentone, being more lipid soluble than barbitone, exhibits a greater affinity for the gastrointestinal membrane and is thus far better absorbed. 89 How can we measure lipid solubility?? An indication of the lipid solubility of a drug, and (its absorption) is given by its ability to partition between a lipid-like solvent (usually octanol) and water. This is known as the drug's partition coefficient, and is a measure of its lipophilicity. 90 The partition coefficient P is the ratio of the drug concentration in the organic phase to its concentration in the aqueous phase Partition coefficient (p) = [ L] conc / [W] conc [ L] conc is the concentration of the drug in lipid phase, [W] conc is the concentration of the drug in aqueous phase. The higher p value, the more absorption is observed. Polar molecules, i.e. those that are poorly lipid soluble and relatively large, such as heparin are poorly absorbed after oral administration and therefore have to be given by injection. 91 The drug is too hydrophilic, what can be done?? Prodrug is one of the options that can be used to enhance p value and absorption as sequence. A prodrug is a chemical modification, frequently an ester of an existing drug. The ester linkage increases lipophilicity of the compound enhances the absorption. the thus A prodrug has no pharmocological activity itself but it converts back to the parent compound as a result of metabolism by the body. (e.g. Rivampicillin a prodrug for ampicillin) 92 C. Drug Dissolution So far we have looked at the transfer of drugs in solution in the G-I tract, through a membrane, into solution in the blood. However, many drugs are given in solid dosage forms and therefore must dissolve before absorption can take place. 93 If absorption is slow relative to dissolution then all we are concerned with is absorption. However, if dissolution is the slow, rate determining step (the step controlling the overall rate) then factors affecting dissolution will control the overall process. The rate of solution may be explained using Fick’s First Low of Diffusion: It is the rate at which a dissolved solute particle diffuses through the stagnant layer to the bulk solution 94 Fick's first law By Fick's first law of diffusion: h Solid Cs D diffusion coefficient, Stagnant Layer A surface area, Cs solubility of the drug, Cb concentration of drug in the bulk solution, h thickness of the stagnant layer. Cb Bulk Solution As Cb is much smaller than Cs the equation reduces to : 95 There are a number of factors which affect drug dissolution: Surface area, A The surface area per gram (or per dose) of a solid drug can be changed by altering the particle size. e.g. a cube 3 cm on each side has a surface area of 54 cm2. If this cube is broken into cubes with sides of 1 cm, the total surface area is 162 cm2. 96 Generally as A increases the dissolution rate will also increase. Improved bioavailability has been observed with griseofulvin, digoxin, etc. Methods of particle size reduction include mortar and pestle, mechanical grinders, fluid energy mills, solid dispersions in readily soluble materials (PEG's). 97 Diffusion layer thickness, h This thickness is affected by the agitation in the bulk solution. In vivo we usually have very little control over this parameter. It is important though when we perform in vitro dissolution studies because we have to control the agitation rate so that we get similar results in vitro as we would in vivo. 98 Diffusion coefficient, D The value of D depends on the size of the molecule and the viscosity of the dissolution medium. Increasing the viscosity will decrease the diffusion coefficient and thus the dissolution rate. This could be used to produce a sustained release effect by including a larger proportion of something like sucrose or acacia in a tablet formulation. 99 Drug solubility, Cs Solubility is another determinant of dissolution rate. As Cs increases so does the dissolution rate. We can look at ways of changing the solubility of a drug: 100 D. (1) Salt Form If we look at the dissolution profile of various salts. Salts of weak acids and weak bases generally have much higher aqueous solubility than the free acid or base, therefore if the drug can be given as a salt the solubility can be increased and we improved should have dissolution. One example is Penicillin V. 101 E. (2) Crystal Form Some drugs exist in a number of crystal forms or polymorphs. These different forms may well have different solubility properties and thus different dissolution characteristics. Chloramphenicol palmitate is one example which exists in at least two polymorphs. 102 The B form is apparently more bioavailable. This is attributed to the more rapid in vivo rate of dissolution. The recommendation might be that manufacturers should use B polymorph for maximum solubility and absorption. Plot of Cp versus Time for Three Formulations of 103 Chloramphenicol Palmitate In addition to different polymorphic crystalline forms, a drug may exist in an amorphous form. Because the amorphous form usually dissolves more rapidly than the corresponding crystalline forms there will be significant differences in the bioavailabilities. e.g. antibiotic novobiocin. The more soluble and rapidly dissolving amorphous form of novobiocin was readily absorbed. However, the less soluble and slower-dissolving crystalline form of novobiocin was not absorbed to any significant extent thus therapeutically ineffective. 104 F. Drug Stability and Hydrolysis in GIT Acid and enzymatic hydrolysis of drugs in GIT is one of the reasons for poor bioavailability. Penicillin G (half life of degradation = 1 min at pH= 1) Rapid dissolution leads to poor bioavailability WHY? (due to release large portion of the drug in the stomach, pH = 1.2) How to protect the drug from the gastric juice? 1. Enteric coating the tablet containing the drug. 2. Prodrug that exhibits limited solubility in gastric fluid but liberates the parent drug in intestine to be absorbed. 105 G. Adsorption Certain insoluble substances may adsorb co-administrated drugs leading to poor absorption. Charcoal (antidote in drug intoxication). 106 H. Complexation Complexation of a drug in the GIT fluids may alter rate and extent of drug absorption. 1. GIT component- drug interaction: Intestinal mucosa + Streptomycin = poorly absorbed complex 2. Food-drug interaction: Calcium + Tetracycline = poorly absorbed complex 3. Tablet additive – drug interaction: Carboxyl methylcellulose (CMC) + Amphetamine = poorly absorbed complex 107 4. Complexing agent + polar drugs: Dialkylamides + prednisone = well-absorbed lipid soluble complex 5. Lipid soluble drug + water soluble complexing agent Miconazole + cyclodextrine = water soluble complex 108 3. Formulation Factors Affecting Oral Absorption Role of dosage forms Solutions Suspensions Capsules Tablets - uncoated - coated 109 With any drug it is possible to alter its bioavailability considerably by formulation modification. Since a drug must be in solution to be absorbed efficiently from the G-I tract, you may expect the bioavailability of a drug to decrease in the order: solution > suspension > capsule > tablet > coated tablet. This order may not always be followed but it is a useful guide. One example is the results for pentobarbital. Here the order was found to be: aq solution > aq suspension = capsule > tablet of free acid form. 110 I. Solution dosage form Drugs are commonly given in solution in cough/cold remedies and in medication for the young and elderly. In general, drugs must be in solution in gastrointestinal fluids before absorption can occur. For drugs that are water soluble and chemically stable in aqueous solution, formulation as a solution normally eliminates the in vivo dissolution step and presents the drug in the most readily available form for absorption 111 therefore absorption from an oral solution is rapid and complete, compared with administration in any other oral dosage form. The rate limiting step is often the rate of gastric emptying since absorption will generally be more rapid in the intestine. • However, dilution of an aqueous solution of a poorly water-soluble drug whose aqueous solubility had been increased by: formulation techniques such as 1cosolvency, 2complex formation or 3solubilization can result in precipitation of the drug in the gastric fluids. 112 • Similarly, exposure of an aqueous solution of a 4salt of a weak acidic compound to gastric pH can also result in precipitation of the free acid form of the drug. In most cases the extremely fine nature of the resulting precipitate permits a more rapid rate of dissolution than if the drug had been administered in other types of oral dosage forms, such as aqueous suspension, hard gelatin capsule or tablet. 113 II. Suspension dosage form A well formulated suspension is second to a solution (nonprecipitating) in terms of superior bioavailability. Absorption may well be dissolution limited, however a suspension of a finely divided powder and hence large surface area will maximize the potential for rapid dissolution. With very fine particle sizes the dispersibility of the powder becomes important. 114 The addition of a surface active agent will improve dispersion of a suspension. As a suspension ages there is potential for increased particle size with an accompanying decrease in dissolution rate. 115 III. Capsule dosage form Provided: the hard gelatin shell dissolves rapidly in the GI fluids encapsulated mass disperses rapidly and efficiently, a relatively large effective surface area of drug will be exposed to the gastrointestinal fluids, thereby facilitating dissolution. 116 The capsule contents should not be subjected to high compression forces which would tend to reduce the effective surface area, thus tightly packed capsules may have reduced dissolution and bioavailability. The inclusion of excipients (e.g. diluents, lubricants and surfactants) in a capsule formulation can have a significant effect on the rate of dissolution of drugs, particularly those that are poorly soluble and hydrophobic. 117 If a drug is hydrophobic a dispersing agent should be added to the capsule formulation. A hydrophilic diluent (e.g. sorbitol, lactose) often serves to increase the rate of penetration of the aqueous gastrointestinal fluids into the contents of the capsule, and to aid the dispersion and subsequent dissolution of the drug in these fluids. However, the diluent should exhibit no tendency to adsorb or complex with the drug, as either can impair absorption from the gastrointestinal tract. 118 119 IV. Tablet dosage form Uncoated tablets Tablets are the most widely used dosage form. When a drug is formulated as a compressed tablet there is an enormous reduction in the effective surface area of the drug, owing to the granulation and compression processes involved in tablet making. The tablets should disintegrate rapidly and completely in the GIT fluids so that a fine, well dispersed suspension of drug particles in the GIT fluids is generated following the administration of a tablet. 120 The overall rate of tablet disintegration influenced by several interdependent factors: the concentration and type of drug, diluent, binder, disintegrant, lubricant and wetting agent as well as the compaction pressure. 121 Film Coated Tablet Tablet coatings may be employed to: - mask an unpleasant taste or odour or - to protect an ingredient from decomposition during storage. 122 Enteric Coated Tablet An enteric coat is designed to: resist the low pH of gastric fluids but to disrupt or dissolve when the tablet enters the higher pH of the duodenum. Enteric coating protects which would otherwise drugs be destroyed if released into gastric fluid and also protects the stomach against drugs which can produce nausea or mucosal irritation (e.g. aspirin, ibuprofen) if released at this site. 123 The presence of a coating presents a physical barrier between the tablet core and the gastrointestinal fluids. Coated tablets therefore not only possess all the potential bioavailability problems associated with uncoated conventional tablets, but are subject to the additional potential problem of being surrounded by a physical barrier. 124