* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Brucellosis wikipedia , lookup
West Nile fever wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Meningococcal disease wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hepatitis C wikipedia , lookup
Neonatal infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Trichinosis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
History of tuberculosis wikipedia , lookup
Chagas disease wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis B wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Fasciolosis wikipedia , lookup
Tuberculosis wikipedia , lookup
Leptospirosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
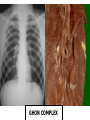
CHRONIC PNEUMONIAS Chronic Pneumonias Often SYNONYMOUS with the 4 classic fungal or granulomatous pulmonary infections . If you see pulmonary granulomas, think of a CHRONIC process, often years. Include : Tuberculosis Histoplasmosis Blastomycosis Coccidiodomycosis : (kok-sid-e-oy-doh-my-KOH-sis) 1- Histoplasmosis,Coccidiodomycosis,Blastomycosis Usually normal host, also immunocompromised Presentation & pathology very similar to T.B. Acute primary pulmonary infection Chronic cavitary pulmonary infection Disseminated miliary infection Lesion is granuloma with necrosis & giant cells Identify the organisms Infections in immunocompromised patients: 1- Candidiasis : Common superficial oral or vaginal mucosal or skin infections. Maybe invasive in special patients. AIDS , renal transplant, neutropenia , heart valvular diseases. Selective involvement of esophagus in AIDS 2-Cryptococcosis : (krip-toh-ko-koh-sis) Opportunistic infection specially in AIDS. Gelatinous organisms, initiates minimal inflammation. Pulmonary, CNS, Disseminated disease. Usually inhalation to lung, spread to meninges in gelatinous masses. 3- Aspergillosis : 1- Invasive pulmonary aspergillosis : Immunocompromised host: Multifocal necrotizing pneumonia May invade Blood Vessles dissemiation with vasculitis, occlusion,& infarction. 2-Aspergilloma : (mycetoma) growing in existing cavities , specially in TB & bronchiectasis. 3-Allergic bronchopulmonary aspergillosis: Asthmatic attack or hypersensitivity pneumonitis : Transient pulmonary infiltrates, eosinophilia IgE ASPERGILLOMA 4 - Mucormycosis: Hyphae localized in nose brain. In lung localized cavity or miliary. Immunocompromised host, specially in diabetics. 5- Pneumocystis carinii pneumonia : ? Protozoa, ? Fungus Majority of humans show positive serology , but no disease Opportunistic infection in AIDS , often with CMV (reactivation) Pathology : Interstitial lymphocytic infiltration. Pink frothy exudate in alveoli. Cysts or trophozoites in exudate. Diagnosis : Organism best detected by special stains & PCR on the following samples : Bronchoalveolar lavage Transbronchial biopsy Silver Stain (+) Methenamine SILVER stain for Pneumocystis Carinii Clinical Picture : Fever, dry cough, dyspnea, hypoxia Chest X ray : Bilateral perihilar & Basilar nodular infiltrates Restrictive pulmonary function defects Recurrences are common 6- Cytomegalovirus ( CMV ) Immunocompromised : Transplants & AIDS. Commonest pathogen in AIDS patients. Necrotizing Interstitial Pneumonia with inclusions. Retinitis Gastrointestinal ulcerations & diarrhea Thank you Tuberculosis Ancient Disease - New Threat TB is an ancient infectious disease caused by Mycobacterium tuberculosis. It has been known since 1000 B.C. 1900’s Approximately all of Europe’s adult population infected with TB No treatment Up till the ’50s Sanatorium with Emphasis on rest, good nutrition, and fresh mountainous air Isolation led to in transmission Meeting held in London (1977) It was concluded that by 1990 Tuberculosis would be rare and by 2010 it will only be of historical interest to the medical fraternity! TUBERCULOSIS Infects one third of world population..! 3 million deaths due to TB every year Under privileged population Since 1985 incidence is increasing in west AIDS, Diabetes, Immunosuppressed patients. Drug resistance Communicable disease caused usually by M. hominis ,bovis, avium,…etc. May affect any organ lung is most affected . Route of infection : Inhalation Lung OR Ingestion Intestine Not all exposed get infected Genetic makeup linked to NRAMP1 polymorphism Mostly self limited , viable organisms Since TB is a disease of respiratory transmission, optimal conditions for transmission include: overcrowding poor personal hygiene poor public hygiene Poor nutrition Transmission Pulmonary tuberculosis is a disease of respiratory transmission, Patients with the active disease (bacilli) expel them into the air by: coughing, sneezing, or any other way that will expel bacilli into the air Environmental Factors Increase Risk for Transmission Exposure in small, enclosed spaces Inadequate ventilation Re-circulated air containing infectious droplets Inadequate cleaning and disinfection of equipment Improper specimen-handling procedures Pathogenesis : TB bacilli taken up by alveolar macrophages through action of receptors on their surface Bacilli inhibit microbial killing by interfering with phagolysosomal function Proliferation of bacilli inside alveolar macrophages, then released→bacteremia Majority are symptomless Inside LN, cell mediated immunity after 3w CD4+TH1 subset→ IFN γ activate macrophages → mediators → bacterial killing Immune response leads to caseation Caseation is tissue necrosis, later healing Outcome of the disease depends on the balance of immunity to tissue destruction Signs and symptoms Early symptoms Common cold symptoms Listlessness, fatigue, fever, a minimally productive cough of yellow or green sputum and a general feeling of malaise. Later symptoms Night sweats, fever, cough with purulent secretions and haemoptysis, dyspnoea, chest pain, and hoarseness appear. Types of TB infection : 1. Primary TB :Infection in unsensitized or immunocompromised host 2. Secondary ( reactivation TB) 3. Progressive pulmonary TB 4. Miliary TB 5. Isolated organ TB 1- Primary TB : Subpleural caseating granuloma Ghon focus Caseation , surrounded by chronic inflammatory cells, epitheloid cells & Langhan’s giant cells Enlarged hilar LNs with caseation Ghon Complex Ghon focus + nodal involvement GHON COMPLEX Caseating granulomata Caseating granulomata WHAT HAPPENS LATER ??? Outcome of Primary TB : - In 95% cell mediated immunity healing in 3 weeks - Fibrosis calcification Ranke complex - Uncommonly disseminated disease Progressive Primary TB 2. Secondary (Reinfection TB) Arises in a previously sensitized host in one of following : Progressive post primary ( < 5% ) Reactivation of old focus Reinfection with a virulent strain Infection is characterized by : Location usually at apex about 2 cm.size CAVITATION is common Lymph node enlargement less prominent Sputum is positive for TB bacilli in most cases Symptoms : Hemoptysis common, fever , loss of weight night sweats, pleuritic pain…. Extrapulmonary manifestations if present May be asymptomatic ! Outcome : May heal or become progressive 3. Progressive Pulmonary TB This can occur after primary or secondary TB , along the following routes : Tracheobronchial tree & lymphatics Tuberculous bronchopneumonia OR Miliary pulmonary disease. Pleural involvement leads to effusion, empyema or obliterative fibrous pleuritis Spread through trachea to larynx leads to Laryngeal TB Swallowing infected sputum leads to intestinal TB Spread through pulmonary veins Heart systemic circulation generalized spread 4. Systemic Miliary TB Numerous tiny tubercles in any organ Most affected : Liver Bone marrow Spleen Adrenals Meninges Kidneys….etc Systemic Miliary TB 5. Isolated Organ TB Spread through blood low grade bacteremia leads to granulomatous infection in any organ Symptoms depend on the organ: Tuberculous salpingitis & endometritis lead to sterility Vertebral TB POTT’s Disease Adrenal gland Addisons disease Tuberculous lymphadenitis± Scrofuloderma Renal infection Tuberculous chronic Pyelonephritis, nephrotic syndrome… Male Genital system Tuberculous epididymo-orchitis & prostatitis sterility Chronic TB SECONDARY AMYLOIDOSIS Adrenal TB - Addison Disease Spinal TB - Potts Disease Tuberculosis in HIV : Bacterial pneumonias in general are commoner & more serious than in immunocompetent patients Tuberculosis in initial phases of HIV is usually secondary reactivation TB In late stages : Miliary TB & Atypical TB M.avium common in late stages poorly formed granuloma without caseation Diagnosis of TB Clinical picture X ray picture Sputum : Direct examination for Acid Fast Bacilli (ZN, Auramine-rhodamine stains, PCR) Culture of sputum about 6 weeks Chest X-ray in primary TB Later : Chest x-rays: Multi nodular infiltrate above or behind the clavicle with or without pleural effusion unilaterally or bilaterally. Diagnosis (continued) Sputum investigation: Cultures will reveal the presence of mycobacterium tuberculosis Patients stay infectious for as long as the bacilli are excreted in the sputum AFB - Ziehl-Nielson stain Diagnosis (continued) Skin test : Tuberculin test Injecting PPD into skin positive ( 48- 72hrs.) PPD Testing PPD Testing Problems of interpretation of test : It indicates hypersensitivity to bacilli but does not differentiate infection from active disease False negative in Miliary TB , AIDS, sarcoidosis some viral diseases , Hodgkin’s disease , malnutrition… False positive in atypical mycobacterial infection Parasitic Infections in the Lung : Hydatid Disease : Common in mediterranean & middle east countries Infection by larval stage of Eccinococcus Granulosis Tape worm. Adult is in dogs eggs Intermediate stage ( Larva) in sheep & humans Mainly affects liver but other organs too Lung, Brain,…. Etc May be accompanied by eosinophilia Diagnosis by MRI & CT Forms a large unilocular cyst lined by eosinophilic laminated membrane from which scoleces develop ( Daughter cysts) In lung may be incidentally discovered May be infected or ruptured Treatment is surgical removal