* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Anaerobic Bacteria
Survey
Document related concepts
Transcript
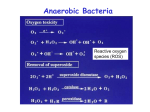
Anaerobic Bacteria Category Spore-forming: rod, Gram (+)--- Clostridium Nonspore-forming: see next slides Category Spore-forming: rod, Gram (+)--- Clostridium Nonspore-forming: Rod, Gram (+) Propionibacterium丙酸菌属 Rod, Gram (-) Cocci, Gram (+) Cocci, Gram (-) Bifidobacterium Lactobacillus Eubacterium Actinomyces Bacteroides Fusobacterium梭菌属 Campylobacter Peptococcus Peptostreptococcus Veillonella Clostridium Species The clostridia are opportunistic pathogens. Nonetheless, they are responsible for some of the deadliest diseases including gas gangrene, tetanus and botulism. Less lifethreatening diseases include pseudomembranous colitis (PC) and food poisoning. cause disease primarily through the production of numerous exotoxins. perfringens, tetani, botulinum, difficile Clostridium Tetani Pathogenesis of tetanus caused by C tetani General introduction C tetani is found worldwide. Ubiquitous in soil, it is occasionally found in intestinal flora of humans and animals C.tetani is the cause of tetanus,or lockjaw. When spores are introduced into wounds by contaminated soil or foreign objects such as nails or glass splinters BIOCHEMICAL CHARACTERISTICS Morphology: long and slender; peritrichous flagella,no capsule, terminal located round spore(drum-stick apperance), its diameter greater than vegetative cell. Culture:obligate anaerobic; Gram(+); swarming occures on blood agar, faint hemolysis. Biochemical activities:does not ferment any carbohydrate and proteins. Resistance: tolerate boiling for 60 min.alive several ten years in soil. Classification and Antigenic Types: C tetani is the only species. There are no serotypes 2-5 x 0.3-0.5um Pathogenicity No invasiveness; toxemia (exogenous infection) produces two exotoxins: tetanolysin, and tetanospasmin(a kind of neurotoxin, toxicity strong) The actions of tetanospasmin are complex and involve three components of the nervous system: central motor control, autonomic function, and the neuromuscular junction. retrograde transport to (CNS) delitescence:a few days to several weeks The two animal species most susceptible to this toxemia are horses and humans. Clostridium tetani -Tetanospasmin disseminates systemically binds to ganglioside receptors • inhibitory neurones in CNS glycine • neurotransmitter stops nerve impulse to muscles spastic paralysis痉挛性麻痹 severe muscle contractions and spasms can be fatal Tetanospasmin Clinical Manifestations The initial symptom is cramping and twitching of muscles around a wound. The patient usually has no fever but sweats profusely and begins to experience pain, especially in the area of the wound and around the neck and jaw muscles (trismus). Portions of the body may become extremely rigid, and opisthotonos角弓反张(a spasm in which the head and heels are bent backward and the body bowed forward) is common. Complications include fractures, bowel impaction, intramuscular hematoma, muscle ruptures, and pulmonary, renal, and cardiac problems Clinical Manifestations DISEASE CLINCAL MANIFESTATIONSA Generalized Involvement of bulbar and paraspinal muscles(trismus or lockjaw, risus sardonicus, difficulty swallowing, irritability, opisthotonos);involvement of autonomic nervous system(sweating, hyper thermia, cardiac arrhythmias, fluctuations in blood pressure) Cephalic Primary infection in head,particularly ear;isolated or combined involvement of cranial nerves, particularly seventh cranial nerve; very poor prognosis Localized Involvement of muscles in area of primary injury; infection may precede generalized disease; favorable prognosis Neonatal Generalized disease in neonates; infection typically originates from umbilical脐带 stump;very poor prognosis in infants whose mothers are nonimmune Tetanus. Epidemiology 1 million cases of tetanus occur annually in the world,with a mortality rate ranging from20% to 50%. But rare in most developed countries. In some developing countries, tetanus is still one of the ten leading causes of death, and neonatal tetanus accounts for approximately one-half of the cases worldwide. In less developed countries, approximate mortality rates remain 85% for neonatal tetanus and 50% for nonneonatal tetanus. In the United States, intravenous drug abusers have become another population with an increasing incidence of clinical tetanus In untreated tetanus, the fatality rate is 90% for the newborn and 40% for adults. Immunity Humoral immunity(antitoxin) There is little, if any, inate immunity and the disease does not produce immunity in the patient. Active immunity follows vaccination with tetanus toxoid Diagnosis Diagnosis is primarily by the clinical symptoms (above). The wound may not be obvious. C tetani can be recovered from the wound in only about one-third of the cases. It is important for the clinician to be aware that toxigenic strains of C tetani can grow actively in the wound of an immunized person. Numerous syndromes, including rabies and meningitis, have symptoms similar to those of tetanus and must be considered in the differential diagnosis. Vaccination • infant • DPT (diptheria, pertussis, tetanus) • tetanus toxoid – antigenic – no exotoxic activity Control The offending organism must be removed by local debridemen清创 术 toxoid TAT; Metronidazole (For more serious wounds) AIDS patients may not respond to prophylactic injections of tetanus toxoid C. perfringens • soil, fecal contamination • gas gangrene – swelling of tissues – gas release * fermentation products • wound contamination Toxins toxin Biological Feature Types of Toxins A B C D E lecithinase; increase the vascular permeability; hemolytic; produces necrotizing activity + + + + + Necrotizing activity, induces hypertension by causing release of catecholamines. - + + - - increase the permeability of gastrointestinal wall - - - + - Necrotizing activity; increase the vascular permeability - - - - + Toxins Many of these toxins have lethal, necrotizing, and hemolytic properties; The alpha toxin produced by all types of C. perfringens, is a lecithinase that lyses erythrocytes, platelets, leukocytes, and endothelial cells. And its lethal action is proportionate to the rate at which it splits lecithin to phosphorylcholine and diglyceride. The theta toxin has similar hemolytic and necrotizing effects. DNAase, hyaluronidase, a collagenase are also produced Enterotoxin Many strains of type A produce enterotoxin, which is a heat-labile protein and destroyed immediately at 100 ℃. Trypsin treatment enhances the toxin activity threefold. The toxin is produced primarily by type A strains but also by a few type C and D strains. It disrupts ion transport in the ileum(primarily) and jejunum by inserting into the cell membrane and altering membrane permeability. As superantigen. Pathogenesis •Tissue degrading enzymes – lecithinase [ toxin] – proteolytic enzymes – saccharolytic enzymes • Destruction of blood vessels • Tissue necrosis • Anaerobic environment created • Organism spreads Without treatment death occurs within 2 days effective antibiotic therapy debridement anti-toxin amputation & death is rare Gas gangrene Gas gangrene is a life-threatening disease with a poor prognosis and often fatal outcome. Initial trauma to host tissue damages muscle and impairs blood supply----lack of oxygenation Initial symptoms : fever and pain in the infected tissue.; more local tissue necrosis and systemic toxemia. Infected muscle is discolored (purple mottling) and edematous and produces a foulsmelling exudate; gas bubbles form from the products of anaerobic fermentation. Gas gangrene As capillary permeability increases, the accumulation of fluid increases, and venous return eventually is curtailed. As more tissue becomes involved, the clostridia multiply within the increasing area of dead tissue, releasing more toxins into the local tissue and the systemic circulation. Food poisoning Enterotoxin producing strains. These bacteria are found in mammalian faeces and soil. Small numbers of the bacteria may also be found in foods and they may propagate rapidly to dangerous concentrations if the food is improperly stored and handled. Food poisoning more than 108 vegetative cells are ingested and sporulate in the gut, the toxins can act rapidly in the body, causing severe diarrhea in 6-18 hours, dysentery, gangrene, muscle infections The action of C. perfringens enterotoxin involves marked hypersecretion in the jejunum and ileum, with loss of fluids and electrolytes in diarrhea. Cellulitis, Fasciitis Cellulitis, Fasciitis Fasciitis : a rapidly progressive, destructive process in which the organisms spread through fascial plan es. Fasciitis causes suppuration and the formation of gas Absense of muscle involvement rapidity Necrotizing Enteritis Rare, acute necrotizing process in the jejunum Abdominal pain, bloody diarrhea, shock, and peritonitis Mortality: 50% Beta-toxin-producing C. perfringens type C Septicemia Who is at risk? Surgical patients; patient after trauma with soil contamination. People who ingest contaminated meat products (without proper refrigeration or reheating to inactivate endotoxin) Epidemiology C. perfringens type A: the intestinal tract of humans and animals, soil and water contaminated with feces. forms spores under adverse environmental conditions and can survive for prolonged periods. Type B to E strains colonize the intestinal tract of animals and occasionally humans. Epidemiology Type A: gas gangrene, soft tissue infections and food poisoning Type C: enteritis; necroticans Laboratory identification • lecithinase production Double Hemolysis Circles C. botulinum Biological Features Anaerobic Gram-positive rod-shaped sporeformer produces a protein neurotoxic. soil, sediments of lakes, ponds, decaying vegetation. intestinal tracts of birds, mammals and fish. Division ---A, B, C1, D, E, F, and G. ---type A. 62% ---Not all produce toxin. ---C and D not ---G plasmid encoded. Transmission ---spores heat resistant. canning. anaerobic environment ---Botulism eating uncooked foods spores ---GI, duodenum, blood stream, neuromuscular synapses. Virulence factors ---bacterial protease ---light chain,A,50 kDa; heavy chain,100kDa. ---disulfide bond. ---A potent toxin binds peripheral nerve receptors • acetylcholine neurotransmitter inhibits nerve impulses flaccid paralysis death Botulinum • respiratory • cardiac failure toxin Botulinum toxin Bioterrorism • not an infection • resembles a chemical attack • 10 ng can kill a normal adult Epidemiology ---4: foodborne, infant, wound, undetermined. ---Certain foods; wound not. ---Foodborne botulism, consumption. ---Infant botulism, 1976, under 12m. ---ingestion, colonize and produce toxin in the intestinal tract of infants. honey. ---increased. ---internationally recognized. Clinical syndromes ---18-36 hours: ---weakness, dizziness,dryness of the mouth. ---Nausea,vomiting. ---Neurologic features: blurred vision, inability to swallow, difficulty in speech, descending weakness of skeletal muscles, respiratory paralysis. Botulism(肉毒中毒) food poisoning • rare • fatal germination of spore inadequately sterilized canned food • home not an infection Infection with C. botulinum Neonatal botulism • uncommon • the predominant form of botulism • colonization occurs no normal flora to compete unlike adult Wounds • extremely rare • an infection Immunity ---specifically neutralized, antitoxin. ---toxoided, make good antigens. ---does not develop, amount toxic. ---Repeated occurrence. ---Once bound, unaffected by antitoxin. ---circulating toxin ,neutralized , injection of antitoxin. ---treated immediately with antiserum. ---multivalent toxoid,unjustified,infrequency. experimental vaccine. Diagnosis ---by clinical symptoms alone ---differentiation difficult. --- most direct and effective: serum or feces. ---most sensitive and widely used: mouse neutralization test. 48h. Culturing of specimens 5-7d. Treatment Individuals known to have ingested food with botulism should be treated immediately with antiserum. antibiotic therapy (if infection) • Vaccination will not protect hosts from botulism, however passive immunisation with antibody is the treatment of choice for cases of botulism. Prevention ---proper food handling and preparation. --- spores survive boiling (100 degrees at 1 atm) 1h. ---toxin heat-labile, boiling or intense heating, inactivate the toxin. ---bulge, gas, spoiled. C. difficile • • • • • After antibiotic use Intestinal normal flora --greatly decreased Colonization occurs Enterotoxin secreted Pseudomembanous colitis Pseudomembranous Colitis Pseudomembranous colitis (PC) results predominantly as a consequence of the elimination of normal intestinal flora through antibiotic therapy. Symptoms include abdominal pain with a watery diarrhea and leukocytosis. "Pseudomembranes" consisting of fibrin, mucus and leukocytes can be observed by colonoscopy. Untreated pseudomembranous colitis can be fatal in about 27-44%. Therapy Discontinuation of initial antibiotic (e.g. ampicillin) Specific antibiotic therapy (e.g. vancomycin) Obligate (strict) anaerobes • • • • no oxidative phosphorylation fermentation killed by oxygen lack certain enzymes – superoxide dismutase * O2-+2H+ H2O2 – catalase * H2O2 H20 + O2 – peroxidase * H2O2 H20 /NAD to NADH Strict anaerobe infectious disease Sites throughout body Muscle, cutaneous/sub-cutaneous necrosis Abscesses Bacterial Flora of the Body Site Total Bacteria Ratio (per/ml or gm) Anaerobes:Aerobes Upper Airway Nasal Washings Saliva Tooth Surface Gingival Crevice 103-104 108-109 1010-1011 1011-1012 3-5:1 1:1 1:1 1000:1 Gastrointestinal Tract Stomach Small Bowel Ileum Colon 102-105 102-104 104-107 1011-1012 1:1 1:1 1:1 1000:1 Female Genital Tract Endocervix Vagina 108-109 108-109 3-5:1 3-5:1 Problems in identification of anaerobic infections • air in sample (sampling, transportation) – no growth • identification takes several days or longer – limiting usefulness • often derived from normal flora – sample contamination can confuse Virulence Factors 1. Anti-phagocytic capsule • Also promote abscess formation 2. Tissue destructive enzymes • B. fragilis produces variety of enzymes (lipases, proteases, collagenases) that destroy tissue Abscess Formation 3. Beta-lactamase production • B. fragilis – protect themselves and other species in mixed infections 4. Superoxide dismutase production • Protects bacteria from toxic O2 radicals as they move out of usual niche Characteristics of Anaerobic Infections 1. Most pathogenic anaerobes are usually commensals • Originate from our own flora 2. Predisposing Conditions • Breeches in the mucocutaneous barrier displace normal flora • Compromised vascular supply • Trauma with tissue destruction • Antecedent infection Characteristics of Anaerobic Infections 3. Complex Flora Multiple species • Abdominal Infection Avg of 5 species 3 anaerobic 2 aerobic • Less complex then nl flora • Fecal flora 400 different species Those predominant in stool are not infecting species • Veillonella, Bifidobacterium rarely pathogenic • Species uniquely suited to cause infection predominate 4. Synergistic Mixture of Aerobes & Anaerobes E. coli Consume O2 • Allow growth of anaerobes Anaerobes promote growth of other bacteria by being antiphagocytic and producing Blactamases Clues to Anaerobic Infection Infections in continuity to mucosal surfaces Infections with tissue necrosis and abscess formation Putrid odor Gas in tissues Polymicrobial flora Failure to grow in the lab 1. 2. 3. 4. 5. 6. BIOCHEMICAL KITS • e.g. API SYSTEM GAS CHROMATOGRAPHY • volatile fermentation products Bacteroides fragilis • Major disease causing strict anaerobic after abdominal surgery non-spore-former • Prominent capsule – anti-phagocytic – abscess formation • Endotoxin – low toxicity – structure different than other lipolysaccharide • Enterobacteriaceae (facultative anaerobes) – commonly cause disease – low numbers gut flora • Strict anaerobes – much less commonly cause disease – high numbers gut flora .