* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Fatal cardiac arrhythmias in patients with heart failure: Risk
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
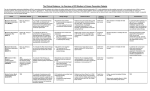
Fatal cardiac arrhythmias in patients with heart failure: Risk stratification, treatment and prevention Dr. Reginald Liew MA, MB BS (Hons), PhD, FRCP, FACC, FESC, FAsCC Director/ Senior Consultant Cardiologist The Harley Street Heart and Cancer Centre Mount Elizabeth Novena Specialist Centre, Singapore Outline of presentation • • • • • Incidence and epidemiology Risk stratification for SCD Role of ICDs for 1ry and 2ry prevention Catheter ablation and drug treatment Other considerations Outline of presentation • • • • • Incidence and epidemiology Risk stratification for SCD Role of ICDs for 1ry and 2ry prevention Catheter ablation and drug treatment Other considerations Incidence of Sudden Cardiac Death SCD in post MI patients • Atherosclerotic coronary artery disease remain the most important underlying substrate for accountable sudden cardiac death. • Survivors of myocardial infarction especially with left ventricular dysfunction, is the high risk population being focused on and where most of the data has been available. Events leading to SCD in post MI patients Liew R; Heart 2010 Outline of presentation • • • • • Incidence and epidemiology Risk stratification for SCD Role of ICDs for 1ry and 2ry prevention Catheter ablation and drug treatment Other considerations Which parameters will help identifying patients who require ICD? • • • • • • • • NYHA functional class Non-sustained VT QT dispersion and variability Cardiac autonomic modulation (HRV, BRS, HRT) Signal –averaged ECG Microvolt T wave alternans EP testing LVEF Signal averaged ECG •Late potential represents low amplitude high frequency electrical activity at the terminal portion of QRS. Thought to be due to slow conduction and delayed myocardial activation, a marker of ischemic substrate. •The prognostic value of SAECG had been reported. In MUSTT trial, patients with abnormal SAECG has higher rate of arrhythmic and total mortality (36% vs 13% 5 yr incidence) but the sensitiviy and specificity was inadequate to guide ICD therapy Liew R; Heart 2010 Imaging the substrate • Ischemia and scarring from CAD result in abnormal myocardial substrate and predispose to life-threatening arrhythmia • Traditional tools in assessing LVEF include 2D echocardiogram and radionuclide imaging • Cardiac MR has emerged as a promising tool in risk assessment arena, providing accurate measurements in LVEF and dimensions, perfusion abnormality, infarct size and viability assessment (DGE). DGE identified regional fibrosis in NICM and ICM and correlates with appropriate ICD Rx (Iles et al. JACC 2011) Correlation of myocardial scar on MRI with voltage map Images from UCLA arrhythmia centre Outline of presentation • • • • • Incidence and epidemiology Risk stratification for SCD Role of ICDs for 1ry and 2ry prevention Catheter ablation and drug treatment Other considerations Implantable cardioverter defibrillators • Useful to protect against sudden arrhythmic death, but have their own associated risks – Inappropriate shocks – Need for regular generator change – Risk of infection – May cause vicious cycle of further arrhythmias due to adrenergic drive • Risk/ benefit ratio needs to be discussed fully with pt and parents • General principles: – Indicated in pts after aborted SCD (2rd prevention) – Consider for 1ry prevention in patients at high risk of SCD Clinical trials of ICD therapy using LVEF as primary risk assessment tool Benefit of ICD for SCD is offset in early post MI Impact of ICD therapy is Time dependent Impact of ICD therapy is Time dependent • The benefit of ICD early vs late post MI does not seem to be similar. • Potent reduction in total mortality by ICD has been confirmed when implemented in a ICM population with remote MI. • Although SCD risk is highest early post MI, ICD does not impact total mortality. ICD merely changes the mode of death from arrhythmic death to nonarrhythmic/heart failure death. • It seems that remodelling of ventricle early post MI negates the ICD benefits, yet in late post MI when the substrate becomes stable with healed scar tissue, reentrant arrhythmia is the primary mechanism for mortality when ICD can significantly impact survival. ACCF/AHA/HRS 2012 focused updated Guidelines Device –based Therapy for Cardiac Rhythm Abnormalities ICD therapy is indicated in patients: • who are survivors of cardiac arrest due to ventricular fibrillation or hemodynamically unstable sustained VT after evaluation to define the cause of the event and to exclude any completely reversible causes. (Class I level A) • with structural heart disease and spontaneous sustained VT, whether hemodynamically stable or unstable. (Class I level B) • with syncope of undetermined origin with clinically relevant, hemodynamically significant sustained VT or VF induced at electrophysiological study. (Class I level B) ACCF/AHA/HRS 2012 focused updated Guidelines Device –based Therapy for Cardiac Rhythm Abnormalities ICD therapy is indicated in patients with: • LVEF less than or equal to 35% due to prior MI who are at least 40 days post-MI and are in NYHA functional Class II or III. (Class I level A) • LV dysfunction due to prior MI who are at least 40 days post-MI, have an LVEF less than or equal to 30%, and are in NYHA functional Class I. (Class I level A) • nonsustained VT due to prior MI, LVEF less than or equal to 40%, and inducible VF or sustained VT at electrophysiological study. (Class I level B) PRIMARY PREVENTION OF SCD WITH THE ICD European Society of Cardiology SUMMARY- SCD and ICDs in heart failure pts • At present, other than LVEF measured at least 40 days post MI, there is no non-invasive or invasive strategy that can reliably predict SCD risk and guide ICD therapy, especially soon after MI. • For early post MI patients, the management directive is to maximize optimal medical therapy and revascularization (early if not primary), and reevaulate LVEF at 40 days post MI or revascularization for indication of ICD . • For stable ischemic cardiomyopathy patient, LVEF still provide the most validated and powerful risk assessment to guide the need for prophylactic ICD. Outline of presentation • • • • • Incidence and epidemiology Risk stratification for SCD Role of ICDs for 1ry and 2ry prevention Catheter ablation and drug treatment Other considerations MANAGEMENT OF SUSTAINED VT IN PATIENTS WITH IHD DRUGS FOR THE TREATMENT OF VENTRICULAR ARRHYTHMIAS AND SCD • Other than beta-blockers, no other AADs have been shown in RCT to be effective in primary management of patients with lifethreatening ventricular arrhythmias and reducing the risk of SCD • Each drug can potentially cause adverse events, including pro-arrhythmia AMIODARONE IS NO BETTER THAN PLACEBO AT PREVENTING SCD Bardy et al. NEJM 2005 CATHETER ABLATION OF VT Catheter ablation of VT VT ablation versus escalation of anti-arrhythmic drugs- Sapp et al. NEJM July 2016 • Multicentre RCT in 259 pts with ischaemic cardiomyopathy, ICD and recurrent VT despite being on AADs • Randomised to VT ablation (132 pts) or escalation of AAD (amiodarone or mexiletine if already on 300mg amiodarone per day; 127 pts) • Primary end-point composite of death, VT storm, or appropriate ICD shock Sapp JL et al. N Engl J Med 2016;375:111-121 Defibrillator implantation in patients with nonischaemic systolic heart failureKober et al NEJM Aug 2016 • RCT of 556 patients with symptomatic systolic heart failure (LVEF ≤35%) not caused by coronary artery disease were assigned to receive an ICD, and 560 patients were assigned to receive usual clinical care (control group). • In both groups, 58% of the patients received CRT. • The primary outcome was death from any cause. The secondary outcomes were sudden cardiac death and cardiovascular death • No sig. difference in 1ry outcome (death from any cause) between ICD and control group. • Sig. reduction of SCD in ICD group (2ry outcome) Outline of presentation • • • • • Incidence and epidemiology Risk stratification for SCD Role of ICDs for 1ry and 2ry prevention Catheter ablation and drug treatment Other considerations MOLECULAR AUTOPSY IN SCD VICTIMS European Society of Cardiology 2015 Genes most commonly altered in cardiomyopathies Gene name Gene symbol Frequency (%) Hypertrophic cardiomyopathy Beta-myosin heavy chain MYH7 15–25 Cardiac myosin-binding protein C MYBPC3 15–25 Cardiac troponin T TNNT2 <5 Cardiac troponin I TNNI3 <5 Alpha-tropomyosin TPM1 <5 LIM-binding domain 3 LBD3 1–5 Ventricular regulatory myosin light chain MYL2 <2 Myosin light chain 3 MYL3 <1 Cardiac muscle alpha actin ACTC1 <1 Long QT syndrome Potassium channel, voltage KCNQ1 gated, member 1 (Kv7.1; LQT1) 40–55 Potassium channel, voltage gated, member 2 (Kv11.1; LQT2) KCNH2 30–45 Sodium channel, voltage gated, type V, α subunit (Nav1.5; LQT3) SCN5A 5–10 Arrhythmogenic right ventricular cardiomyopathy Plakophilin 2 PKP2 10–45 Desmoplakin DSP 10–15 Desmoglein DSG2 7–10 Desmocollin 2 DSC-2 2 Junction plakoglobin JUP <1 THE SUBCUTANEOUS ICD Bardy et al. NEJM 2010 SUBCUTANEOUS ICDs • • • • Effective at preventing SCD Avoids complications related to traditional transvenous systems Long term data lacking Not useful if pacing is required (including CRT) or if ATP is required for VT termination WEARABLE CARDIOVERTER DEFIBRILLATOR • No prospective randomized trials evaluating the device have yet been reported • Small case series, registries and case reports have reported successful use of the WCD in a small proportion of patients WEARABLE CARDIOVERTER DEFIBRILLATOR A recording from a LifeVest of an appropriate shock delivered to a patient with long-QT syndrome. The wearable defibrillator was prescribed after ICD extraction as a result of infection. All plates show the 2 channels used by the wearable defibrillator. WEARABLE CARDIOVERTER DEFIBRILLATOR Conclusions • Various methods for risk stratification of fatal arrhythmias in pts with heart failure - LVEF remains most widely used and featured in guidelines • ICDs can lower risk of SCD- timing is important • Medical therapy not effective to reduce SCD but can be useful to reduce ICD shocks • Catheter ablation of VT/ VF indicated for recurrent ventricular arrhythmias or ICD shocks; should be done in experienced EP centres • Newer options to consider- subcutaneous ICD, wearable cardioverter defibrillator (short term measure) Gleneagles Hospital, #02-38/41, Annexe Block 6A Napier Road, Singapore T +65 6472 3703 Email: [email protected] www.harleystreet.sg Mount Elizabeth Novena Specialist Centre #07-41, 38 Irrawaddy Road, Singapore T +65 6694 0050 Which parameters will help identifying patients who require ICD? • NYHA functional class and presence of nonsustained VT do not provide incremental value in risk assessment over other parameters such as LVEF. • In MADIT II and some small epidemiological studies, QT measurements had been shown to be associated with malignant ventricular arrhythmias. However the sensitivitiy was too low to be clinically useful. Which parameters will help identifying patients who require ICD? • Patients with depressed baroreflex sensitivity(BRS) <3ms/mmHg and depressed heart rate variability(HRV) SDNN<70ms had been shown to have higher total mortality (17% vs 2% with both tests normal). But neither of these tests had been shown useful in predicting arrhythmic death • Heart rate turbulence (HRT) show mixed results in trials. It predicts total mortality in EMIAT, MADIT II and Multicenter Post Infarct Program trials but there is limited data for its SCD prediction. DIAGNOSTIC WORKUP FOR PATIENTS PRESENTING WITH SUSTAINED VT/ VF DIAGNOSTIC WORKUP FOR PATIENTS PRESENTING WITH SUSTAINED VT/ VF Which parameters will help identifying patients who require ICD: Microvolt T Wave Alternans? • Microvolt electrical alternans is the variability of ECG waveform on alternate beats, as pathophysiological manifestation in serious heart disease or in normal subjects when heart rate is very rapid. • The T wave is measured at identical time relative to QRS in multiple consecutive complexes. Spectral analysis is used to differentiate minor alternation in T wave morphology at the alternans frequency from respiration and noise. • T-Wave Alternan (TWA) is measured during atrial pacing or exercise for a target heart rate of 110bpm to maxmize sensitivity and specificity. Microvolt T Wave Alternans? • Measures the variability of ECG waveform on alternate beats, as pathophysiological manifestation in serious heart disease or in normal subjects when heart rate is very rapid • Gehi et al. reported in a meta-analysis of cohort studies between 1990-2004 a harzard ratio of 3.8 with abnormal MTWA and NPV of 92% in ICM, 95% in NICM, and 99% in post MI patients. • However high discordance rate between 1 and 6 month post MI was reported by Oliveira et al. • 2 major trials in 2008 with ICD population – MASTER (Chow et al. JACC 2008) (n=575 ICM EF</=30%) – MTWA SCD-HeFT (Gold et al. Circ 2008) (n=490 ICM and NICM EF </=35%) – Both failed to show a difference in primary endpoint (SCD and ICD discharge) between test negative and non-negative (positive and indetermine) patients MTWA: failure to demonstrate a difference in primary endpoint •MTWA still lacks the reproducibility and predictive accuracy as sole parameters to predict SCD and need for ICD for post MI patients Which parameters will help identifying patients who require ICD:EP testing? • In the past, EP testing was considered the primary method for risk stratification for malignant ventricular arrhythmia. • The value of EP testing is challenged in MUSTT-EPS registry (n=1397) and MADIT II EP substudy (n=593). • Although EP testing does stratify CAD patients at risk of SCD, its ability to do so is only modest. – MUSTT-EPS: non-inducible = 12% arrhythmic death at 2 yr. (NPV 88% at 2 year) – MADIT II EP: non-inducible = 25.5% ICD Rx at 2 yr. (vs 29.4% for inducible patients NS) •The major finding of MUSTT-EPS registry is that 2 year and 5 year rate of cardiac arrest or death by arrhythmia in the non-inducible cohort were still 12% and 24%. Risk of SCD post MI is highest in the first month •Data from the VALIANT trial showed the SCD risk is highest in the first 30 days post MI •With each 5% decrease in LVEF, there was 21% increase in relative risk of SCD during this period •SCD risk decrease with time and plateau at 12 months equalized between different LVEF categories. •This temporal trend is also noted in combined analysis of other trials (EMIAT, CAMIAT, SWORD, TRACE, DIAMOND-MI) Causes of SCD among children and young adults- Bagnall et al, NEJM 2016 • CAD still most common cause • Among cases of unexplained SCD, genetic testing with autopsy helped identify cause