* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Metabolism of bilirubin and bile salts synthesis (uronic acid pathway
Biological aspects of fluorine wikipedia , lookup
Cell-penetrating peptide wikipedia , lookup
Peptide synthesis wikipedia , lookup
Nucleic acid analogue wikipedia , lookup
Genetic code wikipedia , lookup
Citric acid cycle wikipedia , lookup
Human digestive system wikipedia , lookup
Expanded genetic code wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Butyric acid wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Biosynthesis wikipedia , lookup
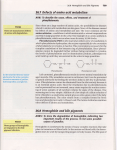
Metabolism of bilirubin and bile salts synthesis (uronic acid pathway and role of glucuronides) • • • • • • • • • Objectives At the end of the lecture, the student should be able to: Name the proteins which contain heme Explain turnover number of erythrocytes Describe the site of heme degradation Describe the fate of globin, Fe and porphyrin ring Discuss the role of microsomal heme oxygenase system– formation of bile pigments Appreciate the changing colour of a bruise Role of uronic acid cycle as a source of glucuronic acid Excretion of bile pigments Heme metabolism Heme is a constituent of: • Hemoglobin, myoglobin, cytochromes and other heme containing proteins • • • 6 g Hb is metabolised/ day Producing 350 mg bilirubin Heme metabolism takes place in reticuloendothelial cells of spleen, liver and bone marrow Heme oxygenase system • Globin part of hemoglobin is hydrolysed to produce amino acids which enter the body’s amino acid pool • Fe(ous) is oxidised to Fe(ic) and reutilised • Iron- free porphyrin ring is first converted to biliverdin (green) and then reduced to bilirubin (orange-red) • • • • • • Microsomal heme oxygenase system Cleaves the porphyrin ring of heme Requires NADPH as coenzyme Cyclic tetrapyrrole structure of heme is converted to linear structure (removal of 1 C atom as CO) A green pigment-BILIVERDIN– is formed Biliverdin is then reduced by biliverdin reductase (NAPDH dependent)to form red-orange bilirubin Changing colour of a bruise Conversion of Heme to Bilirubin Bilirubin • • • belongs among linear tetrapyrrols is excreted mainly with bile is insoluble in water but gets solubilised after its conjugation, e.g. with glucuronic acid • • • • • • • • • • Transport of bilirubin to liver Hydrophobic nature of bilirubin Restricted free movement of bilirubin in plasma forms Non-covalent complex with albumin Carried to liver due to polar nature of albumin Separated from albumin Enters hepatocytes in free form by active process Binds to ligandin or Z protein Uronic acid pathway Inside the hepatocytes, bilirubin is conjugated with glucuronic acid, which is provided by uronic acid pathway (UAP) UAP is a minor pathway of carbohydrate metabolism Glucuronic acid is an important product required for detoxification of drugs and for conjugation of steroid hormones and bilirubin before excretion in urine and bile • • • • • Fate of conjugated bilirubin in intestine Bacterial enzyme beta glucuronidase removes glucuronides from conjugated bilirubin (deconjugation) Subsequent reduction of the pigment produces a colourless compound called urobilinogen (URO) Most of URO remains in intestine and is excreted in feces as stercobilinogen Nearly 20% URO is absorbed from the intestine into portal circulation (subsequently excreted via kidneys into urine as urobinlin) A part of URO returns to liver and reaches gut again • • Plasma bilirubin Total bilirubin = 0.2- 1 mg/dl conjugated bilirubin = 0.1-0.4 mg/dl also called direct bilirubin, being water soluble reacts immediately with diazo reagent unconjugated (albumin bound) bilirubin is called indirect bilirubin. Being water insoluble, it has to be first extracted with methanol and then treated with diazo reagent Summary • • • Bile acids and bile salts Bile acids (24 C compounds) are synthesised from cholesterol (27 C) in hepatocytes and stored in gall bladder Nearly half of the cholesterol in body is converted to primary bile acids – cholic acid and chenodeoxycholic acid Primary bile acids lose OH groups to form secondary bile acids (deoxycholic acid and lithocholic acid respectively) Bile acids are formed from cholesterol: • • • • • • About 1 gram of cholesterol is eliminated from the body per day. Approximately half is excreted in the feces after conversion to bile acids. The remainder is excreted as cholesterol. The primary bile acids are synthesized in the liver from cholesterol. These are cholic acid and chenodeoxycholic acid. In the liver, both primary and secondary bile acids are conjugated with glycine or taurine to form bile salts: thus Cholic acid + glycine glycocholic acid lithocholic acid + glycine glycolithocholic acid Cholesterol bile acids A) addition of OH group(s) to the steroid ring B) removal of 3 C atoms from side chain C) reduction of ring B D) oxidation in the side chain to form a –COOH group Cholic acid = 3,7, 12 cholanic acid • • • • • • References Harper’s Medical Biochemistry, 28th ed D Puri, Textbook of Medical Biochemistry, 2nd ed