* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download pathophysiology
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart failure wikipedia , lookup
Aortic stenosis wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
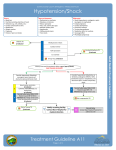
Jatene procedure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
PATHOPHYSIOLOGY Name Homework for Chapter 24, Part 2 – Alterations of Cardiovascular Function: Diseases of the Heart Wall, Heart Disease and Shock Instructions: Use your lecture notes and textbook to find the answers to these questions. When finished, enter your answers on the electronic version of the homework posted on Canvas. You may do this up to three times until you are happy with your grade. 1. Which of the following conditions is caused by the collection of fluid in the pericardial sac, resulting in tamponade? A) Pericardial rub B) Pericardial effusion C) Cardiomyopathy D) Constrictive pericarditis 2. Radiation therapy, hemochromatosis and amyloidosis could all result in: A) dilated cardiomyopathy B) asymmetrical septal hypertrophy C) hypertensive cardiomyopathy D) restrictive cardiomyopathy 3. Aortic stenosis results in the incomplete emptying of the: A) right atrium. B) right ventricle. C) left atrium. D) left ventricle. 4. In the elderly, aortic stenosis usually results from which of the following conditions? A) congenital disorders. B) rheumatic heart disease. C) degeneration and calcification of the valve. D) Marfan syndrome. 5. Which of the following valve disorders is likely to result in left ventricular failure? A) Aortic stenosis B) Aortic regurgitation C) Mitral regurgitation D) All of the above 6. Infective endocarditis is most often caused by: A) viruses. B) bacteria. C) fungi. D) autoimmunity. 7. Manifestations of increased left atrial and pulmonary venous pressures in left (congestive) heart failure include: A) syncope. B) weak pulses and decreased skin temperature. C) oliguria. D) dyspnea and cough. 2 8. A patient is diagnosed with chronic pulmonary disease and elevated pulmonary vascular resistance. Which of the following heart failures generally results from this condition? A) Right heart failure B) Left heart failure C) Low-output failure D) High-output failure 9. Of the following diseases, which is the most common cause of right heart failure? A) Primary hypertension B) Infective endocarditis C) Left heart failure D) Pericarditis 10. Which problem is a pathophysiological consequence common to all shock states? A) Hypoperfusion B) Vasoconstriction C) Pulmonary edema D) Hypertension 11. A consequence of switching from aerobic to anaerobic cellular metabolism during shock states is: A) increased ATP production. B) cellular dehydration. C) lactic acidosis. D) free radical formation. 12. Which of the following conditions is NOT a potential cause of cardiogenic shock? A) Tension pneumothorax B) Spinal cord injury C) Tamponade D) Cardiac arrhythmias 13. Which of the following shock states manifests with tachycardia, vasoconstriction, and movement of large volumes of interstitial fluid to the vascular compartment? A) Anaphylactic B) Hypovolemic C) Neurogenic D) Septic 14. Causes of hypovolemic shock include all of the following EXCEPT: A) dehydration. B) blood loss. C) brainstem injury. D) diuresis. 15. Clinical manifestations of hypovolemic shock include all of the following EXCEPT: A) pulmonary edema. B) tachycardia. C) hypotension. D) oliguria. 16. Which of the following shock states is characterized by vasodilation of the systemic arteries? A) Hypovolemic B) Cardiogenic C) Distributive D) All of the above 3 17. Neurogenic shock is caused by: A) spinal cord injuries below T6. B) inhibition of the parasympathetic nervous system. C) injury to the cerebral cortex. D) a lack of sympathetic activity. 18. Which of the following pathophysiological events causes the severe hypotension observed in neurogenic shock? A) Increased capillary permeability B) Diuresis C) Decreased peripheral vascular resistance D) All of the above 19. Which of the following shock states is characterized by acute, severe bronchoconstriction? A) Cardiogenic B) Anaphylactic C) Hypovolemic D) All of the above 20. Anaphylactic shock occurs in response to severe: A) viral infections. B) allergic reactions. C) brain injuries. D) burn injuries. 21. Anaphylactic shock manifests with the rapid onset of which set of symptoms? A) Bradycardia, decreased arterial pressure, and oliguria B) Dyspnea, hypotension, and urticaria C) Hypertension, anxiety, and tachycardia D) Fever, hypotension, and erythematous rash 22. What is the primary cause of hypotension in early stages of septic shock? A) Blood loss B) Arterial vasodilation C) Activation of the parasympathetic nervous system D) Heart failure 23. High levels of which molecule contributes to the pathophysiology of septic shock? A) Nitric oxide B) Angiotensin II C) Activated protein C D) Epinephrine 24. Which set of clinical manifestations is highly characteristic of a septic shock state? A) Tachycardia, generalized edema, and warm skin B) Confusion, bradycardia, and truncal rash C) Severe respiratory distress, jugular venous distention, and chest pain D) Decreased cardiac output, hypertension, and poor skin turgor 25. The most common cause of multiple organ dysfunction syndrome (MODS) is: A) myocardial infarction. B) septic shock. C) chronic pulmonary disease. D) autoimmune disease. 4 26. MODS is defined as the progressive dysfunction of two or more organ systems resulting from: A) a drug overdose. B) severe hemorrhaging. C) an uncontrolled inflammatory response. D) myocardial depression. 27. In MODS, which of the following events contribute to organ failure? A) Microvascular clotting B) Interstitial edema C) Exhaustion of fuel supply D) All of the above Critical Thinking Questions: 28. The congenital disorder called tetralogy of Fallot involves stenosis of the pulmonary semilunar valve. Which of the following effects would most directly result from this? A) hypertrophy of the left ventricular wall B) hypertrophy of the right ventricular wall C) dilation of the left atrium D) regurgitation of the tricuspid valve 29. Many valvular stenosis and regurgitation disorders in adults have a common etiology. Which of the following can cause both types of valve dysfunction? A) Rheumatic heart disease B) Syphilis infection C) Connective tissue disorders D) Heart failure 30. Congestive heart failure (CHF) results in which of the following? A) Increased left ventricular preload B) Increased ejection fraction C) Decreased right ventricular preload D) Decreased right ventricular end-diastolic pressure 31. In shock, how does the body maintain blood glucose levels once available glucose and glycogen stores are used up? A) By stimulating the release of glucose stores from the spleen B) By breaking down protein to fuel gluconeogenesis C) By converting urea and ammonia to glucose D) By inhibiting the release of cortisol and thyroid hormone 32. Which of the following conditions presents the most significant risk factor for developing septic shock? A) Use of immunosuppressant medications B) History of severe allergies C) Diagnosed with chronic congestive heart failure D) Genetic predisposition to disorders of hemostasis