* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Clinical guidance for the Management of patients with confirmed
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
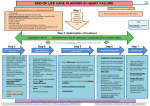
Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire Reference No: Version: 2.0 Ratified by: Date ratified: Name of originator/author: LCHS Heart Failure Complex Case Managers Name of responsible committee/individual: Clinical Governance Committee Date issued: June 2010 Review date: June 2012 Target audience: LCHS Distributed via: myMail Website 1 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Lincolnshire Community Health Services Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire – June 2010 Version Control Sheet Version Section/Para/ Appendix Version/Description of Amendments Date Author/Amended by 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 2 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Lincolnshire Community Health Services Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire – June 2010 Contents i) Version Control Sheet ii) Policy Statement SECTION PAGE 1 Summary of the purpose of the guidance 5 2 Indications for the use of the guidance 5 3 Associated Policies/Guidance 5 4 Contents 6 5 Useful Weblinks/Contacts 39 6 Other useful information 39 7 Audit/Monitoring of policy implementation 43 8 Implementations Strategy 43 9 References 40-42 3 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Lincolnshire Community Health Services Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire Policy Statement Background: This Clinical guidance outlines the diagnosis and clinical management for patients with a diagnosis of chronic heart failure. Statement: The guidance outlines a series of algorithms to support the management of patients with a diagnosis through end of life. Responsibilities Training The heart failure Complex Case Managers plan to deliver education regarding the management of patients with chronic heart failure which is based on the guidance. Dissemination: This guidance will be distributed via My mail and available on the NHS Lincolnshire website Resource implication: The clinical guidance will be further reviewed and amended in light of the latest NICE guidance (2010) once services have been commissioned to implement the guidance 4 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Summary of the purpose of the Guidance The purpose of this document is to provide guidance and a pathway for the treatment of patients with heart failure. The guidance is separated into two parts, the first addresses best practice in the clinical management of heart failure itself and the second focuses on management of symptoms commonly experienced in advanced heart failure and is concerned with palliative and supportive care. The guidance takes the form of a series of algorithms supporting the optimal pharmacological and non pharmacological management including appropriate referral pathways to specialist heart failure services. The term Heart Failure Complex Case Manager will be used throughout the (HFCCM). The role is a specialist nursing role incorporating complex case management, clinical assessment, diagnosis, non-medical prescribing and management of patients with chronic heart failure. The role meets the educational standards as set out by the British Heart Foundation. The term GPsi will be used throughout indicating the role of a general Practitioner with a special interest in heart failure Indications for the use of the Clinical Guidance The algorithms should be used in conjunction with the associated national standards and NICE guidance in order to support the stabilisation of a patient‘s heart condition through optimising treatment, providing support and where necessary palliative care. Associated Policies/ Guidance National Institute for Clinical Excellence (NICE), 2003, Management of chronic heart failure in adults in primary and secondary care. Department of Health (2000), Heart Failure, Chapter Six, National Services Framework for Coronary Heart disease Cheshire West Primary Care Trust (2004), Clinical Guidance for the Management of Patients with suspected or confirmed Heart Failure. British National Formulary Greater Glasgow NHS Board (June 2001), Medical Therapy Guidelines Heart Failure Protocol (February 2005), Gaynor Rickell, Swallowbeck Surgery, North Hykeham ULHT Heart Failure Nurse Services Protocols and PGD‘s, ULHT National Instutute for Health and clinical Excellence (2010) Chronic Heart Failure, Management of Chronic heart failure in adults in primary and secondary care. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure (2008) 5 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Review date: June 2012 Contents: Diagnosis and Management of Chronic Heart Failure ALGORITHM FOR THE MANAGEMENT OF „SUSPECTED‟ AND „CONFIRMED‟ HEART FAILURE (LEFT VENTRICULAR SYSTOLIC DYSFUNCTION) IN PRIMARY CARE BASED ON NICE GUIDELINES JULY 2003 ........................................ 7 ALGORITHM FOR PHARMACOLOGICAL TREATMENT OF LEFT VENTRICULAR SYSTOLIC DYSFUNCTION ................. 8 ALGORITHM FOR THE USE OF AN ACE INHIBITOR FOR „CONFIRMED‟ HEART FAILURE IN PRIMARY CARE BASED ON NICE GUIDELINES 2003. .................................................................................................................................. 9 ALGORITHM FOR USE OF BETA BLOCKERS FOR „CONFIRMED HEART FAILURE IN PRIMARY CARE BASED ON NICE GUIDELINES 2003 ................................................................................................................................................. 10 ALGORITHM FOR THE USE OF ANGIOTENSION RECEPTOR ANTAGONISTS (ARB) FOR CONFIRMED HEART FAILURE IN PRIMARY CARE BASED ON CHARM 2003 ........................................................................................................... 11 ALGORITHM FOR THE USE OF DIURETICS FOR CONFIRMED HEART FAILURE IN PRIMARY CARE........................... 12 ALGORITHM FOR THE USE OF SPIRONOLACTONE FOR „CONFIRMED‟ HEART FAILURE IN PRIMARY CARE BASED ON NICE GUIDELINES 2003 ....................................................................................................................................... 13 ALGORITHM FOR THE USE OF METOLAZONE FOR „CONFIRMED‟ HEART FAILURE IN PRIMARY CARE .................. 14 ALGORITHM FOR THE USE OF CARDIAC SYNCHRONISATION (CRT) THERAPY &/OR INTERNAL CARDIOVERTER DEFIBRILLATORS (ICD), OR BOTH (CRT-D) BASED ON TECHNOLOGY APPRAISAL GUIDANCE 120 & 95 .............. 15 ALGORITHM FOR NON PHARMACOLOGICAL MANAGEMENT FOR „CONFIRMED‟ HEART FAILURE IN PRIMARY CARE ................................................................................................................................................................... 15 Management of Advanced Heart Failure MANAGEMENT OF SYMPTOMS COMMONLY EXPERIENCED IN ADVANCED HEART FAILURE ................................... 17 WHEN DOES A HEART FAILURE PATIENT BECOME “PALLIATIVE”? ...................................................................... 18 ISSUES FOR CONSIDERATION WHEN ASSESSING PATIENT‟S NEEDS ........................................................................ 19 MANAGEMENT OF SUSPECTED ACUTE CONFUSION / DELIRIUM ........................................................................... 21 MANAGEMENT OF BREATHLESSNESS ................................................................................................................... 22 MANAGEMENT OF CONSTIPATION ........................................................................................................................ 23 MANAGEMENT OF COUGH ................................................................................................................................... 24 MANAGEMENT OF FATIGUE ................................................................................................................................. 25 MANAGEMENT OF ITCHING .................................................................................................................................. 26 SPECIAL ISSUES FOR CONSIDERATION WHEN MANAGING PAIN IN HEART FAILURE............................................. 27 MANAGEMENT OF NAUSEA AND VOMITING......................................................................................................... 28 MANAGEMENT OF PERIPHERAL OEDEMA.............................................................................................................. 29 MANAGEMENT OF POOR APPETITE AND WEIGHT LOSS/ CACHEXIA..................................................................... 30 PSYCHOLOGICAL CONCERNS ............................................................................................................................... 31 MANAGEMENT OF SLEEP DISTURBANCE AND INSOMNIA ..................................................................................... 32 MANAGEMENT OF STOMATITIS / SORE MOUTH ................................................................................................... 33 MEDICINES MANAGEMENT IN ADVANCED HEART FAILURE ................................................................................ 34 MANAGEMENT OF ANAEMIA/GOUT ..................................................................................................................... 34 PATHWAY FOR ADVANCE CARE PLANNING IN PATIENTS WITH CHRONIC HEART FAILURE .................................. 36 IATROGENIC PROBLEMS ....................................................................................................................................... 37 PATHWAY FOR DEACTIVATION OF IMPLANTABLE CARDIOVERTER DEFIBRILLATORS AT END OF LIFE ................ 38 USEFUL WEBLINKS/ CONTACTS ........................................................................................................................... 39 OTHER USEFUL INFORMATION ............................................................................................................................. 39 AUDIT/ MONITORING OF POLICY IMPLEMENTATION ............................................................................................ 43 IMPLEMENTATION STRATEGY .............................................................................................................................. 43 6 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the management of „Suspected‟ and „Confirmed‟ Heart Failure (Left Ventricular Systolic Dysfunction) in Primary Care based on NICE guidelines July 2003 If symptoms and/or signs suggestive of heart Failure/Left Ventricular Systolic Dysfunction (LVSD) Bloods – U&E, FBC, Glucose, TFT‘s, LFT‘s, Lipids: if abnormal investigate and treat accordingly ECG- IF ECG abnormal, or } GP refers for Chest X-ray- cardiomegaly or congestion } Echocardiography IF ECG and CXR normal, echocardiography usually not indicated (consider other cause of symptoms) Echo negative Consider other cause of symptoms Echocardiography Cardiologist confirms LVSD- 1 Patients discharged from hospital with diagnosis of LVSD Determine cause of LSVD -Ischaemic heart disease -hypertension -Valvular heart disease -Cardiomypathy -Myocarditis -Arrhythmia -Other 1. 2. 3. 4. 5. 6. 7. 8. Primary Care Informed of Diagnosis Add to Heart Failure Register (read code G5yy9) First Consultation-2 Patient informed of diagnosis by GP or Nurse Practitioner competent in Heart Failure Agree Clinical Management plan Information booklet Optimising pharmacological treatment Blood tests 1. Assessment and management of decompensated patient. 2. Optimisation of medication in collaboration with primary team and cardiologist. 3. Palliative care input Also available for telephone advice on management issues for Multi-Disciplinary Team Not all patients need referral to Community heart Failure Service or Cardiologist No Is patient on optimum pharmacological treatment and stable? Review as clinically indicated or as a minimum annually Review Date June 2012 I - No limitation of physical activity II - Slight limitation Ordinary activities cause symptoms III - Marked limitation. Less than ordinary activity causes symptoms, but comfortable at rest. IV - Unable to perform any activity. May have symptoms at rest Consider referral to Heart Failure Complex Case Manager/ GPsi 2/52 wk review by GP or Nurse Practitioner competent in Heart Failure in Primary Care Education and advise on chronic Heart Failure Consider referral to Expert Patient Programme Clinical Status Optimising pharmacological treatment Check renal function Flu and pneumovax vaccines NYH classification I-IV Review as indicated for pharmacological optimisation Yes New York Heart Association (NYHA) Class Consider Cardiology referral (if any of the following) 1. Patients with heart failure age< 65 years 2. Ongoing symptoms despite optimal medications 3. Failure to respond to treatment 4. Arrhythmia 5. Significant valvular heart disease 6. LSVD due to IHD and candidate for revascularisation 7. Congenital heart disease 7 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for pharmacological treatment of Left Ventricular Systolic Dysfunction New diagnostic Step1 – Start ACE inhibitor and titrate upwards See Algorithm for ACE Inhibitor (page 9) Add diuretic. Diuretic therapy is likely to control congestive symptoms and fluid retention. Add digoxin. If a patient in sinus rhythm remains symptomatic despite therapy with a diuretic. ACE inhibitor (or angiotensin II receptor antagonist) and beta blocker if a patient is in atrial fibrillation then use first line therapy Step 2- Add beta blocker and titrate upwards See Algorithm for beta blocker (page 10) Step 3- Add spironolactone If patient remains moderately to severely symptomatic despite optimal therapy listed above See Algorithm for spironolactone (page 13) Or if ACE inhibitor not tolerated e.g. due to severe cough. Consider angiotensin II receptor antagonist For advice, refer to Heart Failure Complex Case Manager/ GPsi +/_ Cardiologist Telephone or written advice rather than an outpatient review will often be sufficient N/B Consider adding Angiotensin II receptor antagonist to an ACE I when patients remain either symptomatic/hypertension under cardiologist supervision/advice. 8 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the use of an ACE inhibitor for „Confirmed‟ Heart Failure in Primary Care based on NICE guidelines 2003. Confirmed Left Ventricular systolic Dysfunction (LVSD) Suitable for initiation of Angiotensin converting enzyme (ACE) inhibitor Step 1- Initiation of ACE inhibitor Stop potassium supplements/ Potassium sparing diuretics (because of risk of hyperkalaemia) with the possible exception of spironolactone or Explerenone. If possible stop NSAID (because of risk of renal dysfunction) Before starting ACE inhibitor, educate patient about purpose, benefits and possible side effects of medications(ie dizziness, light-headedness, cough). Start with low dose ACE inhibitor Step 2- Review after 1-2 weeks Check U&Es at 10 days Check for adverse effects Symptomatic hypotension Renal dysfunction (rise in Creatinine to 200umol/l) Hyperkalaemia (rise in potassium to >5.5mmol/l) Intolerable cough (NOT just dry cough) Titrate to an intermediate dose if lower dose is tolerated and U&Es satisfactory If no adverse effects uptitrate to maximal tolerated dose. Check U&Es at 10 days and 4 weeks Step 2- Review patient once optimal dose reached Check U&Es Check for adverse effects Symptomatic hypotension Renal dysfunction (rise in Creatinine to > 200 umol/l Hyperkaleamia (rise in potassium to > 5.5 mmol/l Intolerable cough (NOT just dry cough) Review Date June 2012 Specialist advice required before staring ACE inhibitor if any of the following: Creatinine > 200 umol/I Urea > 12mmols Sodium< 130mmol/I Systolic arterial pressure < 100mm Hg Diuretic dose > Furosemide 80mg/ day or equivalent Known or suspected renal artery stenosis (eg peripheral vascular disease) or aortic stenosis Frail, Elderly Refer to Heart Failure Complex Case Manager/ GPsi +/- Cardiologist Telephone or written advice rather than an out patient review will often be sufficient If clinically unstable If clinically unstable If clinically unstable If TRULY intolerant of ACE inhibitor Consider angiotensin II receptor antagonist – e.g. Candesartan 4mg daily and uptitrate to 32mg daily as tolerated. Uptitrate similar to ACE inhibitor. Consider hydralazine 12.5mg qds and isosorbide dinitrate (ISDN) 20mg qds as and alternative. Increase to maximum daily dose of hydralazine 300mg and ISDN 160mg 9 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for use of Beta blockers for „confirmed Heart Failure in Primary Care based on NICE guidelines 2003 Confirmed Left Ventricular Systolic Dysfunction (LVSD) Suitable for initiation of beta blocker? Step 1- Assess whether suitable for treatment Monitor for signs of sodium and water retention e.g. oedema, lungs crackles, rise JVP or congestion on CXR. Monitor heart rate and blood pressure, i.e. heart rate >60bpm & no heart block on recent ECG and systolic blood pressure > 100mmHg Already on ACE inhibitor ± diuretics ± Digoxin Step 2- Assess where treatment should be initiated Nothecontraindications Identify most appropriate environment for the patient for beta block initiation. The options include; Initiation in primary care at GP surgery Initiation in primary care at home Primary care beta blocker mass initiation clinics Step 3- Initiation of Beta Secondary care blocker initiation as a day case Start with lowest recommended dose Educate the patient re: purpose, benefits and signs of worsening heart failure, e.g. patients should be taught how to weigh themselves correctly If taking other rate reducing medication, consider reduction in dose Adverse effects Marked fatigue- reassure patient of likely improvement in symptoms. Review- 2 weeks Worsening heart failure- Consider adding or increasing dose of loop diuretic Symptomatic hypotension- Consider reduction in dose of nitrates, calcium channel blockers or other vasodilators. Consider reducing diuretic if no congestion. If heart rate <50 bpm, obtain ECG. If taking other rate reducing medication, consider reduction in dose. Consider having dose of Beta Blocker If already taking a beta blocker continue drug unless patient becomes more symptomatic Beta blocker probably contraindicted Asthma, Severe COPD, Heart block. Sick-sinus syndrome, BP< 100mm/hg, Bradycardia <60bpm Primary Care Initiation either in GP surgery or in mass initiation clinics To be suitable for primary care initiation then the following should apply; 1. Definite echo proven diagnosis of heart failure due to left ventricular dysfunction. 2. Patient already on a loop diuretic 3. No beta blocker contraindications 4. No ongoing fluid overload/oedema Primary care initiation at home 1. Many patients are suitable for initiation at home; 2. Systolic BP. 120mm/Hg 3. Able bodied partner at home with telephone during initiation. 4. Patient/carer educated to call for help in unlikely (<2%) incidence of untoward symptoms. Secondary Care Initiation Refer to Heart Failure Complex Case Manager/ GPsi +/Cardiologist For initiation of beta blockers either in a mass initiation clinic in primary care or for initiation in secondary care as a say case. For other requests, telephone or written advice rather than an out patient view will often be sufficient. Step 4- Disease increase Beta blocker dosing schedule Please see BNF for recommended doses. Dose depending on patients condition and clinical judgement, e.g. in frail, elderly standard up Uptitration of dose following dose schedule (every 2-3 weeks) titration may need longer. Aim for target dose or, failing that, the highest tolerated dose Carvedilol dose schedule- Indications- treatment of stable mild to moderate chronic heart failure (NYHA I-III) in addition to standard Check U&Es and creatinine 1-2 weeks after initiation and 1-2 weeks therapy. after final dose titration Bisoprolol dose schedule- Indications- treatment of stable chronic moderate to severe heart failure (NYHA II-IV) with reduced ventricular function in addition to standard therapy. Nebivololbe considered in light of the seniors advice. trail in patient If intolerant of Beta Blocker- Consider reducing dose and review in 2 weeks. May Consider stopping or seeking specialist Beta over the age of 70specialist EFC 35%advise should be sought before treatment blockers should not be stopped suddenly unless absolutely necessary; ideally discontinuation. This algorithm is intended as a guide to care only and does not replace clinical judgement Revised HF guidance Nov. 2007 Prior to each uptitration check heart rate and blood pressure i.e. heart rate >50 bpm & systolic blood pressure > 100mmHg 10 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the use of angiotension receptor antagonists (ARB) for confirmed heart failure in primary care based on CHARM 2003 Confirmed Left Ventricular Systolic Dysfunction (LVSD) Suitable for ARB in addition to ACE I? If using instead of ACE I see ACE I Algorithm Asses whether suitable for treatment Patients who are still symptomatic despite therapy with an ACE I and Beta-blocker following specialist advice Specialist advice required before starting ARB if any of the following: Creatinine > 200umol/l Urea > 12mmols/l Sodium <130mmol/i Systolic arterial pressure < 100mm Hg Diurectic dose > Furosemide 80mg/day or equivalent Known or suspected renal artery stenosis (eg peripheral vascular disease) or aortic stenosis Frail, elderly Step 1- Review patient after 1-2 weeks Check U&Es at 10 days Check for adverse effects - symptomatic hypotension - renal dysfunction (rise in Creatinine to >200 umol/l) - hyperkalaemia (rise in potassium to >5.5 umol/l) Titrate to an intermediate dose if lower dose is tolerated and U&Es satisfactory If no adverse effects uptitrate to maximal tolerated dose Check U&Es at 10 days and 4 weeks Step 2- Review patient once optimal dose reached Refer to Heart Failure Complex Case Manager/ Cardiologist Telephone or written advice rather than an out patient review will often be sufficient Check U&Es Check for adverse effects -symptomatic hypotension Renal dysfunction (rise in creatinine to >200 umol/l) - hyperkalaemia (rise in potassium to > 5.5 mmol/l) 11 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the use of Diuretics for confirmed Heart Failure in Primary Care Confirmed Heart Failure Step1- Assess for signs and symptoms of water and sodium Retention Increased peripheral oedema- Raised JVP? Symptoms of breathlessness – PND and orthophoea? IF YES - Are they on a loop Diuretic? Yes No Up titrate to MAX 80mg furosemide or equivalent if clinically indicated Signs symptoms still present? Consider: latest U+Es/ CKD stage, BP/Hypotension and allergies, taking into account the risk/benefit ratio for the patient Suitable for Initiation of loop Diuretic? No Yes Yes Seek Specialist Advice No Aim to maintain on dry weight minimal dose required. Monitor U+Es Consider adverse effects/signs of dehydration? Dizziness Constipation Weight loss >1kg/day Reduced skin turgor Disproportionate rise in urea Patient Self Management Education: Weight, signs and symptom monitoring, medication information, when to seek help. Commence Loop diuretic -Furosemide 40mg od - Bumetanide 1mg od - Torasemide 10mg od Check U+Es 7-14 days after starting. Review in 1-2 weeks post initiation to reassess Symptoms still present Ensure titration and optimisation of other heart failure treatment. Consider referral to cardiologist and/or nephrologist Symptoms resolved NB: Diuretics should administered in combination with ACE inhibitors ARBs and B- blockers if tolerated 12 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the use of Spironolactone for „Confirmed‟ Heart Failure in Primary Care based on NICE guidelines 2003 Confirmed Left Ventricular Systolic Dysfunction (LVSD) Suitable for initiation of spironolactone? Step 1- Assess whether suitable for treatment Current or previous symptomatic heart failure (NYHA III-IV Already on optimal pharmacological treatment No evidence of hypovolaemia Inform patient of purpose, benefits & possible side effects of spironolactone Step 2- Check U&Es and review use of potassium supplements and potassium sparing diuretics Potassium must be < 5mmol/l to continue Consider stopping potassium supplements and potassium sparing diuretics Continue ACE inhibitor, loop diurectics, Digoxin and Beta blocker if also prescribed. Step 3 – Spironolactone initiation Commence at 25mg od Step 4 – Monitoring Repeat U&E at 1, 4, 8 & 12 weeks and every 3 months thereafter. Spironolactone contraindicted Serum potassium > 5mmol/l Serum Creatinine >220 Caution if mild to moderate renal impairment Caution if using in the frail and elderly if they are taking ACE inhibitors Adverse Effects Potassium > 5.5mmol/l - Stop spironolactone or reduce to 12.5 mg daily - Repeat bloods5-7 days later Intolerant to spironolactone - Consider reducing dose to 12.5mg daily or if necessary stop Gastro-intestinal disturbance - For diarrhoea, stop spironolactone and repeat U&Es at earliest convenience If clinically unstable If tolerant of spironolactone Consider Eplerenone particularly if the aetiology for heart failure is IHD and if post Myocardial Infarction Refer to Heart Failure Complex Case Manager/ GPsi+/Cardiologist Telephone of written advice rather than an out patient review will often be sufficient. 13 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the use of Metolazone for „Confirmed‟ Heart Failure in Primary Care Confirmed Left Ventricular Systolic Dysfunction (LVSD) Suitable for initiation of Metolazone Step 1- Assess whether suitable for treatment Patient not responding to a loop diuretic who presents one or more of the following signs/symptoms; Increase in weight > 2kg Evidence of leg oedema and / or abdominal distension Basal crepitations Gallop rhythm Raised Jugular Venous Pressure Increased dyspnoea Step 2 – Refer to Heart Failure Complex Case Manager Minimum interval between doses is 24 hours Minimum interval between increased doses is one day Educate the patient re: purpose, benefits and signs of worsening heart failure e.g. patients should be taught how to weight themselves correctly Advised to stop taking metolazone if weight loss > 3kg in 24 hours Metolazone contraindicted Weight loss > 3kg in 24 hours Blood pressure systolic < 90mmHG Serum urea or creatinine rising compared to previous results Sreum postassium < 3.5mmol Serum sodium < 125mmol Patients unwilling or able to self medicate Renal failure with anuria Pregnancy with breast feeding Liver Failure Porphyria Refer to Cardiologist 14 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for the use of cardiac synchronisation (CRT) therapy &/or internal cardioverter defibrillators (ICD), or both (CRT-D) Based on NICE technology appraisal guidance 120 & 95 Confirmed Left ventricular Systolic Dysfunction (LVSD) Suitable for CRT? Or ICD or CRT-D? Assess whether suitable for CRT? They are experiencing or have recently experienced class IIIIV symptoms. They are in sinus rhythm: - Either with a QRS duration of 150 ms or longer estimated by standard Electrocardiogram (ECG) - or with a QRS duration of 120149 ms estimated by ECG and mechanical dyssynchrony that is confirmed by echocardiography They have a left ventricular ejection fraction of 35% or less They are receiving optimal pharmacological therapy Assess whether suitable for ICD? „Secondary prevention‟ that is for patients who present, in the absence of a treatable cause, with one of the following: Having survived a cardiac arrest due to either ventricular tachycardia (VT) or ventricular fibrillation (VF) Spontaneous sustained VT causing syncope or significant haemodynamic compromise Sustained VT without syncope or cardiac arrest, and who have an associated reduction in ejection fraction (LVEF of less than 35%) (no worse than class III of the N.Y.H.A. functional classification of heart failure) N.B.This criteria does not cover the use of implantable defibrillators for non-ischaemic dilated cardiomyopathy Assess whether suitable for ICD „Primary prevention‟ that is for patients who have: Either LVSD with LVEF of less than 35% (no worse than class 3 N.Y.H.A and non-sustainable VT on Holter (24 hour ECG monitoring) and inductible VT on electrophysiological (EP) testing or LVSD with an LVEF of than 30%, no worse than class 3 N.Y.H.A and QRS duration of equal to or more than 120 milliseconds Asses whether suitable for CRT-D? Cardiac resynchronisation therapy with a defibrillator device (CRT-D) may be considered for people who fulfil the criteria for implantation of CRF device and who also separately fulfil the criteria for the use of an ICD device. If meets criteria refer for cardiology refer for cardiology assessment at tertiary centre N.B. Re primary prevention- A familial cardiac condition with a high risk of sudden death including long QT syndrome, hypertrophic cardiomyopathy, Brugada syndrome or arrythmogenic right ventricular dysplasia, or have undergone surgical repair of congenital heart disease. 15 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Algorithm for Non Pharmacological Management for „Confirmed‟ Heart Failure in Primary Care Prognosis-explore potential disease progression to include long term condition and symptom control Diagnosis Ensure patient/carer has received the Information Booklet, i.e. Living with Heart Failure Discuss Causes Explain Anatomy & Physiology Chest Examination – if competent listen for signs of clued overload Clinical Assessment Record Height, weight, BMI, BP & HR, respiration rate, Oedema Identify NYHA Classification Explain general symptom management including Paroxysmal Nocturnal Dyspnoea, Breathlessness, Cough, Sputum, Orthopnoea Fatigue including energy conversation and advise on pacing activities, exercise and sexual activity. Nausea Early recognition of worsening symptoms When and where to seek help Explain self management of fluids Educate on the signs & symptoms or peripheral & central oedema Advise no more than 1 ½ -2 litres/day, depending on clinical signs & symptoms Consider increased dose of diuretics Provide patient / carer with contact numbers for both in office hours and out of hours Educate on daily weights including who to contact for advice if > 4Ibs over 2 days Self Management Diet- Discuss a balanced nutritional intake and explain rationale for the increased risk of malnutrition and cardiac cachexia Salt Consider referral for Cardiac/lifestyle rehabilitation. This may include exercise Consider referral to dietician for patients with cachexia / obesity Educate on reducing salt intake Caution on the use of ―Low Salt‖ and raise awareness on the salt in processed food. Advise on 2g sodium per day. Alcohol Educate on reducing alcohol intake Negotiate intake with individual if appropriate Smoking – Advise on benefits of stopping Medication – discuss reasons for medications and concordance issues is needed Psychological/ Social Needs Advise on avoiding aggravating medication, e.g. NSAIDs and rate increasing calcium channel blockers Advise on immunisation Psychological Needs Assess for symptoms of depression- as per NICE guidance (2009) Assess for symptoms of anxiety Advise on support groups- British Heart Foundation, Cardiomyopathy Association Carers Needs Encourage carer involvement including joint attendance at appointments Check their understanding of condition & care Next Review Home & social situation Assess environment and peer support mechanisms. Following initial assessment, frequency of review of Non pharmacological management is indicated by clinical need. Minimum review is annual Review Date June 2012 Consider referral to smoking cessation programme If symptoms of depression noted, advise patient to refer self to GP or refer to the local Mental Health team Advise on relaxation techniques Draw patient‘s attention to the contact details in the information booklet Consider referral to Social Services including OT assessment Consider benefits advice including attendance disability badge etc. 16 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Part Two Management of symptoms commonly experienced in advanced heart failure Indication for the development of this clinical guidance Heart Failure is very difficult to palliative effectively and there are many disease specific barriers to palliation. Many previously published guidelines for heart failure focus on active interventional aspects of management rather than palliation of the disease. I comparison with cancer patients, Heart Failure patients: Receive less information and support regarding their illness Have poorer understanding of the illness and it‘s prognosis Tend to be less involved in decision-making regarding treatment or non-treatment Do not perceive themselves as ‖dying‖ Experience frustrations with progressive loss (social and physical), complex medical regimes, social isolation and exclusion, poorly co-ordinated services and little palliation of symptoms Common Symptoms and Problems Experienced by Heart Failure Patients Breathlessness Cough Fatigue Peripheral Oedema Nausea and Vomiting Sleep Disturbance Pain Anorexia and weight loss Agitation and Delirium Increasing Dependence on others Psychological Concerns: Depression and Anxiety Constipation Itch Carer crisis These guidance aim to provide advice on the above. It is important to remember that many symptoms can be iatrogenic nature, some of these are listed also. 17 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 When does a Heart Failure Patient become “Palliative”? 1. You would not be surprised if this patient were to die in the next 6-12months based on your intuition which integrates co-morbidity, social and other factors. 2. Choice/ Need-patient makes a choice to have only comfort care and no curative therapy or is believed to need supportive/ palliative care 3. Clinical Indicators General Multiple co-morbidities Weight loss greater than 10% over 6 months General physical decline Serum albumin <25g/1 Reduced performance status Dependence in most activities of daily living At least 2 of the Indicators specific to Heart Failure New York Association Class III or IV despite optimal tolerated therapy Repeated episodes of symptomatic heart failure (this may be seen in terms of repeated hospital admissions or intensive community management) often with shorter periods of stability in between episodes. Difficult physical or psychological symptoms despite optimum tolerated therapy Deteriorating renal function Chronic Kidney Disease stage 4 or 5 Failure to respond within 2-3 days to changes I diuretic or vasodilating drugs Place patient on Palliative/ Supportive Care Register Issue green Card and Fax Out of Hours Handover sheet & complete DS1500 Ensure pre-emptive plan and drugs are organised if appropriate Days Consider place of care Continuing Care funding Liverpool Care Pathway Days to Weeks Consider place of care Continuing Care Funding Social care package, Community Nursing, Complex Case Manager, CHFMDT Weeks to Months Consider place of care Consider social care package, Community Nursing, Complex Case Manager support, Day Hospice, CHFMDT Consider Referral to Specialist Palliative CareTeam 18 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Issues for consideration when assessing patient‟s needs Diagnosis and prognosis should be discussed using the principles established as good practice for ―Breaking Bad News‖, bearing in mind that many heart failure patients and their families have little comprehension of the severity of their illness. Exploration of patient‘s expectations may be of benefit. Prognosis is particularly difficult to estimate in heart failure and underlying causes of deterioration in condition/ symptoms such as infection should be treated before considering prognosis in light of indicators. Preferred Priorities of Care should be discussed and documented The complexity of chronic heart failure necessities an individualised approach to the risks and benefits of various medical therapies. This is often a multidisciplinary process and should always include the patient. Medicines management should be an ongoing process ensuring optimal medical management suitable to stage of disease, e.g. withdrawal of satin therapy in last weeks of life. Discussion of resuscitation status should be undertaken and documented in patient‘s records and where appropriate communicated to healthcare professionals and ambulance service. This is a pertinent issue for people with heart failure as their risk of sudden cardiac death (SCD) is 50% higher than in the general population. SCD is also more prevalent in class I & ii heart failure patients. Following the issue if NICE guidance there are now increasing numbers of people who will be fitted with an implantable cardioverter defibrillators (ICD). If someone had an ICD, there will need to be an open and honest discussion about when and how the defibrillator should be deactivated. Guidance on Page 38 provides further guidance Patients should be asked if they have an Advance Decision to Refuse Treatment (ADRT) of have considered having one- bear in mind new guidance on advanced decisions and mental capacity act. A Management Plan should be drawn up with the patient and with a written record provided. This should be communicated to other healthcare professionals as appropriate. Anticipatory prescribing and planning should be a priority and where appropriate patients should be supplied with a pack of anticipatory medications and local contact numbers, to avoid problems at nights, weekends and public holidays. The issue of a green card and faxing of a handover sheet will allow out of hours and emergency services staff to provide care more appropriately. Provision of supportive printed information should be given where available and appropriate e.g. End of Life Booklet (Marie Curie & Cancer Bacup) which is aimed at all conditions not just cancer. Consideration needs to be given to carer support and referrals to appropriate agencies made. Follow up arrangements should be discussed and the patients should have clear understanding of what is likely to happen next. 19 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Place Patient on Palliative and Supportive Care Register (GSF) Days Days to Weeks Weeks to Months Preferred priorities of Preferred Priorities of Identify preferred care Care priorities of care and social care package OOH Green Card Funding of Care Care Package Continuing Care Funding DS1500 Benefit OOH Green Card Care Package Consider referral to: Support Group Welfare Advice Community Nursing Therapists Day Hospice for Palliative Rehabilitation Advanced CHF MDT Specialist Palliative Care Carer Support Group Community Nursing Support Liverpool Care Pathway Advanced CHFMDT Specialist Palliative Care OOH Green Card Carer Support Group Months to Years Social Care OOH Blue Card Consider referral to: Support Group Benefits Advice Community Nurses Therapists Cardio respiratory Rehabilitation Day Hospice for Palliative Rehabilitation Advanced CHF MDT Carer Support Group 20 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Suspected Acute Confusion / Delirium Onset typically hours to days and Non- Pharmacological Management clinical features, from which underlying cause may be elicited. Listen to patient and try to explore their fears and Common Clinical Features anxieties. These can manifest themselves in hallucinations and nightmares Restlessness, anxiety, sleep disturbance, irritability, emotional lability, anger, sadness, euphoria Disorientation Memory Impairment Disorganised thought processes, altered perception, illusions hallucinations, delusions Incoherent speech Attention span reduced, easily distracted Motor abnormalities such as tremor, altered tone and reflexes Remain calm and avoid confronting the patient Try to keep patient in as normal and familiar a routine and place as is possible. Explore perceptions and validate those that are accurate Explain clearly what is happening and why to patient and carer(s) Try to provide an action plan for what can be done Explain management plan and repeat information to assist retention by patient and family If medication is required ensure the length of treatment course is discussed and stress that delirium is not mental illness but a state in which periods of lucidity can be expected. Do not use restraints and allow to mobilise if safe to Treat Underlying Causes Infection Hypoxia Renal Impairment Hepatic Impairment/congestion Drug toxicity-beta blockers, digoxin, anti-cholinergics Drug withdrawal-opiods, alcohol, Pharmacological Management Benzodiazepines should not be used alone as they can worsen delirium (unless associated with alcohol withdrawal) Consider: 1. Haloperidol either PO,SC (low dose in elderly but can be increased if poor response) 2. Haloperidol + Benzodiazepine e.g. diazepam or midazolam 3. If severe Midazolam and levompromazine combined may be necessary to provide sedation 4. Consider use of a syringe driver benzodiazepines, SSRIs, nicotine Unrelieved pain Constipation, urinary retention If No Improvement after exclusion of underlying causes or it is inappropriate to treat: Consider whether this is Terminal Restlessness, which is a feature of dying. If dying is diagnosed follow Liverpool Care Pathway 21 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Breathlessness Assessment Non pharmacological Management Do not Assume due to CHF as Consider teaching breathing techniques –refer to breathlessness is usually multi-factorial Assess when they feel breathlessness is physiotherapist or occupational therapist Use a fan to improve airflow around face a problem How much of the day, including investigating its affect on sleep Assess effect on functional abilities and activity Pace activities and plan recovery time Consider referral to cardiopulmonary Rehabilitation or physiotherapy activity programme Consider referral to Palliative Rehabilitation Group What makes it better or worse Consider referral to Hospice Day Care Explore Fears Consider use of complementary therapies Associated symptoms Pharmacological Management Identify and Treat Underlying Causes Consider: Anaemia- common in people with kidney impairment as blood cells are damaged and can‘t carry as much oxygen Infections or respiratory disease Concommitant Problems e.g. COPD, renal impairment Saline nebuliser prn Low dose opiates, e.g. codeine phosphate 30mg 4 hourly, low dose oramorph or MST Consider laxatives if commenced on opiates Lorazepam 0.5-1mg chewed or sublingually prn Oxygen Short of breath on exertion (SOBOE) Medication e.g. betablockers Consider Poor symptom control- e.g. Nebuliser Oxygen Diuretics breathlessness, pain, leg swelling Psychological and spiritual issues – e.g. frustration, stress and low mood, anxiety / concerns about what the future holds. Is disease management optimal? Short of breath anxiety related or at rest (SOBAR) Consider Oxygen Opiate Nebuliser Benzodiazepine Terminal SOB Consider Opiate Midazolam levomepromazine If blood oxygen saturation impaired consider Long Term Oxygen Therapy Assessment, see appendix for guidelines Review Date June 2012 22 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of constipation Assessment Non-Pharmacologist Management Assess using Lincolnshire PCT bowel health assessment form Encourage adequate diet and fluid intake Establish dietary and fluid intake Stay as active as possible Consider the use of prune juice Provide information on best position to sit in to pass stool Record stool chart Encourage to sit on the toilet 20 minutes after meals to Review medication list take advantage of the gastro colic reflex Consider referral to the Community Nursing Team or Explore attitudes and current functional capacity e.g. has mobility recently reduced? Specialist Continence Clinical Nurse Specialist Consider DRE (digital rectal examination) if competent Pharmacological Management Identify and treat causative factors Consider use of magrocols e.g. movicol Inadequate dietary intake Consider stool softener e.g. lactulose, sodium docusate Dehydration from diuretics or not drinking enough Immobility Medications such as opoids or iron supplements Consider stimulant, e.g. senna, glycerine, suppositories, microlax enema, bisacodyl. Consider combination agent e.g. co-danthramer Consider sodium docusate enema Consider referral to the Community Nursing Team or Specialist Continence Clinical Nurse Specialist If opioid-induced constipation, follow: Mid-Trent Cancer Network Symptom Control Guidelines accessed at: http:// www.information4u.org.uk/files/midtrentsymptomcontrolguidlinesfinal 170506.pdf 23 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Cough Assessment Frequency Non-Pharmacological management Consider teaching breathing techniques-refer to physiotherapist or occupational therapist Use a fan to improve airflow around face Sputum Aggravating factors Relieving Factors Identify and Treat Underlying Causes Consider Infections Concomitant Problems e.g. Respiratory Conditions Medication e.g. ACE Inhibitors Is disease management optimal? Pharmacological Management Optimise Heart Failure Management whilst trying to minimise side effects of drugs. Simple linctus or codeine linctus prn Low dose Oramorph, e.g. 2mg prn. Consider prophylactic laxatives if commenced on opiate Saline nebuliser of thick secretions Consider whether related to ACE I or other therapy Consider mucolytics / glcopyrronium 24 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Fatigue Assessment Assess when they feel fatigued, how much of the day, including investigating sleep patterns both at night and day Assess functional abilities and activity patterns e.g. if able to wash and dress, how long it takes, how they feel afterwards etc. Non-Pharmacological management of Fatigue Encourage the patient to: Eat small regular meals Exercise regularly (even a very small amount) Plan activities, but plan to do what they can definitely achieve, nothing what they completed and what they had to stop before finishing Plan to rest after each activity and after meals for a short time Keep a diary and note when the best and worst parts of the day are, then use the best times to undertake activities Plan to do less on days when you will be tired, e.g. plan less Identify and Treat Underlying Causes on the day of a hospital appointment and the day after as energy will be needed to get there and to recover afterwards Consider: Anaemia- common in people with kidney impairment as blood cells are damaged and can‘t carry as much oxygen Consider referral to cardiopulmonary Rehabilitation, Physiotherapy activity programme or palliative rehabilitation Make adaptations to home to aid energy conservation Infections Energy conservation advice sheet Concomitant Problems e.g. diabetes, renal impairment, thyroid dysfunction Review Home Care package Medication e.g. betablockers, opiates, digoxin, psychotropics. Eating problems - loss of appetite, nausea, altered taste may reduce the amount and variety of foods eaten. Less calories = less energy available Poor symptom control- e.g. breathlessness, pain, leg swelling Psychological and spiritual issues – e.g. frustration, stress and low mood, anxiety / concerns about what the future holds. Consider referral to support Group or Expert Patient Programme Pharmacological Management Treat Underlying Causes Optimise Heart Failure Management whilst trying to minimise side effects of drugs AVOID APPETITE STIMULANTS (Dexamethasone, progestogens, amphetamines) Tricyclic Antidepressants 25 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Itching Assessment General Management Where is the itching? When does it itch? What makes it worse? How long does it last? What is the impact on life/ functional abilities / Sleep? What is the condition of the skin like? Treat Underlying Causes Dry Skin Wet Skin including sweating Renal Impairment Liver function impairment Thyroid Dysfunction Iron Deficiency Drug induced – opioids, aspirin, hormonal treatments Note: Many of these causes are not histamine related and are more likely to be a central effect of the underlying abuse. i.e. they may not respond to anti-histamines Wear Cotton Clothing Discourage scratching Avoid Hot Baths Avoid Soap and Bubble Bath Avoid Overheating Avoid Sweating Loose bedding Consider use of fan to aid cooling Management of Specific Underlying Causes Dry skin Avoid soap Use emulsifying ointment or baby soap Consider using Cetraben or Diprobase creams as soap substitutes. Apply emollients esp. after washing (note sometimes using greasier preparation such as Epaderm at night and something less greasy e.g. Cetraben in the day works well) Note bath emollients are wasteful and costly Wet skin (incontinence, sweating) Use barrier cream e.g. Cavilon Consider the use of appropriate fitting incontinence wear , and only when indicated the assessment for a catheter or sheath drainage. Protect skin from stool leakage (absorbent pads and barrier cream/ manage constipation or diarrhoea effectively) NOTE Co-danthramer can cause unpleasant rash on buttocks or thighs. Consider treatable causes of sweating – e.g. infection, hormonal, drug-induced. Cancer related. Consider using paracetamol for fever Renal and Liver Impairment General measures + antihistamine trial Ondansetron 4mg bd orally (unlicensed use) Consider levomepromazine 3—6mg orally if resistant Consider dexamethasone if severe Opioid Induced General Measures + try alternative opioid 26 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Special Issues for Consideration when Managing Pain in Heart Failure Types of Pain o o o Adequate pain assessment is vital Attempt to define the origin(s) of the patient‘s pain Major types of pain are: musculo-sketal, somatic,neurpathis, spasmodic, pain of a psychical nature (also referred to as spiritual pain). Not all pains are opiate responsive o o o Somatic pain is usually very responsive to opiates Some musculo-skeletal and neuropathic pains may respond partially to opiates but may require the addition of adjuvant analgesics See Mid-Trent Cancer Network Guidelines for further advice Remember the Analgesics Ladder o o Problems associated with opiate toxicity can be avoided by following the steps outlined in the ladder. Always Start Low with opiate Doses and Go Slow when increasing Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) – Risks/ Benefits o o In some circumstances the risk of increased oedema and/or worsening renal function associated with the use of NSAIDs can be outweighed by the benefit to the patient in terms of pain relief In the management of Acute Gout, a short course of NSAIDs can be well tolerated. Colchicine is a useful alternative and Allopurinol should be considered for prevention after a second episode of acute gout has been treated.(N.B. In patients with renal dysfunction a reduction in standard dose is appropriate) See full guideline at www.rheumatology.oxfordjournals.org Trans-dermal Analgesics o o Buprenorphine and Fentanyl Patches are being increasingly used in the management or non-malignant chronic pain. They are designed to be used for stable opiate sensitive pain and should not be used for acute pain relief or where titration of analgesia is required. Their use in the terminal, end of life situation is problematic for many reasons and their substitution/replacement with an alternative form of opiate should be considered. The use of a syringe driver should be considered in these situations Routes of Administration o o In the presence of extensive peripheral and visceral oedema, the absorption of oral medication may be erratic, unpredictable. Consider other routes of administration sub-lingual, trans-dermal (avoid placing patches on oedematous areas), sub-cutaneous. 27 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Nausea and Vomiting Assessment Assess symptom-nausea and or vomiting If vomiting, what is being produced? When are symptoms present Any precipitating factors e.g. eating food Any relieving factors Consider asking patient to keep a symptom diary Review after treating Non-Pharmacological Management Consider psychological and spiritual care to treat anxiety Consider relaxation therapy, refer to physiotherapist/Occupational Therapist Consider Complementary therapy, suggest self referral to private provider or hospice Pharmacological Management Avoid cyclizine (increase heart rate and decreases cardiac output) Consider causative factors and correct where possible Drugs e.g. morphine or antimuscarinics Renal or liver dysfunction Gastric stasis caused by enlarged liver, constipation or gastric outflow obstruction Oedema Constipation Anxiety Pain Infection Cough Review medication and identify risk/ benefit of any drugs believed to cause nausea or vomiting and discontinue therapy if appropriate. For chemical causes e.g. morphine, renal failure - Consider Haloperidol or Metoclopramide. Consider Metoclopramide or Domperidone if: - Related to meals - Vomiting undigested food - Hepatomegaly If nausea is constant or there is renal impairment/failure - Consider Haloperidol at night - Levomepromazine which has a sedative effect but may cause postural hypotension. Use in low doses (3-6mg) and cautiously with elderly people 28 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of peripheral oedema Non-Pharmacological Management Assessment Rest Assess Tissue Viability Colour Texture Temperature Restrict fluid intake Record daily weights is able to Review home support and arrange additional Sit with feet up and legs well supported when possible care as required Assess oedema including whether: Bilateral Height up leg Abdominal distension Sacral oedema Pitting Identify and treat if appropriate any alternative underlying causes such as: Renal failure Dependant oedema Infection Deep vein thrombosis Liver dysfunction Pharmacological Management First line is loop diuretic If persistent oedema addition of an aldosterone antagonist should be considered. Resistant oedema may require the addition of a thiazide diuretic periodically and referral for specialist advice should be sought as careful monitoring of clinical status, renal and liver function is required in this group of patients 29 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Poor Appetite and Weight Loss/ Cachexia Assessment Use Malnutrition Universal screening Tool and LPCT guidelines for management Non- Pharmacological Management As desired diet Establish daily dietary and fluid intake Advise small meals often Consider a small amount of alcohol before meals Suggest high calorie, high protein, no added salt diet- see local guidelines for details Encourage good oral hygiene Consider alternative flavouring for foods Refer to dietician Consider referral to Palliative rehabilitation Establish likes and dislikes Explore expectations Consider environmental factors Are there any problems with eating, swallowing? Consider examining mouth Identify and treat causative factors Drug toxicity e.g. Digoxin Renal or liver dysfunction Oedema Constipation Anxiety Dry or sore mouth Pharmacological Management Avoid appetite stimulants – (Dexamethasone progestogens, amphetamines) Supplement drinks or dietary fortifications may be prescribed (use LPCT guidelines to aid prescribing) Ill fitting dentures or no teeth Consider discontinuing statin Unable to prepare food Consider whether related to medication Overdiuresis 30 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Psychological Concerns Non- pharmacological Advice Assessment Assess mood for signs of Anxiety Depression- as per NICE guidline (2009) Discuss expectations Identify hopes and fears Explore beliefs and wishes Use MDT to address issues using therapies, where available such as: Relaxation Counselling Imaging techniques Complementary therapies Spiritual support Chaplaincy support Palliative Rehabilitation Support groups Carer support Cognitive Behavioural therapy Psychology Mental health referral/ crisis team if stating suicidal intent Identify and Treat Underlying Causes of Anxiety and Depression Consider: Poor symptom control- e.g. breathlessness, pain, leg swelling Pharmacological Management Avoid tricyclics as cardio-toxic AVOID St John‟s Wort Psychological and spiritual issues- e.g. frustration, stress, and low mood, anxiety/ concerns about what the future holds. Antidepressant, e.g. sertraline is first-line Sleep disturbance and insomnia Nausea and Poor appetite consider Fatigue Poor Appetite treatment Anxiety depression, e.g. citalopram antidepressant e.g. mirtazepine Night sedation, e.g. Ziplicone, lorazepam, lormetazepam, lorazepam Anxiolytics e.g. lorazepam sub lingual or chewed especially for panic attacks Anxiety, e.g. diazepam is first-line treatment (buspirone is second line treatment) 31 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Sleep Disturbance and Insomnia Non-pharmacological management of Insomnia Assessment Assess including investigating sleep patterns both at night and day, e.g. What time did you go to bed? What did you do beforehand, e.g. activities, food and drink taken? Encourage the patient: To establish a bedtime routine, e.g. having a warm drink but avoiding caffeine/alcohol from mid afternoon and/ or a snack before bed To make the bedroom quiet and the right temperature If they are lying awake not able to sleep, to get up and do something then come back to bed To try to relaxation techniques or mental exercises To set the alarm and try to get up at the same time every morning To avoid napping late afternoon Follow advice given in Sleeping Well Leaflet available at www.rcpsych.ac.uk Did you get off to sleep right way? When did you wake in the night? How often did you wake in the night? Any other symptoms associated with being awake? What naps in the day did you have? (Time, place and length) Is snoring a problem? Any episodes or witnessed apnoea? Treat Underlying Causes Poor symptom control- e.g. breathlessness, pain, leg swelling Psychological and spiritual issues- e.g. frustration, stress and low mood, anxiety/ concerns about what the future holds. Sleep Apnoea- see NICE Guidance Pharmacological Management AVOID tricyclics as cardio-toxic Night sedation, e.g. zopiclone, lorazepam, lormetazepam,lorazepam,temazepam. Antidepressant, e.g. sertaline is first-line treatment Anxiety depression, e.g. citalopram Anxiolytics, e.g. lorazepam sub lingual or chewed especially for panic attacks Anxiety, e.g. diazepam is first-line treatment (buspirone is second line treatment) 32 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Stomatitis / Sore Mouth Non-Pharmacological Management Assessment Undertake assessment in good light and note the colour, moisture, texture of the mucosa. Note any plaques, lesions, discolouration or injury seen. Note if dentures or dental prosthesis worn Ask when last reviewed by dentist Review medication Review dietary and fluid intake Teach good mouth and lip care regime Rinse with water regularly Try sucking ice cubes, lollies or ice chips Try chewing gum Rinse mouth with pineapple juice Promote a healthy diet General Pharmacological Management Use paraffin gel on lips if not using oxygen If using Oxygen consider humidifying it Infection (bacterial or viral) Consider use of antibacterial mouth wash Oxygen Use via Nasal Cannula Oral balance products/artificial saliva Ulceration Consider dietary supplements/fortification of food if nutritional intake is poor Treat Underlying Causes Ill-fitting dental prosthesis Thrush Herpes Simplex Poor blood glucose control Heart failure causes dry mouth and thirst Drug Side Effects Examples include: Nicorandil which is associated with mouth ulceration in some people Steroid Inhalers and long term omeprazole use which can be cause thrush Specific Pharmacological Management Thrush Consider nystatin suspension or lozenges If persistent, oral fluconazole may be usedsee BNF for prescribing information Herpes Simplex Consider acyclovir preparations Mouth Ulceration Consider Difflam Mouthwash or Orabase gel 33 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Medicines Management in Advanced Heart Failure Review Medications at each visit Consider discussing with GP, Pharmacist or at Multidisciplinary Team Meeting Consider stopping medications that derive no short term benefits such as statins. Maintain ACE Inhibition, Betablocker, Aldosterone Antagonist and Digoxin if possible as these all aid heart function and symptom control Diuretics are used only for symptom control and should be reviewed in light of signs and symptoms see Weigh up risks/benefits of therapies Use therapy guidelines where available to aid a systematic approach to care Consider best route for administration of essential medicines The use of drugs outside their license is more common in palliative care and there are some clearly identified instances in these guidelines. Clinicians should seek further advice from pharmacist or specialist palliative care team before prescribing if they are unfamiliar with the use of that particular drug in these circumstances. 34 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Management of Anaemia Anaemia is a common problem in heart failure and should be investigated to enable the treatment of the underlying cause Hb < 11g/dl? Assess Renal function and Haematinic‘s Non renal causes and Haematinic deficiency excluded? See NICE clinical guideline 39 for further guidance on Anaemia Management in people with chronic kidney disease if GFR < 60 ml/min. http://guidance .nice.org.uk/cg39 Management of Gout Gout is common in heart failure due to the use of diuretics. The use of NSAID‘s or Corticosteroids is to be avoided in the management of acute gout in heart failure. The preferred drug treatment is Colchicine with a view to commencinglow dose Allopunnol once the acute attack has been treated Please see http://www.rheumatology.oxfordjournals.org for further guidance. 35 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Pathway for Advance Care Planning in patients with Chronic Heart Failure Patients condition prompts discussion regarding preferred priorities of Care/goals of care Provide documentation on Preferred Priorities of Care/Information Record Discuss the patient‘s goals of care/preferred priorities of care and treatment plan If the patient wishes to, discuss to refuse Treatment/resuscitation status Provide patient information regarding ADRT including frequently asked questions for the patient to discuss with family/significant others Explain ADRT-the circumstances that it would be followed as per the ADRT documentation If the patients wishes to complete an ADRT they complete themselves/with assistance if required Document mental capacity in patients notes Once ADRT completed: Fax to all health care professionals involved with a covering letter (GP/CM/OOH/Hospice) If the patient has decided not for resuscitation complete EMAS registration form and fax with a copy of the ADRT Return the original documents to the patient Review the patient‘s wishes at regular intervals 36 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Iatrogenic Problems Iatrogenic Problems Overdiuresis Symptoms Hypokalaemia Hypotension Falls Nausea Loss of appetite Confusion Nausea Loss of appetite Diarrhoea Abdominal Pain Confusion Bradycardia/ Heart Block Hypotension Loss of awareness of impending hypoglycaemia Confusion Constipation Dry Mouth Nausea Muscle Spasm (Myoclonus) Can precipitate deterioration in heart failure, renal function and blood glucose control. Digoxin Toxicity Opiates Steroids Drugs to Avoid In Heart Failure Cyclizine NSAIDS Steroids Calcium Channel Blockers Glitazones Amphetamines Progestagens Tricyclic Antidepressants St Johns Wort 37 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Pathway for Deactivation of Implantable Cardioverter Defibrillators at End of Life Indications for consideration of deactivation of ICD Patient preference in advanced disease In the event that the patient has completed an Advanced Decision to Refuse Treatment Approaching end of life when activation would be inappropriate Following withdrawal of anti-arrhythmic drug therapy as per medicines review at end of life While an active DNR order is in force Process prior to deactivation Open discussion with the patient, next of kin/carer or patient advocate as part of advance care planning please see guidance on page 32 Multidisciplinary review including cardiologist where appropriate Points of discussion may include: Resuscitation status and possible completion of an ADRT Withdrawal will not result in immediate death but the safety not provided by the device will no longer apply Deactivation is achieved using an external programmer and is not painful Multi-organ failure associated with electrolyte disturbance may be proarrhythmic and result in device discharge Inappropriate shocks are uncomfortable and inconsistent with symptomatic care Some ICDs incorporate both defibrillation and pacing modalities and it may be appropriate to selectively disable the defibrillation element as untreated bradycardias may exacerbate patient symptoms. Procedure for deactivation: The patient should complete the locally agreed deactivation consent formappendix Liaise with local senior cardiac physiologist to arrange a mutually convenient time and appropriate place identified for deactivation Deactivation of ICD by cardiac physiologist NB, After death, ICD generators may need to be explanted if cremation is being considered Further guidance available at www.arrhythmiaaliance.org.uk Or www.bhf.org.uk 38 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Useful Weblinks/ contacts Organisation American Heart Association British Cardiovascular Society British Heart Foundation Cardiomyopathy Association European Society for Cardiology Mid- Trent Cancer Network National heart and lung library National Specialist Library for cardiovascular diseases Palliativedrugs.com Prodigy Prescribing Information Royal College Psychiatrists Patient Information Sites Contact Information www.americanheart.org www.bcs.com www.bhf.org.uk Tel: 0845 70 80 70 www.cardiomyopathy.org www.escardio.org www.mtcn.nhs.uk email: [email protected] Tel: 0115 9627988 www.nhlbi.nih.gov www.libary.nhs.uk/cardiovascular www.palliativedrugs.com www.prodigy.nhs.uk www.rcpsych.ac.uk www.CHFpatients.com www.heart-transplant.uk www.patient.co.uk Local Support Group -HOPE www.heartfailurematters.org www.arrhythmiaaliance.org.uk www.hopelinks.org.uk Advance Decision to Refuse Treatment www.adrtnhs.co.uk Other Useful Information Trent midcancer network symptom control guidelines hold valuable advice on the following: Opiate Conversion Charts Opioids for breathlessness Opioid-induced constipation Acute inflammatory episodes in Lymphoedema Depression Dry skin in lymphoedema Pain Relief 39 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 References Arrhythmia Alliance (2007) Implantable Cardioverter Defibrillators (ICD‘S) in Dying Patients Baines, M. (1997) The emetic process-,pathways or emesis and the neurotransmitters involved. BMJ Vol 315 pp. 1148-1150 Beattie J (2007) ‗End of life Issues and Cardiac Device therapy‘ www.heart.nhs.uk British Medical Association and royal Pharmaceutical Society of Great Britain (2006) British National Formulary No 51. London. BMJ Publishing Group Ltd and RPS Publishing Buckman, R.A.(2005) Breaking bad news; the S-P-I-K-E-S strategy. Community Oncology Vol.2 pp 138-142 Ellershaw J.E Wilkinson S. (2003) Care of the dying: a pathway to excellence. Oxford University Press. Gibbs, L.M.E., Addington-Hall, J, Simon, J, Gibbs, R. (1998) Dying from Heart failure: lessons from palliative care: Many patients would benefit from palliative care at end of their lives. British Medical Journal. Vol 317 No 7164 pp 961-2 Johnson, M.J (2006) A palliative care approach for patients with heart failure. Palliative Medicine Vol.20 pp 182-185 Johnson M.J., Houghton,T. (2006) Palliative care for patients with heart failure: description of a service. Palliative Medicine Vol.20 pp 211-214 Jordon, K.M., Cameron, J.S. Smith, M.,Zhang, W., Doherty, M., Seckl, J., Hingorani, A., Jacques, R., Nuki, G on behalf of the British Society for Rheumatology and British HealthProfessionals in Rheumatology Standards, Guidelines and Audit Working Group (SGAWG) (2007) British Society for Rheumatology and British Health Professionals in Rheumatology Guideline for the management of Gout, Accessed online at http://rheumatology.oxfordjournals.org/cgi/content/full/kem05av1 on the 13th July 2007Lincoln. Jordhoy, M.S., Grande, G. (2006) Living alone and dying at home: a realistic alternative? European Journal of Palliative Care. Vol 30 pp 325-8 Mid-Trent Cancer Network Publications (2006) consulted: Guidelines for communicating Bad News with Patients and their Families, 2006. Symptom Control Guidelines, 2006 Palliative Care Pocket Book (2nd Ed) 2006 Available via www.mtcn.nhs.uk 40 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 National Institute for Clinical Excellence Clinical Guidline 5 Chronic heart failure: Management of chronic heart failure in adults in primary and secondary care. London. National Institute for Clinical Excellence 2003 Sica, D.A (2003) Drug absorption and the management of Conjestive Heart Failure: Loop Diuretics. CHF Volume 9 No.5 pp 287-292 Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ (2001) More ‗malignant than cancer? Five-year survival following a first admission for heart failure. European Journal of Heart Failure Vol 3. pp 315-22 SymptomControl.com(2006) Symptom Control info. (online) www.SymptomControl.com/1430.html Accessed at Lincoln on 5th January 2007 Tan, L/B.,Bryant, S. Murray, R.G, (1988) Detrimental haemodynamic effects of cyclizine in heart failure. The Lancet Vol 8585 pp 560-1 Tsuyuki, R.T.,Mckelvie, R.S, Malcolm,J.,Arnold,O.,Avezum A.Jr.,Barretto,A.C.P., Carvalho,A.C.C, Isaac,D.L, Kitching,A.D.,Piegas, L.S., Teo,K.T., Yusuf,S. (2001) Acute Precipitants of Congestive Heart Failure Exacerbations Archives of Internal Medicine. Vol. 161:2337-2342 Twycross R, Wilcock A (2001) Symptom Management in Advanced Cancer (3rd Edition) Radcliffe Medical Press Ltd, Oxon Twycross R, Wilcock A, Charlesworth S and Dickman A (2002) Palliative Care Formulary (2nd Edition), Radcliffe Medical Press Ltd,Oxon. See also www.palliativedrugs.com. Verma, AK., Da Silva, J.H., Kuhl, D.r. (2004) Diuretic Effects of Subcutaneous Furosemide on Healthy Volunteers: A Randomized Pilot Study. The Annals of Pharmacology. Vol.38 No.4 pp 544-549 Zambroski, C.H (2006) Managing beyind an uncertain illness trajectory:palliative care in advanced heart failure. International Journal of Palliative Nursing. Vol 12 No.12 pp.566-573 British Heart Foundation (2007) Implantable cardioverter defibrillators in patients who are reaching end of life, London BHF Advance Care Planning: a guide for health and social care staff (2008) available: www.endoflifecareforadults.nhs.uk 41 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Coronary Heart Disease Collaborative (2004) Supportive and Palliative Care for Advanced Heart Failure. Available at www.heart.nhs.uk Department for Constitutional Affairs (2007) Mental Capacity Act 2005. Code of Practice, London JSO Department of Health (2008) End of life Care strategy London DOH National Council for Palliative Care (2008). Advance Decisions to refuse treatment, a guide for the Health and Social Care Professionals. London DOH Prognostic Indicator Guidance Gold Standards Framework, Available at: www.goldstandardsframework.nhs.uk ICD TA95 and CRT TAI20 guidance available at www.nice.org.uk 42 Review Date June 2012 Clinical guidance for the management of patients with confirmed Heart Failure in primary care in Lincolnshire- June 2010 Audit/ Monitoring of policy Implementation The implementation of the policy will be audited by the service managers through the Audit Tool attached at Appendix E of the ―Guidance on Policy Development‖ available on the trust website Audit is also undertaken via the Gold Standards Framework which will provide information regarding heart failure patients on this register Implementation Strategy The corporate Directorate will ensure that the guideline after approval is put on the trust website for dissemination and sent out in staff newsletter issued by the communications department via Postmaster. Additionally, the individual teams will also be informed by their team leaders about the policy. Training will be offered through the Trust‘s Chronic Heart Failure Study Days, Palliative Care Education Forum and on request. 43 Review Date June 2012