* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Soft Tissue Infections: Abscesses, Cellulitis and Necrotizing Fasciitis
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Oesophagostomum wikipedia , lookup
Anaerobic infection wikipedia , lookup
Antibiotics wikipedia , lookup
Melioidosis wikipedia , lookup
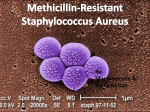
Staphylococcus aureus wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Abscess Management in a Post CA-MRSA era Erin Marra MD Simran Vahali MD 2016 Abscess Management What are current guidelines in abscess management? Do we I&D all abscesses or can we use needle aspiration? Do we need to pack all abscesses we drain? Who needs antibiotic treatment? Is management different in pediatric cases? NEJM, 2006 Prospective prevalence study N = 422 Patients with acute, purulent skin and soft tissue infections 11 university affiliated EDs in August 2004 Cultures obtained on all patients S. aureus isolated from 320/422 pts (76%) MRSA prevalence 59% (rest was MSSA) Among the MRSA isolates 95% susceptible to clindamycin 6% susceptible to erythromycin 60% susceptible to fluoroquinolones 100% susceptible to rifampin and bactrim 92% susceptible to tetracycline Follow up by phone 2-3 weeks after enrollment Antibiotics discordant in 100/175 patients MRSA most common cause of abscesses presenting to the ED Empiric antibiotics prescribed in the ED should cover MRSA in patients with cutaneous abscesses MRSA IN INDIA? Methicillin resistant staphylococcus aureus (MRSA) in India: Prevalence & susceptibility pattern Indian J Med Res. 2013 Feb; 137(2): 363-369 • Studied 15 Indian tertiary care centers during 2008-2009 • 26,310 isolates obtained • Overall prevalence of MRSA= 41% • 2009: 47% ICU; 49% ward; 27% community • Mrjority of isolates from skin and soft tissue infections> respiratory and blood infections • Low susceptibility of MRSA to ciprofloxacin (21%) Treatment options for MRSA Recommendations from authors Culture your wounds Vancomycin and Linezolid for MRSA De-escalate once culture sensitivities are returned 201 staph isolates detected as MRSA out of 500 staph samples (40.2%) 143 were HA-MRSA (71.1%) 58 were CA-MRSA (28.8%) Suggestions by authors Ca-MRSA Had “relatively” low resistance patterns for clindamycin (21%), bactrim (22%), gentamicin (17%), tetracycline (14%), chloramphenicol (7%) and amikacin (6%), nitrofurantoin (0%) Ha-MRSA- use linezolid and Vancomycin Journal of Emergency Medicine, 2011 Literature review MRSA - no reliable historical, physical or epidemiological risk factors Wound cultures - not necessary in uncomplicated abscesses Antibiotics - do not aid in healing but may decrease rates of formation of new lesions Incision and drainage - primary treatment of superficial abscesses Packing - small pilot studies show similar outcomes in packed and un-packed abscesses Wound Care Follow-up - 48 hour check Abscess Incision and Drainage If I&D is considered primary treatment of abscesses, what is role of needle aspiration? What to do when you hear - “Just go stick a needle in it.” Annals of Emergency Medicine, 2011 Nonblinded randomized control trial Pts with uncomplicated superficial abscesses N = 101; I&D group (54) vs. ultrasound guided needle aspiration (47) Post procedure sono done for resolution Pts had f/u at 48 hours and on day 7 Goal was sonographic resolution at day 2 and clinical resolution at day 7 60% needle aspirations yield little/no purulence despite evidence of pocket on sono Overall success needle aspiration 26% and I&D 80% Difference was 54% (95% CI 35-69%) Both less successful with MRSA Needle aspiration is insufficient therapy for skin abscesses To Pack or not to Pack Has packing drained abscesses been shown to be of any benefit? Academy of Emergency Medicine, 2009 Prospective randomized single-blinded trial Determine if packing of simple abscesses after I&D has benefit over I&D alone N = 48 Patients recorded pain scores BID Follow up at 48 hours No significant differences in need for second intervention at 48 hour f/u Packed group = greater pain scores immediately post procedure (p = 0.014) and at 48 hours (p = 0.03) Packed = 23 - 4 required intervention Nonpacked = 25 - 5 required intervention p = 0.72; 95% CI 0.4-4.2 Greater use of ibuprofen (p = 0.12) and percocet (p = 0.03) Not packing simple abscesses does not result in increased morbidity Antibiotics Are they indicated after I&D? When should we be prescribing them? Annals of Emergency Medicine, 2007 Systematic Review Article N = 6 RCTs, Prospective and Retrospective Cohort Studies Pts with I&D alone have same rates of resolution as I&D + antibiotics Both groups show > 90% full resolution Current literature doesn’t support practice of prescribing antibiotics after I&D of simple abscess Annals of Emergency Medicine, 2010 Multicenter, double-blind, randomized placebocontrolled trial N = 190 Included pts > 16yr with uncomplicated abscess In adults with soft tissue infection: Does bactrim reduce rate of tx failure by 15% relative to placebo at 7 days after I&D? What is the rate of new lesion formation within 30 days? All abscesses drained, packed, and had wound cultures sent Physicians and pts blinded Pts returned at 2 and 7 days for re-eval 30 day f/u conducted over the phone Rate of MRSA 53% Pediatrics What are recommendations for abscess management among the pediatric population? Annals of Emergency Medicine, 2010 Double-blind, Randomized Controlled Trial N = 161 Randomized to 10 days of bactrim or placebo after I&D Follow-up Visit or call at 10-14 days Call at 90 days Primary outcome = treatment failure at 10d Secondary outcome = new lesion at 10d or 90d follow-ups Non-inferiority of placebo compared to bactrim for primary and secondary outcomes Failure rates 5.3% in placebo group 4.1% in antibiotic group Noninferiority established (equivalence threshold of 7%) New lesions at 10d and 90d follow-up 19 at 10d and 15 at 90d on placebo 9 at 10d and 13 at 90d on antibiotics Statistically significant difference at 10d, not at 90d Conclusion that antibiotics not required for pediatric skin abscess resolution but may help prevent new lesions in the short term Pediatric Infectious Disease, 2004 Prospective Observational Study Determine if I&D alone is sufficient for management of CA-MRSA abscess N = 69 Initial visit and two follow up visits Overall ID Guidelines What does Infectious Disease recommend for MRSA management? Clinical Infectious Diseases, 2011 Management of SSTI in era of CA-MRSA Cutaneous abscess I&D is primary treatment For simple abscess I&D is likely adequate Culture if use antibiotics, severe local infection, signs of systemic infection, no response to initial treatment Antibiotics recommended for abscesses with: Recurrent or persistent abscesses Associated comorbidities or immunosuppression Severe or extensive disease Rapid progression in presence of associated cellulitis Signs/symptoms of systemic illness Extremes of age Abscess in area difficult to drain (face, hand, genitalia) Associated septic phlebitis Lack of response to I&D alone Empirical coverage of CA-MRSA in outpatients with SSTI Empirical coverage for b-hemolytic strep AND CA-MRSA Clindamycin, bactrim, tetracycline (doxy or minocycline), linezolid Clindamycin, bactrim, tetracycline plus b-lactam OR linezolid alone Pediatric considerations Cannot use tetracyclines in kids < 8 yoa In hospitalized children vancomycin is recommended Recurrent MRSA SSTI Management: Personal hygiene and good wound care Environmental hygiene measures Consider decolonizing Treat with antibiotics if active infection Treat symptomatic contacts Take Home Points MRSA rates are high among adult and pediatric patients presenting to the ED, and increasing in India I&D is primary treatment of abscesses Needle aspiration is not as effective Packing may be painful and does not affect outcome No need to treat simple abscess with antibiotics Take Home Points If you do treat with antibiotics, cover for MRSA Treat if recurrent, systemic illness, comorbidities, cellulitis Questions? References Duong, M., Markwell, S., Peter, J. and Barenkamp, S. (2010). Randomized, Controlled Trial of Antibiotics in the Management of Community-Acquired Skin Abscesses in the Pediatric Patient. Annals of Emergency Medicine, 55, 401-407. Edlich, R. F., Cross, C. L., Dahlstrom, J. J and Long, W. B. (2010). Modern Concepts of the Diagnosis and Treatment of Necrotizing Fasciitis. Journal of Emergency Medicine, 39.2, 261-265. Gaspari, R. J. et al (2011). A Randomized Controlled Trial of Incision and Drainage Versus Ultrasonographically Guided Needle Aspiration for Skin Abscesses and the Effect of Methicillin-Resistant Staphylococcus aureus. Annals of Emergency Medicine, 57, 483-491. Hankin, A. (2007). Are Antibiotics Necessary After Incision and Drainage of a Cutaneous Abscess? Annals of Emergency Medicine, 50, 49-51. Lee, M. C. et al (2004). Management and outcome of children with skin and soft tissue abscesses caused by communityacquired methicillin-resistant Staphylococcus aureus. Pediatric Infectious Diseases, 23.2, 123-127. Liu, C. et al (2011). Clinical Practice Guidelines by the Infectious Diseases Society of America for the Treatment of Methicillin-Resistant Staphylococcus Aureus Infections in Adults and Children. Clinical Infectious Diseases, 52, 1-38. Moran, G. J. et al (2006). Methicillin-Resistant S. aureus Infections among Patients in the Emergency Department. New England Journal of Medicine, 355, 666-674. O’ Malley, G. F. et al (2009). Routine Packing of Simple Cutaneous Abscesses Is Painful and Probably Unnecessary. Academic Emergency Medicine, 16.5, 470-473. Schmitz, G. R. (2011). How do you treat an abscess in the era of increased community-associated methicillin-resistant staphylococcus aureus (MRSA)? Journal of Emergency Medicine, 41.3, 276-281. Schmitz, G. R. et al (2010). Randomized Controlled Trial of Trimethoprim-Sulfamethoxazole for Uncomplicated Skin Abscesses in Patients at Risk for Community-Associated Methicillin-Resistant Staphylococcus aureus Infection. Annals of Emergency Medicine, 56, 283 – 287.