* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Syncope - ACM
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
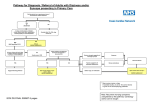
Electrocardiography wikipedia , lookup
Syncope The only difference between syncope and sudden death is that in one you wake up.1 UHN/MSH AIMGP Seminar 2007 Yash Patel 1 Engel GL. Psychologic stress, vasodepressor syncope, and sudden death. Ann Intern Med 1978; 89: 403-412. References Neurocardiogenic Syncope. New England Journal of Medicine 10 March 2005. 352(10): 1004-1010. Guidelines on Management of Syncope – Update 2004. European Heart Journal 25: 2054-2072. Vasovagal Syncope. Ann Intern Med Nov 7 2002; 133(9):714-725. Incidence and Prognosis of Syncope. NEJM 347(12):878-85. Sept 2002. Primary Care: Syncope. NEJM 343(25):1856-1862. Dec 2000. AHA Statement on Evaluation of Syncope. Circulation 113:316-327. Jan 2006. Outline 1. Objectives 2. Definitions 3. Differential diagnosis 4. Approach 5. Treatment 6. Extra material Objectives Learn to distinguish syncope from other “non-syncopal” conditions that lead to transient loss of consciousness Develop an approach to the assessment of patients with syncope How to risk stratify patients with syncope When to hospitalize patients with syncope Case 1 35 Woman Unwitnessed loss of consciousness (1st. Event) No palpitations or preceding symptoms PMH: Hypothyroidism on replacement Exam normal No sequelae No injuries IS THIS SYNCOPE? WHAT IS SYNCOPE? Some Definitions Syncope: sudden, transient loss of consciousness and postural tone with spontaneous recovery without therapeutic intervention Presyncope: no actual loss of consciousness Vertigo: Dizziness accompanied by a sense of motion Drop attacks: spontaneous falls while standing or walking without LOC Is it Syncope or Seizure? Syncope: – Precipitant: pain, exercise, micturition, defecation, anxiety – Preceding sx: sweating and nausea – Event: LOC usually <5 min – Followed by: prompt recovery Seizure: – Preceding sx: aura, jacksonian march – Event: clonic or myoclinic jerks, LOC >5 min, incontinence – Followed by: slowness, neurological deficits, postictal paresis Epidemiology of Syncope Population based incidence (Framingham): Men Women 3% per yr. 3.5% per yr. It increases with age: 35 - 44 y/o > 75 y/o 0.7% per yr. 6% per yr. Case 1 35 Woman Unwitnessed loss of consciousness (1st. Event) No palpitations or preceding symptoms PMH: Hypothyroidism on replacement Exam normal No sequelae No injuries IS THIS SYNCOPE? YES, THIS WAS PROBABLY A SYNCOPAL EVENT REMEMBER SYNCOPE IS A SYMPTOM NOT A DIAGNOSIS Case 2 70 Woman PMH: CAD - Previous MI CABG x 3 10 yr. Ago Meds: Metoprolol, ASA, Fosinopril, recently started on clarithromycin for CAP Witnessed syncope lasting 15 sec. Palpitations prior to event ECG: Inferior Q waves, no arrhythmias WHAT IS THE CAUSE OF HER SYNCOPE? Syncope: Etiology NeurallyMediated 1 • Vasovagal • Carotid Sinus • Situational Cough Postmicturition 24% Orthostatic 2 3 • Brady • Drug Induced • ANS Failure Sick sinus AV block Primary Secondary 11% Cardiac Arrhythmia • Tachy VT* SVT Structural CardioPulmonary NonCardiovascular 4 • Aortic Stenosis • HOCM • Pulmonary Hypertension 5 • Psychogenic • Metabolic e.g. hyperventilation • Neurological 4% 12% • Long QT Syndrome 14% Unknown Cause = 34% Case 2 70 Woman PMH: CAD - Previous MI CABG x 3 10 yr. Ago Meds: Metoprolol, ASA, Fosinopril, recently started on clarithromycin for CAP Witnessed syncope lasting 15 sec. Palpitations prior to event ECG: Inferior Q waves, no arrhythmias WHAT IS THE APPROACH TO EVALUATING SOMEONE WITH SYNCOPE? Approach 1. Hx, Physical and ECG form core workup (yields diagnosis in ~ 50 % of cases) 2. Cardiac causes carry a worse prognosis and should be excluded first 3. Exertional syncope or existing heart disease predicts worse outcomes and warrants more intense investigation 4. In the elderly think of polypharmacy History: focus on... Precipitating Factors – exertion, position, neck or arm movement, specific activities (urination, defecation) and stressful situations Associated Symptoms: – Nausea, diaphoresis, blurred vision - vasovagal – Diarrhea, Vx, GI bleed - volume contraction – Prodromal aura, incontinence - seizure Medications: – side effects, overdose, interactions – antiHTN, Digoxin, diuretics, antibiotics Family Hx: Long QT, WPW, HOCM, CAD, Brugada Syndrome Physical Exam: focus on... Vitals: Orthostatic, BP in both arms CSM (avoid if carotid bruits present) Cardiac exam Neurologic exam Misc: Pulses, bruits, OB in stool Case 2 70 Woman PMH: CAD - Previous MI CABG x 3 10 yr. Ago Meds: Metoprolol, ASA, Fosinopril, recently started on clarithromycin for CAP Witnessed syncope lasting 15 sec. Palpitations prior to event ECG: Inferior Q waves, no arrhythmias SHOULD SHE BE ADMITTED TO HOSPITAL? WHAT INVESTIGATIONS ARE INDICATED? When to Hospitalize? 1. For Investigation: structural heart disease, arrhythmias or ischemia (palpitations or chest pain), or abnormal ECG 2. For Treatment: obstructive HD, severe orthostasis, or adverse drug reactions 3. Consider in all patients with injury following syncope Investigations for Suspected Cardiac Syncope Guided by history, physical and clinical suspicion (ie/risk factors, age >60) Echo - abnormalities found in 5-10 % but these may not relate to sx Stress testing if ischemic arrhythmia suspected Prolonged ECG recording Electrophysiologic testing If above testing is negative and syncope recurrent, evaluate for neurally mediated syncope ECG Features Suggesting Arrhythmic Etiology Bifasicular block Intraventricular conduction abn (QRS>.12) Mobitz II AV block Sinus brady, sinus block or sinus pause >3 sec in absence of negative chronotropes Pre-excited QRS Prolonged QT Brugada Syndrome:RBBB and ST elevation V1-V3 Neg T waves in R precordial leads, epsilon waves and ventricular late potentials (ARVD) Q waves Electrocardiographic Monitoring “ECG monitoring is unlikely to be helpful in patients who do not have clinical or ECG features suggestion an arrhythmic syncope and therefore should not be performed” Electrocardiographic Monitoring In hospital monitoring if high risk Holter monitoring – True + (arrhythmias with sx) ~ 4% of tests – True - (sx with no arrhythmia) ~ 17% of tests Loop recording for longer monitoring – External if inter-symptom interval <4 wks Consider EPS in anyone with structural heart disease with a non-diagnostic Holter Case 3 82 Man PMH: HTN, BPH, Glaucoma, COPD, Depression Meds: Diltiazem, ASA, Salbutamol, Ipratropium, Prazosin, Paroxetine, Tyl #3, Omeprazole Syncope while urinating in early AM, shortly after rising Trauma to forehead from episode YOUR DIAGNOSIS IS NEURALLY-MEDIATED SITUATIONAL SYNCOPE WHAT INVESTIGATIONS DOES HE NEED? Investigations for Suspected Neurally Mediated Syncope The majority of patient with single or rare episodes do not require confirmatory tests Investigations in patients without suspected heart disease and recurrent or severe syncope: – Tilt testing – Carotid massage – Prolonged ECG monitoring Case 1 Case 2 Case 3 35 Woman Unwitnessed loss of consciousness (1st. Event) No palpitations or preceding symptoms PMH: Hypothyroidism on replacement Exam normal No sequelae No injuries 70 Woman PMH: CAD - Previous MI CABG x 3 10 yr. Ago Meds: Metoprolol, ASA, Fosinopril, recently started on clarithromycin for CAP Witnessed syncope lasting 15s Palpitations prior to event ECG: Inferior Q waves, no arrhythmias 82 Man PMH: HTN, BPH, Glaucoma, COPD, Depression Meds: Diltiazem, ASA, Salbutamol, Ipratropium, Prazosin, Paroxetine, Tyl #3, Omeprazole Syncope while urinating in early AM, shortly after rising Trauma to forehead from episode WHAT IS THE PROGNOSIS FOR EACH OF THESE PATIENTS WITH SYNCOPE? Risk Stratification and Prognosis in Syncope Structural heart disease is the most important predictor of mortality and sudden death in patients with syncope Poor Prognosis Structural heart disease Excellent Prognosis Young, healthy, normal ECG Neurally-mediated syncope Orthostatic hypotension Unexplained syncope Prognosis in Syncope (from Framingham database) Etiology Total Mortality 1yr 5yr Cardiac Noncardiac 15% 40% 5% 2% 30% 15% 5% 25% 2% 15% Neurologic Vasovagal/Others Unknown Controls w/o syncope NEJM 2002;347:878 Summary Syncope is a common symptom History/Physical can establish a diagnosis in 50% of cases The approach involves risk assessment for the presence of cardiac disease Investigations and Treatment are tailored to the suspected etiologic cause of syncope Extras... Driving after syncope Treatment of syncope Mechanism of Vasovagal syncope Tilt-table testing Neurologic evaluation Psychiatric evaluation Driving and Syncope Driving and Syncope Physicians are obliged to disclose risk of driving to patients and advise them not to drive 7 provinces (including Ontario) and all territories have mandatory reporting legislation Single episode of vasovagal Dx and tx cause (ie/ PPM) Reversible cause (ie/ hemorrhage) Situational w/avoidable trigger Unexplained Single episode Recurrent Recurrent Private Commercial No restriction No restriction Wait 1 week Wait 1 month No restriction No restriction Wait 1 week Wait 1 week Wait 1 week Wait 3 months Wait 12 months Wait 12 months Wait 1 week Wait 12 months Syncope and Driving Further guidelines exist for patients with arrhythmia, MI, valvular heart disease and devices See CCS Consensus Conference 2003: Assessment of Cardiac Patients for Fitness to Drive and Fly. Canadian Journal of Cardiology, 2004, 20(13): 1313-1323. Treatment of Syncope Treatment Identifiable arrhythmia, structural heart disease, or non-syncopal event: Rx accordingly Treatment: Neurally-Mediated Education and reassurance usually sufficient Additional treatment may be warranted if: – Very frequent – Unpredictable and exposes pts to trauma It may be valuable to assess the relative contribution of cardioinhibition and vasodepression Treatment: Nonpharmacologic Avoid trigger events Modify or discontinue hypotensive drugs Other – – – – – Increase fluid intake (2L water/day) Salt supplements Isometric leg and arm counter-pressure maneuvers Tilt training Compression Stockings Treatment: Drugs Beta-blockers discouraged in 2004 ESC guidelines Other meds with limited evidence: – Fludricortisone – Midodrine – SSRIs – Others Treatment: Devices Permanent dual chamber pacing may have a role in: – Those with no prodrome – Failure of other therapies – Profound bradycardia or asystole during syncope >5 attacks per year Age >40 Mechanism of Vasovagal Syncope Mechanism of Vasovagal Syncope Bezold–Jarisch Reflex: Excessive venous pooling triggers a chain of events that culminates in vasodilatation and bradycardia (instead of the physiologic compensatory responses of vasoconstriction and tachycardia) This in turn leads to the hypotension and loss of consciousness associated with vasovagal syncope. Common Triggers in Situational Syncope Defecation Micturition (especially in elderly men with BPH that wake up at night and strain to pass urine) Heavy straining Cough All situations that induce valsalva => – decreased preload + – cardioinhibitory and vasodepressor reflexes produced by central baroreceptors Tilt-Table Testing Vasovagal Syncope Test = Head Up Tilt-table testing using a provocative agent (Isoproterenol or Nitroglycerin): Sn and Sp difficult to evaluate because of lack of gold standard ACC has guidelines on testing (JACC 1996:28 pg 263-275) Head-up Tilt table testing Indicated in: 1. Recurrent syncope 2. Single syncopal event resulting in injury or occurring in high risk setting 3. Where the treatment of syncope may be complicated by vasovagal symptoms Contraindicated in presence of obstructive heart disease or cerebrovascular stenosis Neurologic and Psychiatric Testing Neurologic Testing Low yield: – EEG ~ 2% – CT head ~ 4% – Doppler carotids (no studies) The majority of positives can be identified by history: e.g. seizure events Bottom line: only indicated if suspicion of seizure or neuro deficits present Psychiatric evaluation Syncope can be a feature of: – Anxiety disorders: Gen anxiety or panic – Somatization – Substance abuse These tend to occur recurrently in younger patients without heart disease In elderly patients organic (i.e. cardiac) causes must be excluded