* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Title of Presentation
Survey
Document related concepts
Transcript
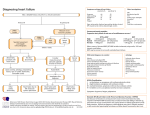
Cardiorenal Syndrome Samira Tabiban MD Rajaie Cardiovascular medical and research center Cardiorenal syndrom • • • • Definition Classification Pathophysiology Treatment Definition Of CRS The CRS can generally be defined as a pathophysiological disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other organ. The cardiorenal syndrome (CRS) Definition Heart failure with… Worsening renal function (> 25-30% increase in creatinine or BUN during treatment for acute decompensation) High Prevalence of Renal Dysfunction and Its Impact on Outcome in 118,465 Patients Hospitalized With Acute Decompensated Heart Failure: A Report From the ADHERE Database J. Thomas Heywood MD et al J Card Failure Sept 2007 65% Have at least Moderate renal dysfunction Inpatient mortality from ADHERE Registry Based on admission BUN, creatinine and BP < BUN 43 (n=32220) 2.88% (n=24469) < < 2.31% (n=20820) 15.30% (n-1863) SBP 115 (n=2,702) 5.67% (n=3882) 8.35% (n=67640) < 13.23% (n-1270) SBP 115 (n=6697) Cr 2.75 (n-1862) 5.63% (n-4834) 19.76% (n-592) Analysis of patients in the National Acute Decompensated Heart Failure National Registry (ADHERE) BUN=blood urea nitrogen, Cr=serum creatinine, SBP-systolic blood pressure Fonarow GC et al. J Cardiac Fail 2003;9(suppl 1):S79. Why is renal function abnormal in patients with heart failure? Role of the kidney in congestive heart failure: Relationship of CI to kidney function RBF, p<.05 with Group A 500 Renal Blood Flow 400 Renovascular 200 Resistance 100 RVR, p<.01 with Group A 300 0 Renal BF RV Resistance A, CI> 2 B, CI>1.5 <2.0 C, CI <1.5 Ljungman, Cody Drugs 1990;39 Suppl 4:10-21 Role of the kidney in congestive heart failure: Relationship of CI to kidney function CI, p<.001 with Group A 70 BUN, p<.01 with Group A 60 GFR / BUN 50 40 GFR BUN 30 20 10 0 A, CI> 2 B, CI>1.5 <2.0 C, CI <1.5 Creatinine was not different between the groups. BUN better indicated low CI and GFR than creatinine Ljungman, Cody Drugs 1990;39 Suppl 4:10-21 ` Am J Cardiol 2006:97:1759 Effect of increasing central venous pressure on GFR in dogs, constant BP 1.4 Raised Venous Pressure: A direct cause of renal sodium retention P< .05 GFR 1.1 Ml/min P< .05 0.8 Firth et al Lancet 5/7/88 High CVP significantly impairs GFR 0.5 0 6.25 12 18.75 25 mm Hg 0 Central Venous Pressure Effect of Increased Renal Venous Pressure on Renal Function Doty J et al J of Trauma: Injury, Infection and Critical Care 1999 47:1000-1005 • • Swine where anesthetized, instrumented and a unilateral nephrectomy preformed. In the remaining kidney the renal vein was constricted in half the animals to obtain a renal venous pressure of 30, the other animals served as controls 30 P <.05 between groups 25 20 15 Control RV Constric 10 5 0 RA Blood flow Index GFR Aldosterone Renin Activity Renal Decapsulation in the Prevention of Post-Ischemic Oliguria Stone HJ Annals of Surgery 1977:343-355 • 15 rhesus monkeys, 1 hour suprarenal aortic clamping to produce ATN, after which the renal capsule was stripped from one kidney. The ureters of each kidneys were catheterized to collect urine for creatinine, urea and free water. 7 6 P <.01 5 4 Decapsuled Control 3 2 1 0 Cr Cl Urea Cl Free Water Prevalence of Worsening Renal Function During Hospitalization According to Categories of Admission CVP, CI, SBP, and PCWP Mullens, W. et al. J Am Coll Cardiol 2009;53:589-596 Treatment of the Cardiorenal Syndrome 5 important questions… • • • • • What is the fluid status? Is the blood pressure adequate for renal perfusion? What is the cardiac output? Is there evidence of high central venous pressure? Is there intrinsic renal disease? Hypovolemic Cardiorenal Syndrome Too Dry!!! • Overdiuresed or intercurrent illness results in volume loss and renal dysfunction • Give fluids, stop diuretics and IV vasodilators • Often a reluctance to give fluids to HF patients but it may be critical in this situation and time is of the essence to avoid irreversible renal damage CRS due to high central venous pressure Too Wet!!! • Poor renal perfusion due to high central venous pressure • Usually CVP > 15-20 mm Hg coupled with reduced blood pressure • Diuretics often held because of worsening renal function and misguided idea of “ intravascular volume depletion” • Continue diuretics to reduce central venous pressure • Ultrafiltration CRS with vasoconstriction Clamped Down!!! • Low CO and hence renal hypoperfusion due to HF mediated vasoconstriction (Ang II, endothelin induced increased afterload) • CO is low and SVR high, often over 1800-2000 • ACEI and vasodilators very useful since CO can increase significantly if afterload normalized. Actual improvement in renal function may be seen • May need temporary inotropic support if systolic BP <80 as vasodilators are added (J Am Coll Cardiol 2014;63:853–71) “Although there is no serum creatinine level per se that contraindicates ACE inhibitor therapy, greater increases in serum creatinine occur more frequently when ACE inhibitors are used in patients with underlying chronic renal insufficiency.” ACEI play a complex role in renal function in HF • May improve CO in some patient and hence increase effective renal perfusion • ACEI may lower BP to the point where effective renal perfusion is impaired • With chronic renal disease, there is hyperfiltration in the remaining nephrons. ACEI decreases efferent arteriole constriction and hence decreases glomerular capillary pressure which may preserve renal function longterm • This may result in a 10-20% increase in creatinine, but over the long term renal function is preserved CRS with vasodilation “Vasodilated!!” • Renal hypoperfusion due to low perfusion; CO may be normal but SVR and BP low • Vasodilators worsen BP and hence renal perfusion • Stop of ACEI, especially if SVR is low • Rule out sepsis • Pressors, Inotropes, ? Vasopressin • Consider transplant or ventricular assist device if renal dysfunction is felt to be reversible CRS with normal CO and SVR “It’s the Kidneys, Not the Heart!!!!”” • Consider intrinsic renal disease (IRD) or diuretic resistance syndrome, renal artery stenosis • Probable IRD when long hx of HTN and/or diabetes, look for proteinuria, renal artery stenosis • Trial of loop diuretic infusion, combination with distal tubular diuretic • Add nesiritide • Consider ultrafiltration Invasive hemodynamic monitoring should be considered in a patient: • who is refractory to initial therapy, • whose volume status and cardiac filling pressures are unclear, • who has clinically significant hypotension (typically SBP !80 mm Hg) or worsening renal function during therapy, Or • who is being considered for cardiac transplant and needs assessment of degree and reversibility of pulmonary hypertension, Or in whom documentation of an adequate hemodynamic response to the inotropic agent is necessary when chronic outpatient infusion is being considered. (Strength of Evidence 5 C) Profiles of the Cardiorenal Syndrome CRS due to: Fluid Status CO CI SVR Proteinuria Too Dry!!! Dry Low Nml or high None Fluids, stop diuretics Too Wet!!! (high CVP) Wet Nml Nml None Continuous diuretic infusion, distal tubular diuretic, ultrafiltration Too Clamped Down!!! Wet or Nml Low High None ACEI, Nitroprusside, Nesiritide, Relaxin Nml or high Low None Vasodilated!!! Nml or wet Stop ACEI, Pressors, Vasopressin Inotropes, VAD Low Nml None No Pump!!! Wet or Nml Inotropes, Vasopressors Balloon Pump LVAD Wet Nml Nml None Continuous diuretic infusion, distal tubular diuretic, ultrafiltration Intrinsic Renal Disease/Diureti c Resistance Treatment Volume Management Concept of Plasma Refill Rate in ADHF Diuretics to increase sodium loss and decrease venous pressures Redefining the Therapeutic Objective in Decompensated Heart Failure: Hemoconcentration as a Surrogate for Plasma Refill Rate Boyle and Sbotka J Card Failure May 2006 Concept of Plasma Refill Rate in ADHF Diuretics to increase sodium loss and decrease venous pressures Hemodynamic Changes No Hemoconcentration Hemoconcentration P value RA pressure -2.8±5.6 -5.4± 0.031 Pulm Art Sys Pres -9.0±12.4 -14.4±10.8 0.124 Wedge Pressure -6.2±8.3 -12.6±9.6 0.015 Hemoconcentration No Hemoconcentration Secondary Endpoints: Low vs. High Intensification Low High P value Dyspnea VAS AUC at 72 hours 4478 4668 0.041 % free from congestion at 72 hrs 11% 18% 0.091 -5.3 lbs -8.2 lbs 0.011 3575 mL 4899 mL <0.001 % Treatment failure 37% 40% 0.56 % with Cr increase > 0.3 mg/dL at 72 hrs 14% 23% 0.041 6 5 0.55 Change in weight at 72 hrs Net volume loss at 72 hrs Length of stay, days (median) Changes in Creatinine over Time *: High vs. Low 1.8 p = 0.34 1.75 Low High p = 0.59 1.7 Creatinine (mg/dL) p = 0.85 1.65 p = 0.07 p = 0.81 p = 0.28 1.6 1.55 1.5 1.45 0 1 2 3 4 7 Time (days) * P values are for change in creatinine from baseline 60 Proportion with Worsening Renal Function: High vs. Low 25% Low % with Δ Cr > 0.3 mg/dL 20% High 15% 10% 5% 0% 0 1 2 3 Time (days) 4 7 60