* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Drug Treatment Choice in Older Adults with Urinary Incontinence
Orphan drug wikipedia , lookup
Compounding wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Psychopharmacology wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Theralizumab wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmacogenomics wikipedia , lookup
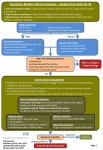
Drug Treatment Choice in Older Adults with Urinary Incontinence Catherine E. DuBeau, MD Professor of Medicine Director, Geriatric Continence Clinic Co-Director, Urology Resident Geriatric Education Program Disclosures Pfizer Astellas Novartis Drug Choice for UI in Older Adults Factors in Management - Ease of Use Efficacy Tolerability Pathophysiology Drug Choice for UI in Older Adults Factors in Management - Ease of Use Efficacy Tolerability Aging Comorbidity Pathophysiology Pathophysiology Homogeneity of Youth Punk rockers, 1978 Heterogeneity of Age Punk rockers, 2008 Aging effects on UI drug effects • Pharmacokinetics • Pharmacodynamics • Age-related changes in micturition – – – – Structure Function Receptors Impact of comorbidity on voiding and toileting Pharmacokinetics in Older Persons - 1 Absorption • • • • Healthy: No change Neuro & GI disease: impaired swallowing Diabetes, anticholinergics: delayed gastric emptying Frail: decreased subcutaneous fat affecting topical absorption Distribution • Healthy: No change • Inactive, frail: low muscle, higher fat mass – Longer half life of lipophilic agents – Higher serum concentration of water soluable agents • CNS penetration..? Water soluble agents Tight junction Lipophilic agents Plasma proteins Cationization Drugs Efflux pumps Transport proteins Metabolism Neuwelt EA. Neurosurgery 2004; 54:131-142 Blood-Brain Barrier in Age & Aging-related Diseases • Data from studies using CSF/serum albumin ratio (C/s) as indication of BBB dysfunction – C/s increases with age – C/s correlates with severity of white matter signal abnormalities (WMSA) on CT in pts with and without dementia • WMSA also associated with vascular risk factors (HTN, DM, hyperlipidemia • WMSA associated with urgency severity Blennow et al, Eur Neurol 1993; Wallin et al, Eur Neurol 2000: Kuchel GA et al, AGS 2008 Pharmacokinetics in Older Persons - 2 Metabolism • Healthy – No change in hepatic glycosylation – No definite change in P450 enzymes – Hepatic mass and blood flow: less first-pass effect and increased serum levels of un-metabolized drug • Comorbid disease – Further decrease in hepatic mass and blood flow – Polypharmacy - medications that induce or inhibit P450 enzymes Clearance • Healthy – Renal: small decrease in GFR • Comorbid disease – Renal: Significant decrease in GFR, under-estimated by serum creatinine – GI: decreased transit time Pharmacodynamics • Age-related changes in detrusor muscarinic receptors – Normal contraction: M3 > M2 effect – With age: Decrease in M3 but not M2 mRNA – Age-related decrease in M receptor number in men (aging vs obstruction effect?) – Decrease in muscarinic-mediated contraction • Extrapolation to clinical data uncertain Mansfield KJ. et al. Brit J Pharmacol 2005, 144:1089 Andersson KE. Schroder A. Urologe (Ausg. A) 2004, 43:552 Impact of Comorbidity: Polypharmacy Polypharmacy is the norm for older patients – Average number of meds = 5 – Among older women reporting medication use in previous week, 57% took > 5 agents – Current disease guidelines promote polypharmacy • Recommended regimen for 74 yo woman with HTN, DM, CHF, arthritis, osteoporosis = 12 meds, taken at 4 different times during the day – Leads to burden and cost disincentives to adding another drug Boyd CM et al. JAMA 2005, 294:716 Kaufman DW et al. JAMA. 2002, 287:337 Ernst ME. Iyer SS, Doucette WR. Value in Health. 2003, 6:51 Impact of Drugs on Continence and LUTS in Older Persons Nocturia Nifedipine “Glitazones” NSAIDs/COX2 Gabapentin Pregabalin Constipation Calcium blockers Anticholinergics Narcotics Mobility Antipsychotics Mentation Sedative hypnotics Benzos Anticholinergics Stress UI ACE inhibitors LUT function Decrease contractility Anticholinergics Calcium blockers Sphincter tone Alpha agonist Sphincter tone Alpha blocker Diuretics Common Drugs for Common Conditions Nocturia Nifedipine “Glitazones” NSAIDs/COX2 Gabapentin Pregabalin Constipation Calcium blockers Anticholinergics Narcotics Mobility Antipsychotics Mentation Sedative hypnotics Benzos Anticholinergics Stress UI ACE inhibitors LUT function Decrease contractility Anticholinergics Calcium blockers Sphincter tone Alpha agonists Sphincter tone Alpha blockers Diuretics Use of Medications Affecting Continence in Women (median age 80) Attending a Geriatric Continence Clinic GCC Patient Use of Medications that Could Affect Voiding Symptoms and their Treatment (n= 66) Effect on continence, LUTS, and antimuscarinic drug treatment Medication % NSAIDs Ca+ Blocker Steroids Glitazone Narcotics Tricyclic antidepressant Atypical antipsychotic Antispasmodic Loop diuretic Hypnotic Estrogen Benzodiazepene Calcium Other antidepressants* ACE Inhibitor 20 35 3 45 8 Pedal edema X X X X DU Urine Output Cognition X Bowels Cough Incr UI Drug – drug interact X X X X X 5 X X X 3 3 9 2 5 5 20 X X X X X X X X X 6.1 29 X X X X X X X X DuBeau and Shanti, Am Geriatr Soc Annual Meeting, 2006 The Prescribing Cascade 77 yo woman with urgency; gets nifedipine for HTN Edema, constipation, impaired bladder emptying Nocturia, urgency, some UI OAB! Add antimuscarinic constipation Add laxative.... The Prescribing Cascade 77 yo woman with urgency; gets nifedipine for HTN Edema, constipation, impaired bladder emptying Nocturia, urgency, some UI OAB! Add antimuscarinic constipation Add laxative.... Efficacy “Do urge UI drugs work in older persons?” Oxytolfesosolidaritros in Patients Aged > 65 yr Analysis of pooled phase III fixed dose clinical data Oxytolfesosolidaritros in Patients Aged > 65 yr Analysis of pooled phase III fixed dose clinical data Placebo 2.7 mg Median % Change UI QoL Placebo 5.4 mg 0 -20 -40 -34.8% Perception -44.8% -60 -66.7% -80 † -75.9% † Placebo OAB Drug A “Older patients” in trials often much healthier than those in primary care <65 y >65 y OAB Drug A OAB Drug B UIE Decrease UIE A B 65 - 70 y -2.5 -1.0 71 - 75 y -2.5 -1.0 > 75 y -2.5 -2.5 Total mean -2.5 -1.5 <65 y >65 y Problems with existing efficacy studies • Inadequate heterogeneity of study population – Lack of racial-ethnic and SES diversity – Include only cognitively and functionally intact – Exclusion of comorbidities known to affect micturition and continence – Limited to patients with high daytime frequency (>8 times daily) – Failure to include older- and oldest-old – Failure to include or assess whether patients have age-related detrusor underactivity (“DHIC”) Problems with existing efficacy studies • Little to no stratification by age group • No stratification by comorbidity • Little stratification by previous treatment No multivariate analyses despite large N’s If you control for age, you can’t evaluate it Efficacy: Are we looking at the right outcomes? • Patient perception: interaction with expectations? – – – – Patient (and family) concerns about adverse drug effects Marginal trade-off: drug benefit vs polypharmacy and cost Dissatisfaction with previous inadequate treatment Previous encounters with ageist providers • Nocturia: never normalized to hours in bed/sleeping • QoL and Bother – Few scales derived using patient-based data from older persons – Floor effects regarding “social” and “role” functions – None validated in oldest old, cognitively +/- functionally impaired – Alternative measures: in nursing home residents, prevalent and especially incident UI have negative impact on social interactions DuBeau et al, J Am Geriatr Soc 2006 DuBeau et al, J Am Geriatr Soc 1998 What do older persons want from treatment? Variance in Limitation in Daily Life from OAB • Bother - 42% Urgency and Nocturia • UI - 17% • Urgency/Frequency - 12% • Nocturia - 11% Treatment, months Michel MC et al, Neurourol Urodynam 2007 ADE Risk in Older Patients Functional capacity Minimum function • Not due to chronological age • Important factors vary by individual needed (eg, GFR >20) – Pharmacokinetic changes – Pharmacodynamic changes – Physiologic • Age-related changes in organ systems • Comorbidity and associated medications • Decreased functional reserve: “homeostenosis” Age/Disease Gurwitz and Avorn, Ann Int Med 1991 Safety of OAB Drugs in Older Persons Consider number needed to harm (NNH) - inverse of attributable risk – Typical antimuscarinic – Decrease in urge UI: drug 70%, placebo 44% – Dry mouth: drug 28%, placebo 10% – NNT = 1/.26 = 3.8 Takes only 2 more pts to see harm – NNH = 1/.18 = 5.6 Cognitive Impairment from Antimuscarinics? • Case reports • RCTs using non-standard cognitive measures – Oxybutynin “worse than Benadryl” (Katz, JAGS 1998) – Quantitative EEG studies: oxybutynin worse than tolterodine, trospium (Todorova, J Clin Pharmacol 2001) • Epidemiological studies – Prescription-event monitoring: more hallucinations with tolterodine than 10 non-antimuscarinic, non-CNS active drugs, RR = 4.85 (95% CI, 2.72-8.66) (Layton, Drug Safety 2001) use of – 372 elderly in France: anticholinergics associated with impairments in multiple domains of a cognitive battery (Ancelin, BMJ 2006) Evidence for Cognitive Impairment from Antimuscarinics • RCTs using standard cognitive batteries – Nursing home residents: oxybutynin ER 5 mg daily did not increase incidence of delirium (measured by CAM) over placebo (Lackner, JAGS 2008) – Older healthy patients: in 3-period crossover trial, variable doses of darifenacin no different than placebo on computerized cognitive battery; however, no intrapatient comparisons, only half of eligible patients randomized (Lipton, J Urol 2005) – Older healthy patients: oxybutynin ER did and darifenacin did not cause more impairment in delayed recall than placebo (Kay, Eur Urology 2006) 3 week RCT Comparing Darifenacin, Oxybutynin ER and Placebo Delayed Name-Face Association Test (lower score = worse) 7 6 5 *† *† Darifenacin (n=46) Oxybutynin ER (n=49) Placebo (n=50) 4 0 Baseline Week 1 Week 2 Week 3 Kay G et al, Eur Urol 2006 Was the Study Design Biased? High starting dose 7.5 mg 10 mg 7.5 mg 15 mg Different titration schedule 15 mg 20 mg Very high end dose 7 Are other commonlyused drugs even worse? 6 5 *† *† Darifenacin (n=46) Oxybutynin ER (n=49) Placebo (n=50) 4 0 Baseline Week 1 Kay G et al, Eur Urol 2006 Week 2 Week 3 3 week RCT Comparing Darifenacin, Oxybutynin ER and Placebo • No differences between darifenacin, oxybutynin ER, and placebo on other tests of delayed recall, immediate recall, visual attention, psychomotor reaction time, information processing speed, or selfrated memory. • In the French community study, anticholinergics were not associated with impairment in delayed recall Kay G et al, Eur Urol 2006; Ancelin, BMJ 2006 Drug-Drug Interactions • Agents utilizing CY2D6 and 34A ubiquitous in primary care • Highly protein-bound drugs (eg, trospium) can compete with digoxin, increasing digoxin serum levels – Toxic digoxin level lower in elderly (> 0.8) • Antimuscarinics may add to pre-existing anticholinergic burden • Implications – Accept and acknowledge drug-drug interactions as fact of life – Use of electronic tools/EMR for checks and alerts Drug-Disease Interactions: The Example of Diabetes • • • • • • Renal impairment: drug clearance Slowed gastric motility: drug absorption Constipation: ADE risk and impact Cognitive impairment: ADE risk and impact Glycosuria: masks antimuscarinic efficacy DM medications – – – – – “Glitazones”: CHF; pedal edema causing nocturia Metformin: competes for clearance with trospium ACE inhibitors: cough exacerbates mixed UI Gabapentin, pregabalin: edema causing nocturia Tricyclics: PVR , constipation Drug Choice for UI in Older Adults Factors in Management - Ease of Use Efficacy Tolerability Aging Comorbidity Pathophysiology Pathophysiology Choosing an Antimuscarinic • • • • • • Cost (variable) Dose size and escalation (start Detrol LA 2 mg; Ditropan XL widest range) Once daily vs other dosing (extended release forms best) Timing with other meds, meals (trospium: empty stomach) Drug-drug interactions (CYP 2D6 – SSRIs; 3A4 - antifungals, macrolides) Drug-disease interactions (trospium – renal clearance) No Differences All decrease UI ~70%, ~25% cure rate Efficacy • Dry mouth: oxybutynin worst • Constipation: darifenacin, solifenacin worst • Least: Oxytrol patch (but rash in 15%) Tolerability Adverse effects 4th International Consultation on Incontinence, 2008 Chapple C et al, Eur Urol 2005 Shamliyan TA et al, Ann Int Med 2008 Research Agenda for Oxytolfesosolidaritros in Older Patients • Efficacy & tolerability – Assess across a spectrum of comorbidity and impairment – Predictors of response – With and without behavioral interventions – Absolute benefits and risk, NNT and NNH • Patient-based treatment utilities • Outcome measures specific to the spectrum of disease/disability and patient preferences The Example of Dry Mouth • 30% of older people already have it • Most already take at least one drug that causes it • Morbidity: dental caries, problems chewing, poorly fitting dentures, dysphagia, nutritional problems, sleeping difficulty, poor QoL Ship JA et al J Amer Geriatr Soc 2002 Fonda D et al. Frail Elderly, 3rd ICI Age and Physiology • Inter- and intra-individual variability increases • Chronological age poor marker of health status • “Age-associated” vs “age -related” • Both phenomena may be independent of function and symptoms Antimuscarinic Drug Trials in Older Patients • Tolterodine – At 4 weeks, urge UI episodes greater in pts 75 yr (P <0.02) – Reduction in voiding frequency similar in both age groups – No differences in efficacy in pts </> 65 years – No differences in dry mouth by age Malone-Lee et al, JAGS 2001;49:700 Malone-Lee et al, J Urol 2001;165:1452 What is the “placebo effect”? “Perceived” placebo effect • Natural history – Maximum expected improvement 42% at 1 yr (6% at 8 wk) • Regression to mean, esp with severe symptoms at entry – MERIT population 3 UI episodes/day, but 45% sx > 5yr • Time effects related to pts – Early improvement leads to hope for good outcome • Unintended parallel interventions – Earlier improvers may be more likely to perform/continue other behavioral modifications (eg, decrease fluids) What is the “placebo effect”? “True” placebo effect • Conditioning – No difference in previous treatment or its efficacy – Impact of informed consent: improvement is “reasonably expected”; listing of potential side effects • Study participation – Amplification of placebo response by increased hope of good outcomes simply by entering a trial • Outcome measure – If overly sensitive, placebo effect increased – Bladder diary valid/reliable, but subjective/QoL measures? Preserved Plasticity • Systems can continue to adapt and change “despite” advanced age – Weight training increases muscle mass and strength in 90 year olds – Persons who stay intellectually engaged have improved quality of life – New evidence that CNS plasticity preserved What Increases ADE Risk? • Not chronological age • The important factors vary by individual – Pharmacokinetic changes – Pharmacodynamic changes – Physiologic: both co-morbidity (and meds to treat it) and decreased reserve – Functional characteristics Gurwitz and Avorn, Ann Int Med 1991 The Example of Dry Mouth • 30% of older people already have it • Most already take at least one drug that causes it • Morbidity: dental caries, problems chewing, poorly fitting dentures, dysphagia, nutritional problems, sleeping difficulty, poor QoL Ship JA et al J Amer Geriatr Soc 2002 Fonda D et al. Frail Elderly, 3rd ICI Adverse Drug Effects • Common with all drugs in older persons (prevalence 35-66%) • Changes placing elderly at higher risk for anticholinergic AEs: – – – – – Altered cholinergic receptor number and distribution Age and disease effects on blood-brain barrier (BBB) Drug metabolism, drug-drug interactions Pre-existing dry mouth and constipation Impaired visual accomodation The Confusion around Confusion • Incidence unclear – Ditropan XL: “confusion” rate 2 to <5% in all studies – Detrol LA: “confusion” not listed; hallucinations in UK post-marketing survey, 4.5% rate/1000 pt-yrs (95% CI 2.9 – 6.8) – Case reports: “The addled nonagenarian” • Definition unclear – Is it worsening memory? Delirium? Both? – What are the best measures? Do proxy measures (eg, EEG) correlate clinically? US Ditropan XL prescribing information US Detrol LA prescribing information Layton et al, Drug Safety 2001; 24:703 Shader and Oesterheld, J Clin Psychopharm 1995; 15:378 Further Confusion • Unknown if pts with Alzheimer’s truly at higher risk because impaired central cholinergic systems • Concomitant cholinesterase inhibitors: – One case report of delirium in pt also taking bladder relaxant – Unknown if bladder relaxant efficacy affected – Do cholinesterase inhibitors cause UI? – Is the blood-brain barrier the most important factor? Ouslander et al, J Am Med Dir Assoc 2001;2:207-214 Womack and Heilman, Arch Neurol 2003;60:771-773. Impact of DM on Continence Determinants • Function: neuropathy, poor vision, amputation • Cognition: vascular dementia • Comorbidity – – – – CAD/CHF: nocturia Constipation UTIs Med side effects • Glitazones, Avandia: edema → nocturia • ACEI: cough→ stress UI Antimuscarinic Adherence • Medicare Managed Care enrollees ( n ~14,000) with OAB (ICD-9 codes and at least one antimuscarinic Rx q6 mos) (n = 279, 2%) • Medication Possession Ratio (MRP) – # days of Rx dispensed/days between prescription (30 tabs refilled every 30 days = 100% adherence) • OAB antimuscarinics MRP = 0.42 – Higher with better general health perception – Lower with comorbidity and greater # prescriptions – 10% in antimuscarinic MRP associated with 6% total health costs – Unclear if relationship between MRP with costs specific to antimuscarinic Balkrishnan et al, J Urol March 2006 Drug-Drug Interactions • Antimuscarinics add to pre-existing anticholinergic burden • Bladder antimuscarinic metabolism – Agents metabolized via CY2D6 and 34A ubiquitous in primary care • Clinical implications – Drug-drug interactions fact of life for all prescribing – Electronic tools (Epocrates, etc) – Start low: is your formulation small enough? QTc Prolongation and Mortality Risk • Review of 7 prospective cohort studies of prolonged QTc and overall and cardiovascular mortality; n = 36,03; 2677 (8.7%) had QTc >440 msec • 1 study: no association (relative risk, 1.02; 95% CI 0.70-1.49) • 6 studies inconsistent associations overall and across subgroups (age, sex, and comorbidities) • Only consistent findings were in subgroup with prior CV disease – Total mortality, RR 1.1 - 3.8 – CV mortality, 1.2 - 8.0 – Rudden death, 1.0 - 2.1 for • Caveat: cannot directly address QTc prolongation related to medication use • Other interations: impaired lung function, low body weight Montanez M et al, Arch Intern Med. 2004 Sharp DS, Ann Int Med 1998 QTc Prolongation and Mortality Risk • Degree of QTc prolongation during treatment with QTcprolonging drugs is prognostic for the risk of torsade • QTc prolonging drugs should probably not be prescribed for patients with a QTc >460 ms • Medicare database study: no association between antimuscarinics and ventricular arrythmias • Other considerations: concomitant or interval use of other QTc prolonging agents, eg quinolones Elming H, Cardiac Electrophysiol Rev 2002 Wang PS, J Am Geriatr Soc 2002 Upper, Middle, and Lower Quartiles of Life Expectancy by Age Walter, L. C. et al. JAMA 2001;285:2750-2756. Copyright restrictions may apply. Upper, Middle, and Lower Quartiles of Life Expectancy by Age 77 yo man in lower quartile of LE won’t live long enough to experience symptomatic benefit of finasteride over alpha-blocker Walter, L. C. et al. JAMA 2001;285:2750-2756. Copyright restrictions may apply. Anticholinergic use in 372 community-dwelling elderly in France 14% (51) on anticholinergic at baseline 30 still on anticholinergic agent at one year Ancelin M et al, BMJ 2006 Male veterans > 65 yo on > 5 prescribed meds 27% Ness J et al, Am J Geriatr Pharmacother 2006 Placebo OAB Drug A “Older patients” not compared directly with younger patients A - low dose A - high dose Tolerability and Safety Lack of adequate safety info in all drug trials • Analysis of RCTs of drug Rx (HTN in elderly, HIV, antibiotics for sinusitis, thrombolysis, NSAIDs for RA, H Pylori, GI tract decontamination); N = 130,074 pts • Severity of ADEs and toxicity adequately defined in only 39% and 29% of reports • Only 46% stated the frequency of specific reasons for discontinuation due to toxicity • Median space allocated to safety results was same as that devoted to contributor names and affiliation Ioannidis JP & Lau J. JAMA 2001, 285:437