* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Update On OAB
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Clinical trial wikipedia , lookup
Neuropharmacology wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmacokinetics wikipedia , lookup
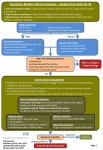
Pharmacogenomics wikipedia , lookup
Update On OAB Joon Chul Kim The Catholic University of Korea Overactive Bladder Syndrome : ICS Definition • Urgency, with or without urge incontinence, usually with frequency and nocturia – Absence of pathologic or metabolic conditions that might explain these symptoms • Urgency - Sudden, compelling desire to pass urine that is difficult to defer Abrams P et al. Urology. 2003;61:37-49. Desire to Void (Urge to Void) and Normal Micturition Process Void Intervoid Interval First Sensation Urge Intensity Volume Voided Bladder Volume (—) Intensity of desire to void 300 – 500 cc 100 cc Time Urge: A physiological desire to void • • • Gradual onset Increases as a function of bladder volume Can usually be deferred with appropriate strategies Chapple CR et al. BJU Int. 2004; 94:738-744. Urgency: Micturition Process in OAB Urgency Presumed Normal Void Volume Reduction in Volume Voided Due to Urgency Void Intensity Bladder Volume (—) Desire to Void (voluntary and/or involuntary) Time Reduction of Intervoid Interval Chapple CR et al. BJU Int. 2004; 94:738-744. Urgency Drives the Other Symptoms of OAB Urgency 1 Increased Frequency Nocturia 2 and Reduced 2 Incontinence Intervoid Interval 1 Reduced Volume Voided per Micturition 1. Proven direct effect 2. Effect correlated with urgency but inconsistent due to multifactorial etiology of the symptom Chapple CR et al. BJU Int. 2004; 94:738-744. Prevalence of OAB by Gender in Korea The Overall Prevalence of OAB in Korea was 12.2% (10.0% Men and 14.3% Women) Prevalence,* % 25 Men Women 20 *For population 40+ years of age, OAB = 14.9% (male 11.2%; female 18.4%) 15 10 Estimation of people with OAB in Korea: 5,951,437 5 0 Korea Prevalence of OAB by Gender in Korea Total Men Prevalence of OAB, % 30 25 20 15 10 5 0 Age Group, years Women OAB Initiating Treatment • If there is no significant abnormality of physical exam, urine analysis and PVR, treatment for OAB can be initiated without further workup • In some cases where abnormalities are found, treatment can be initiated, but abnormality must be worked up (e.g. hematuria) – UDS in select patients Antimuscarinics 2008 in Korea • • • • • Oxybutynin IR Oxybutynin ER Tolterodine IR/ER Trospium Solifenacin BID-TID QD BID / QD BID / QD* QD What’s The Difference?? • Efficacy – No great differences – Dose dependent • Tolerability • Safety • Clinical Effectiveness – different for different patients depending on expectations Differences Among Anticholinergics • Metabolism – Hepatic – Renal • Pharmacokinetics Produce a number of – Delivery system clinically measurable and theoretical – Bioavailability differences • Receptor selectivity • Chemical structure – Permeability • Dose titration – 50-60% of patients will choose higher dose Why is Efficacy So Hard to Measure in the OAB Population • Different patients have different: – Primary bother symptoms – Expectations from treatment • Different studies have different populations Efficacy of Antimuscarinic Agents vs Placebo Frequency Drug % Frequency Placebo % Ratio UUI Drug % UUI Placebo % Ratio Tolterodine ER (4 mg)* 1 -22 -15 1.47 -71 -33 2.15 Oxybutynin ER (10 mg)** NA NA NA NA NA NA Oxybutynin TDS (3.9 mg)*2 -18 -8.7 2.07 -75 -50 1.5 Trospium (20 mg BID)** 3 Trospium (20 mg BID)** 4 -18.1 -20.5 -8.4 -13.5 2.15 1.52 -59 -63 -44 -43 1.34 1.47 Solifenacin (5 mg)** 5 Solifenacin (5 mg)** 6 -19.6 -17 -12.8 -8 1.53 2.12 -62.7 -65 -42.5 -40 1.48 1.63 Solifenacin (10 mg)** 5 Solifenacin (10 mg)** 6 -21.9 -20 -12.8 -8 1.71 2.5 -57.1 -63 -42.5 -40 1.34 1.58 Darifenacin (7.5 mg)* 7 -16.6 -9.1 1.82 -68.4 -53.8 1.27 Darifenacin (15 mg)* 7 -17.4 -9.9 1.76 -76.8 -58.3 1.31 *Median % change for baseline **Mean % change from baseline. Side Effects: Dry Mouth Incidence Oxybutynin ER 10mg Tolterodine ER 4mg Oxybutynin TDS Solifenicin 5 mg Solifenicin 10 mg Darifenicin 7.5 mg Darifenicin 15 mg Drug 28.1-29.7% 23% 9.6% 14% 21.3% 18.8% 31.3% Placebo n.a. 8% 8.3% 4.9% 4.9% 13.2% 13.2% Ratio 2.9 1.2 2.9 4.3 1.4 2.4 Side Effects: Constipation Incidence Oxybutynin ER 10mg Tolterodine ER 4mg Oxybutynin TDS Solifenicin 5mg Solifenicin 10 mg Darifenicin 7.5mg Darifenicin 15mg Drug 6.4-7.0% 6% <2% 7.2% 7.8% 14.8% 21.3% Placebo Ratio n.a. 4% 1.5 <2% ~1 1.9% 3.8 1.9% 4.1 6.7% 2.2 6.7% 3.2 Urgency: Defining Symptom of OAB • How is it measured? – Yes/no – Degree • VAS, IUSS, UPS – Warning time – OAB voids • Recent studies have shown positive effects on antimuscarinics on urgency – Darifenicin and solifenicin using yes/no scales – Tolterodine and trospium using fixed scales – Darifenicin using a VAS Reduction in Urgency Episodes/24 hrs Episodes 6.15 6.03 End of study mean: 2.24 3.30 Mean change from baseline to endpoint Mean baseline: 4 -3.91 63.6% -2.73 3 2 n=348 † 45.3% n=336 1 Solifenacin Placebo 0 P<0.0001 †Flexible dosing with solifenacin 5 or 10mg. Patients were allowed to dose increase at wk 4 and increase/decrease at wk 8 Serels S et al. Urology 2006; 68 (suppl 5a): 73 MP-04.11 Improvement in IUSS Score: Baseline to End of Study IUSS score Lower IUSS score indicates reduced urgency 2.4% 100 3 = Severe 90 2 = Moderate 18.7% 22.0% 80 1 = Mild 6.8% 18.6% 56.0% 70 Percent 0 = None 60 61.6% 67.8% 50 63.6% 40 50.2% 30 20 10 13.3% 0 Baseline 0.3% 12.0% End of Study Solifenacin Serels S et al. Urology 2006; 68 (suppl 5a):73 MP-04.11 19.5% Baseline 0.3% 5.9% End of Study Placebo Improvement in Urgency Perception Score: Baseline to End of Study 1 = Usually not able to hold urine 2 = Usually able to hold urine until I reach the toilet if I go immediately 3 = Usually able to finish what I am doing before going to the bathroom 100 90 15.1% 7.2% 15.2% 9.0% 80 Percent 70 46.7% 60 56.0% 68.4% 73.2% 50 40 30 46.1% 20 35.0% 10 0 16.4% 11.7% Baseline End of Study Solifenacin Baseline End of Study Placebo Higher UPS score indicates reduced urgency Serels S et al. Urology 2006; 68 (suppl 5a):73 MP-04.11 Tolterodine LA Nighttime Dosing Reduced 24-Hour Frequency Study 037 Placebo (n=421) Tolterodine LA (n=429) Total* Normal† OAB‡ Median Reduction in Micturitions, % 0 -10 -20 9.4 14.7 12.3 18.6 -30 11.5 18.1 -40 -50 P=.0068 P=.1571 P=.0012 -60 Micturition episodes defined as: *Urgency score of 1–5 on urgency scale †Urgency score of 1–2 on urgency scale ‡Urgency score of 3–5 on urgency scale P=.0225 Rackley et al. Urology. 2006;67:731-736. Individual Agents Advantages and Drawbacks Oxybutynin - ER • Advantages – Widest range of dose titration – Only compound approved for “high dose” administration • Drawbacks – Effects on cognitive function Tolterodine • Advantages – Long safety record – Number 1 prescribed drug – New CNS data favorable – Data on male OAB • Drawbacks: – Lack of titration – Mild increase in QT interval at super therapeutic doses Trospium • Advantages – No hepatic metabolism • Less drug-drug interactions – Less crossing of blood-brain barrier • ? Clinical correlation at this time – Higher urine concentration • ? Clinical meaning • Drawbacks BID dosing No dose titration Slight increase in heart rate Solifenicin • Advantages – Dose titration – Relatively low dry mouth incidence • Drawbacks – Mild increase in QT interval at super therapeutic doses Antimuscarinics Summary • Efficacy among antimuscarinic agents is similar • There are several different advantages (some theoretical) which may influence drug choice in a particular patient • Expect in cases of high dose antimuscarinics, decisions are more likely to revolve around tolerability and safety (or perceived safety) Male LUTS Can Be Associated With the Bladder, the Prostate, or Both Bladder Condition: OAB Urgency, with or without urgency incontinence, usually with frequency and nocturia Pharmacologic Therapy for OAB: Antimuscarinics BPH = benign prostatic hyperplasia; OAB = overactive bladder; 5-ARI = 5-alpha-reductase inhibitor. Prostate Condition: BPH Term used and reserved for the typical histological pattern that defines the disease Pharmacologic Therapy for BPH: alpha-Blockers 5-ARIs Abrams P et al. Urology. 2003;61:37-49. Timing of combination treatment • Primary vs. Add-on : Many patients with BPH and OAB have benefit from alpha blocker only : Initially treated with an alpha blocker : Anticholinergics is added in patients who report partial response to the alpha blocker but still have persistent OAB symptoms In Men With OAB, Treatment With Tolterodine Was Not Associated With Increased Incidence of AUR Subanalyses of Male Patients With OAB in Tolterodine ER Studies Withdrawal Because of Symptoms Suggestive of Urinary Retention, % (n/N) AUR, % Registration study (N = 163) Tolterodine ER* Placebo 1.3 (1/77) 0.0 (0/86) 0.0 0.0 Studies 037 and 041 (N = 745) Tolterodine ER* Placebo 0.8 (3/371) 0.5 (2/374) 0.0 0.0 IMPACT study† (N = 155) Tolterodine ER* 1.3 (2/155) 0.0 *Tolterodine ER 4 mg/d. †Open-label study. Roehrborn CG et al. BJU Int. 2006;97:1003-1006. Abrams P et al. J Urol. 2006;175:999-1004. Elinoff V et al. Intl J Clin Pract. 2006;60:745-751. TIMES Study : Urinary Retention Summary Placebo (n = 220) Tolterodine ER (n = 216) Tamsulosin (n = 215) Tolterodine ER/ Tamsulosin (n = 225) 4 4 0 2 Urinary retention 3 2 0 2 Urinary flow decreased 1 2 0 0 Discontinued due to AE 2 1 0 1 Catheterisation necessary (AUR) 0 1 0 1 Reported urinary AEs Kaplan SA et al. JAMA. 2006;296:2319-2328. Concerns about the risk of AUR • Several recent clinical trials have refuted • But, given the exclusion criteria should be considered • Exclusion criteria for PVR in clinical trials - greater than 30-40% of maximum capacity - or 50-200ml Concerns about the risk of AUR • Post-void residual volume should be measured to exclude baseline urinary retention • The safety in patients with baseline urinary retention is not known Recommendation Low PVR: <40% of functional capacity Jaffe WI, Te AE, Current Urology Reports 2005 Summary: OAB in Men • Available data suggests that antimuscarinics are safe in men with OAB + BOO, but PVR should be considered • Optimal way to use + alpha blockers needs to be sorted out • It should be evaluated which patient benefit from adding of antimuscarinics initially in real life practice