* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PowerPoint Presentation - No Slide Title
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Artificial heart valve wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
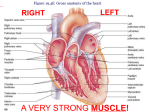
A. Includes a powerful pump (heart) and extensive system of tubes (blood vessels) B. Functions to transport oxygen, nutrients, and wastes. A. Size 1. Varies with body size average adult 9 cm x 14 cm B. Location 1. Nearly centered in the thoracic cavity, with the distal end toward the left side. C. Coverings of the heart Superior vena cava aorta Heart covered by visceral pericardium Right ventricle Left ventricle 1. Pericardium outer layer 2. Visceral pericardium (inner layer) 3. Parietal pericardium (middle layer) Pericardial cavity - serous fluid 1. Pericardium outer layer 2. Visceral pericardium (inner layer) 3. Parietal pericardium (middle layer) D. Wall of the Heart 1. endocardium a. serous membrane 2. myocardium a. thick cardiac muscle layer 3. epicardium a. epithelial and connective tissue b. specialized muscle fibers - Purkinje fibers E. Heart Chambers and Valves 1. chambers a. right atrium - receives returning blood from body b. right ventricle - pumps blood to lungs c. left atrium - receives blood from lungs d. left ventricle - pumps blood throughout body C C A A D D B B Interventricular septum 2. Valves = three cusps to valve = two cusps to valve a. tricuspid valve* - allows blood from right atrium to right ventricle b. pulmonary valve# - allows blood to leave right ventricle c. bicuspid (mitral) valve* - allows blood from left atrium to ventricle d. aortic valve# - prevents blood from flowing back into the left ventricle after contraction - located at base of aorta. *=AV valve #= semi lunar valve 3. Skeleton of heart a. connective tissue provide firm attachment points for valves, muscles Prevent atria & ventricles from dialating a. aorta & branches 4. Path of Blood Through the Heart e. b. capillary beds of all body tissues where gas exchange occurs d. f. c. a. c. superior and inferior vena cavae d. pulmonary arteries b. e. capillary beds of the lungs where gas exchange occurs f. pulmonary veins 5. Blood Supply to Heart a. coronary arteries i. Supply blood to heart tissue ii. Feed into many capillaries of myocardium iii. Small alternative branches (anastomoses) b. cardiac veins i. Drains blood to coronary sinus on hearts posterior surface - empties into right atrium A. Cardiac Cycle - (the coordinated contractions / relaxation of heart) 1. Atria - relaxed (atrial diastole) a. blood flows in b. pressure increases - A-V valves open blood flows into ventricle 2. Atria - contracted (atrial systole) a. atrial pressure rises - forcing remaining blood into ventricle 3. Ventricles contract (ventricular systole) a. A-V valve closes - partially extends into atrium b. papillary muscles contract pulling on chordae tendineae reducing valve extension back into atria. c. A-V valve remains closed as atria refills - pressure increases d. ventricle pressure increases opening semi-lunar valves e. Blood leaves ventricles 4. Ventricles relax (ventricular diastole) a. A-V valve opens blood flows into ventricle - atria pressure drops b. ventricle pressure low while filling - increases slightly with atria contraction c. semi-lunar valves close B. Heart Sounds 1. Lubb - first part - when ventricles contract A-V valves are closing 2. Dubb - second sound - when ventricles relax - semi-lunar valves close C. Cardiac muscle Fibers 1. Cardiac muscle fibers in branching networks a. stimulation to part - impulses to all - contracts as a unit i. unit is functional syncytium Atrial syncytium and ventricular syncytium Separated by fibrous skeleton D. Cardiac Conduction System 1. Sinoatrial node (S-A node) a. self initiating impulses travel to atrial syncytium b. right and left atria contract simultaneously c. impulse passes to atrioventricular node (A-V node) via junctional fibers (JF) 2. A-V node a. JF fibers small diameter conduct impulses slowly - delays impulse b. A-V node further slows impulse - allows for atrium to empty before ventricle contracts 3. A-V bundle - (bundle of His) a. from A-V node impulse travels along A-V bundle - through interventricular septum 4. Purkinje Fibers (PF) a. PF arise from A-V bundle b. spread into papillary muscles c. branch into small fibers contacting cardiac muscle fibers 5. Whorls of muscle fibers in ventricles contract in a twisting motion squeezing blood from ventricle E. Regualation of the Cardiac Cycle 1. Parasympathetic fibers contacting S-A, A-V node - continuous a. acetylcholine release decreases S-A and A-V node activity 2. Sympathetic fibers contact S-A, A-V nodes and other areas a. norepinephrine released - increases rate and force of contraction 3. Monitored by medulla oblongata (MO) a. Baroreceptors - monitor blood pressure i. Increase pressure - slows down heart rate (HR) b. Cerebrum and hypothalmus - influence MO c. Temperature i. Decrease - decrease HR d. Ions i. K+ - decrease HR ii. Ca+2 - increase HR S-A node Atrial syncytium Junctional fibers A-V node A-V bundle bundle branches Purkinje fibers Ventricular syncytium F. Electrocardiogram (ECG) or (EKG) 1. A recording of electrical changes in the myocardium during a cardiac cycle - (waves or deflections) 2. S-A node triggers - atrial fibers depolarize - P wave recorded 3. When ventricular fibers depolarize - QRS complex recorded a. Q wave Depolarization of ventricular fibers just prior to b. R wave contraction c. S wave 4. Ventricular fibers repolarizing produce T wave 5. repolarizing of atria mask by ventricle depolarizing A. Arteries 1. Elastic vessels - carry blood away from heart 2. Branch into smaller arterioles - capillaries 3. Structure a. three layers i. Tunica interna Endothelium cells smooth surface, ii. Tunica media Smooth muscle encircle tube. Elastic connective tissue iii. Tunica externa Connective tissue with elastic and collagenous fibers B. Capillaries 1. Smallest diameter BV 2. Connect arterioles with venules 3. Thin walls for O2, CO2, nutrient and waste exchange with blood 4. Density varies with need - muscles, endocrine glands, SI, increased numbers 5. Precapillary sphincters - open and close off capillaries as needed 6. Exchanges of substances a. diffusion - high to low concentration. b. filtration - high pressure in arteriole end of capillary forces out molecules c. osmosis - water tends to enter toward venous end of capillary. C. Veins 1. Return blood to heart 2. Smaller branches - venules 3. Three layer walls similar to arteries 4. Valves prevent back flow 5. Collapse when empty A. A measure of force exerted on inner walls of blood vessels. 1. Systolic pressure - high end of the measured pressures 2. Diastolic pressure - low end of measured pressures B. Factors influencing blood pressure (BP) 1. Heart action - (cardiac output) - determines how much blood enters arterial system. a. Cardiac output = stroke volume x heart rate. 2. Blood volume 3. Peripheral resistance - friction between blood and walls of blood vessels 4. Blood viscosity - ease at which fluid molecules move past one another C. BP control 1. Regulation of cardiac output and peripheral resistance