* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Magnetic resonance imaging for ischemic heart disease
Survey
Document related concepts
Cardiac contractility modulation wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Echocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Transcript
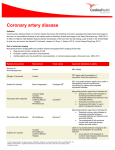
JOURNAL OF MAGNETIC RESONANCE IMAGING 26:3–13 (2007) Invited Review Magnetic Resonance Imaging for Ischemic Heart Disease Hajime Sakuma, MD* identification of subendocardial infarction with late gadolinium (Gd)-enhanced MRI. MRI is noninvasive and does not require injection of iodinated contrast medium, which is potentially nephrotoxic for patients with cardiovascular disease. In addition, MRI does not expose the patient to ionizing radiation. Therefore, cardiac MRI is suited for serial assessments of patients with heart disease. Recently, late Gd-enhanced MRI has been shown to be useful in detecting infarct tissue and in predicting myocardial viability and prognosis of the patients, and is routinely performed in many hospitals to evaluate patients with MI. Stress myocardial perfusion MRI and coronary MR angiography (MRA) are mainly performed by a growing number of early adopters at this point. While several important issues remain to be resolved, such as education and training for technologists and physicians, standardization of study protocols, and reimbursement for cardiac MRI, combined stress myocardial perfusion and late CE-MR studies will eventually play a central role in therapeutic decision-making for patients with ischemic heart disease. This article reviews recent advances in CE and non-CE cardiac MR applications from a clinical perspective in the areas of stress MR studies for detecting myocardial ischemia, MRI of MI and viability, coronary MRA, and MR assessment of coronary artery bypass graft. Cardiac MRI has long been recognized as an accurate and reliable means of evaluating cardiac anatomy and ventricular function. Considerable progress has been made in the field of cardiac MRI, and cardiac MRI can provide accurate evaluation of myocardial ischemia and infarction (MI). Late gadolinium (Gd)-enhanced MRI can clearly delineate subendocardial infarction, and the assessment of transmural extent of infarction on late enhanced MRI has been shown to be useful in predicting functional recovery of dysfunctional myocardium in patients after MI. Stress first-pass contrast-enhanced (CE) myocardial perfusion MRI can be used to detect subendocardial ischemia, and recent studies have demonstrated the high diagnostic accuracy of stress myocardial perfusion MRI for detecting significant coronary artery disease (CAD). Free-breathing, whole-heart coronary MR angiography (MRA) was recently introduced as a method that can provide visualization of all three major coronary arteries within a single three-dimensional (3D) acquisition. With further improvements in MRI techniques and the establishment of a standardized study protocol, cardiac MRI will play a pivotal role in managing patients with ischemic heart disease. Key Words: ischemic heart disease; coronary artery; myocardial infarction; myocardial ischemia; left ventricular wall motion J. Magn. Reson. Imaging 2007;26:3–13. © 2007 Wiley-Liss, Inc. MR Assessment of Cardiac Function ISCHEMIC HEART DISEASE is one of the leading causes of morbidity and mortality in many industrialized countries. Evaluation of ischemic heart disease requires measurement of regional and global ventricular function, identification of the presence and extent of myocardial ischemia, visualization of luminal narrowing of the coronary arteries, and assessment of myocardial infarction (MI) and viability. MRI has several important features for the assessment of ischemic heart disease. Cardiac MRI offers high spatial resolution, permitting direct visualization of subendocardial ischemia with stress first-pass contrast-enhanced (CE)-MRI and Cine MRI is now generally recognized as the most accurate and reproducible technique for assessing global ventricular function and left ventricular (LV) mass (1). The development of steady-state free precession (SSFP) sequences provided substantially improved blood–myocardial contrast on cine MR images in a reduced imaging time, allowing more accurate and reproducible delineation of the endocardial borders (2,3). Thus cine MRI is ideally suited for serial assessments of LV function in patients who have undergone therapeutic interventions. The sample size required to detect significant changes in clinical trials can be substantially reduced in comparison to other imaging modalities (4). In patients with impaired LV function after MI, the reliable differentiation of irreversibly damaged tissue and potentially salvageable viable myocardium is of major clinical importance. Cine MRI with SSFP sequences can provide accurate determination of regional LV wall thickness and systolic wall thickening in dys- Department of Diagnostic Radiology, Mie University Hospital, Mie, Japan. *Address reprint requests to: H.S., Department of Diagnostic Radiology, Mie University Hospital, 2-174 Edobashi, Tsu, Mie 514-8507, Japan. E-mail: [email protected] Received May 1, 2006; Accepted January 26, 2007. DOI 10.1002/jmri.20976 Published online in Wiley InterScience (www.interscience.wiley.com). © 2007 Wiley-Liss, Inc. 3 4 functional myocardial segments in patients with MI. However, rest cine MRI cannot distinguish between viable and nonviable myocardium, since both potentially viable and necrotic myocardia may demonstrate impaired regional myocardial contraction. Inotropic stimulation with low-dose (10 g/kg/minute) dobutamine infusion has been established as a reliable and safe means of predicting functional recovery of dysfunctional LV segments in patients with MI. Compared with echocardiography, MRI can be more suitable for predicting recovery of myocardial contraction because it is relatively independent of the operator’s skill, and the entire LV wall can be imaged with optimal imaging planes (5). Recent studies demonstrated that low-dose dobutamine stress cine MRI can provide more accurate prediction of functional recovery than late Gd-enhanced MRI in patients with MI (6,7). High-dose dobutamine stress (40 g/kg/minute) augments both myocardial contractility and the ratepressure product, thus increasing myocardial oxygen demand and causing ischemia in areas perfused by coronary arteries with flow-limiting stenoses. Highdose dobutamine stress echo has become a well-established modality for diagnosing myocardial ischemia. One of the limitations of stress echocardiography is that a substantial number of subjects yield suboptimal or nondiagnostic images. Stress-induced wall motion abnormalities can be detected with a significantly higher diagnostic accuracy by using dobutamine stress cine MRI compared to dobutamine stress echocardiography in patients with coronary artery disease (CAD). The sensitivity and specificity of high-dose dobutamine stress MRI for detecting significant CAD were reported to be respectively 83% and 83% by Hundley et al (8), and 86% and 86% by Nagel et al (9). The improved accuracy with stress MRI is generally explained by an improved delineation of the endocardial and epicardial borders, and superior quality of MR images in patients with obesity and pulmonary emphysema. High-dose dobutamine stress is superior to adenosine stress for detecting significant luminal narrowing in the coronary artery as a stress-induced wall motion abnormality (10). While adenosine induces myocardial blood flow inhomogeneities by vasodilation, and is useful for evaluating perfusion abnormality on first-pass CE-MRI, it does not induce increased oxygen demand because myocardial contraction is not augmented. In contrast, high-dose dobutamine stress can cause “true ischemia” due to increased myocardial contraction and oxygen demand. Complex intramyocardial contractile pattern can be evaluated by using a myocardial tagging technique. A radiofrequency (RF) prepulse labels the myocardium with dark grids, and enables detailed analysis of rotation, shortening, and strain of regional myocardium (11,12). Myocardial tagged MRI with strain quantification allows for more accurate assessment of regional wall motion abnormality compared to a wall-thickening analysis on cine MRI without tagging (13,14). A recent study by Bree et al (15) demonstrated that 3D strain analysis of low-dose dobutamine stress tagged MRI can provide precise identification, quantification, and display of regionally varying ventricular function in pa- Sakuma Figure 1. First-pass CE perfusion MR images with dipyridamole stress acquired with a saturation recovery GRE sequence with echo-planar readout in a patient with significant luminal narrowing in the left anterior descending artery (LAD). The hypoperfused region (arrows) in the anteroseptal wall is depicted as a region of lower enhancement. tients with ischemic cardiomyopathies. Fast harmonic phase (HARP) MRI combined with a rapid HARP postprocessing technique is one of the promising methods that permit rapid and operator-independent monitoring of strain abnormalities (16). Myocardial tissue tracking with two-dimensional (2D) cine displacement-encoded (DENSE) MRI is a new technique for quantitative motion tracking of the myocardium (17). Advantages of the DENSE approach include high spatial resolution of strain mapping and direct extraction of tissue displacement from phase-reconstructed images. Rest-Stress Perfusion MRI Accurate assessment of myocardial ischemia caused by flow-limiting stenosis in the coronary artery is important for evaluating patients with chest pain syndromes and in managing patients after therapeutic interventions. Dynamic MRI following a bolus injection of contrast material enables assessment of first-pass myocardial enhancement during pharmacological stress, which can provide information regarding the presence and the extent of CAD (Figs. 1 and 2). Rest-stress perfusion MR images are usually evaluated with semiquantitative approaches, such as an upslope analysis of myocardial time-intensity curve, or with a visual assessment. Myocardial blood flow in the resting state is not altered unless the luminal diameter stenosis in the epicardial coronary artery exceeds 90%, due to an autoregulation of coronary circulation that is regulated by the resistance in the arteriolar level. Vasodilator stress with adenosine or dipyridamole relaxes the arteriolar tonus and induces a perceptible difference in perfusion between normal and ischemic myocardia (18). Inotropic stress with high-dose dobutamine is widely employed in stress function studies and theoretically can be useful for inducing myocardial ischemia in stress perfusion MRI for Ischemic Heart Disease Figure 2. First-pass CE perfusion MR images with dipyridamole stress acquired with a saturation recovery GRE sequence with echo-planar readout in a patient with triple vessel disease before (a) and after (b) coronary artery bypass graft surgery. Subendocardial hypoenhancement encompassing the entire circumference of the LV myocardium is observed before bypass graft surgery, which is markedly improved after successful bypass grafting. MR studies. However, high-dose dobutamine stress is not usually used for rest-stress perfusion MRI, because increased heart rate induced by high-dose dobutamine leads to substantial motion artifacts and image degradation on perfusion MR images. Currently, no consensus has been established regarding the optimum dose of Gd MR contrast medium for stress perfusion MRI. A lower dose of the contrast medium (0.025– 0.05 mmol/ kg) is preferable to maintain the linear relationship between blood Gd concentration and MR signal intensity that is critical for quantitative assessment of myocardial perfusion. Administration of a higher dose (0.075– 0.1 mmol/kg) is beneficial to achieve an increased myocardial enhancement and a better contrast between normal and ischemic myocardium. A dual-bolus administration of Gd contrast medium (0.0025 mmol/kg followed by 0.1 mmol/kg) is an approach that enables quantitative assessment of myocardial perfusion while maintaining excellent contrast enhancement in the myocardium (19). Myocardial perfusion MR sequences need to satisfy several conflicting requirements, including high spatial resolution, high temporal resolution, sufficient coverage of LV myocardium, high contrast-tonoise ratio (CNR), and reduced artifacts. Saturation recovery fast gradient-echo (GRE) sequences and hybrid echo-planar sequences have been widely used in perfusion MR studies (20). Recently, saturation recovery SSFP sequences were introduced as a method that can provide improved signal-to-noise ratio (SNR) (21). However, the sequence of choice for perfusion MRI has not been determined at this point, and the image quality of saturation recovery myocardial perfusion MR images generally needs further improvements. Suppression of a dark artifact in the subendocardium, which is most apparent during first-pass transit of MR contrast medium through the LV cavity, is particularly important because it may mimic the subendocardial perfusion abnormalities observed in CAD. This artifact is primarily caused by Gibbs ringing and cardiac motion during image data acquisition. Improved spatial resolution of perfusion MR images, and shorter acquisition times per image to reduce motion artifacts seem to be important to reduce the artifact. A comparison of rest and stress 5 perfusion MR images is sometimes useful to distinguish stress-induced subendocardial hypoperfusion from a dark subendocardial artifact. Recent studies demonstrated that first-pass perfusion MRI with pharmacological stress allows the detection of hemodynamically significant CAD with high diagnostic accuracy. Schwitter et al (22) obtained stress perfusion MR images in 48 patients and 18 healthy volunteers by using a multislice hybrid echo-planar MR pulse sequence. Stress perfusion MRI showed a sensitivity of 91% and specificity of 94% for detecting CAD as defined by positron emission tomography (PET), and a sensitivity of 87% and specificity of 85% in comparison with quantitative coronary angiography. In a more recent study, Nagel et al (23) obtained first-pass CE MR images in 84 patients by using a fast GRE/echo-planar hybrid sequence. By assessing myocardial perfusion reserve index, MRI yielded a sensitivity of 88%, specificity of 90%, and accuracy of 89%. In a multicenter dose-range study reported by Wolff et al (24), the highest area under the receiver operating characteristics (ROC) curve of 0.90 ⫾ 0.04 was obtained at a relatively low injection dose of 0.05 mmol/kg. The sensitivity, specificity, and accuracy of stress perfusion MRI with this dose were 93%, 75%, and 85%, respectively. Atherosclerosis in multiple vascular areas is a major problem in the care of patients with vascular diseases, and significant CAD was found in approximately 31% to 53% of patients with aortic aneurysms. The use of routine coronary angiography in all patients with aortic diseases, however, may increase unnecessary risk and costs. A recent study by Ishida et al (25) demonstrated that stress CE-MRI is useful for noninvasive detection of CAD in patients prior to elective repair of aortic aneurysms. The overall sensitivity, specificity, and accuracy of combined stress perfusion MRI and late Gdenhanced MRI for detecting patients with significant CAD were 88%, 87%, and 88%, respectively. Stress myocardial perfusion single-photon emission computed tomography (SPECT) has been widely used to demonstrate reduced regional myocardial perfusion in patients with CAD. First-pass MR perfusion assessment has several potential advantages over nuclear medicine techniques in terms of good spatial resolution, no ionizing radiation, and no attenuation or scatter artifacts. The improved spatial resolution of MRI permits the detection of small subendocardial ischemia in patients with mild to moderate CAD, and the delineation of diffuse subendocardial hypoenhancement in patients with multivessel CAD. In a study that directly compared stress perfusion MRI and stress SPECT, the diagnostic accuracy of stress perfusion MRI was significantly better than that of stress SPECT when results from quantitative coronary angiography were used as the reference standard (26). In another recent study, the areas under the ROC curve for detection of significant coronary stenosis was 0.84 – 0.86 for stress perfusion MRI and 0.72-0.79 for stress 201Tl SPECT (27). Viability Assessment With Late Gd-Enhanced MRI Assessment of myocardial viability is important in the prediction of functional recovery after revascularization 6 Sakuma Figure 3. Late CE-MR images from a patient with old MI acquired with an IR 3D turbo-field-echo (TFE) sequence using sensitivity encoding (SENSE). a: Short-axis image. b: Vertical long-axis image. c: Four-chamber view. Late Gd-enhanced MR images show transmural high signal intensity in the anteroseptal wall and apex. No myocardial viability was preserved in the infarcted area. and in the risk stratification of patients with CAD. Myocardial viability has several different definitions, including functional viability that can be assessed by monitoring responses to dobutamine stress using echocardiography or cine MRI, cellular viability indicated by Tl-201 SPECT as a preserved intracellular fraction, metabolic viability assessed by FDG (fluorodeoxyglucose) PET as preserved glucose metabolism, and histological viability determined by late Gd-enhanced MRI. Among these definitions, the one closely related to histology seems to be the most definite criterion for determining whether a myocardial cell is alive or not. Myocardial uptake of Tl-201 on SPECT does indicate the presence of viable myocardial cells, since there is an apparent similarity between the transport of ionic thallium and potassium through myocardial cell membranes. However, spatial resolution of SPECT is limited, and Tl-201 uptake in viable myocardium can be substantially influenced by myocardial blood flow as well. Late Gd-enhanced MRI of the myocardium has become increasingly important as a noninvasive MR method for demonstrating MI and assessing myocardial viability. CE-MRI has high spatial resolution and can clearly demarcate infarcted tissue and viable myocardium within the LV wall. An animal study demonstrated that the spatial extent of enhancement on late Gd-enhanced MRI showed a good agreement with that of MI defined by TTC (triphenyl-tetrazolium chloride)-stained slices in both acute and chronic states (28). Late CE-MR images were acquired 10 –15 minutes after contrast injection (29). In the equilibrium phase, Gd contrast medium nonspecifically distributes in the extracellular space that constitutes about 20% of water fraction in normal myocardial tissue. In infarcted tissue, however, the distribution volume of extracellular contrast medium is substantially increased due to loss of intracellular fraction of myocardium (30), resulting in enhancement of MI on inversion recovery (IR)-prepared MR images (Fig. 3). Typically a patient is given a 0.1– 0.2-mmol/kg intravenous administration of extracellular Gd contrast medium, and images are acquired with IR GRE sequences (29). The inversion time (TI) needs to be adapted individually for each examination to null the signal of the normal myocardium in order to ensure an optimal contrast between infarction and viable myocardium. The Look-Locker pulse sequence acquires multiple GRE MR images at different TI values after the IR pulse, which is useful for determining an optimal TI value for late Gd-enhanced MR images (31). Phasesensitive image reconstruction allows the use of a nominal TI value and eliminates the precise adjustment of TI in each patient (32–33). With two-dimensional (2D) IR GRE sequences, repeated breath-holds are required to cover the entire LV for a comprehensive evaluation of myocardial viability of the heart. This procedure is time-consuming and difficult for some patients with advanced heart failure. The three-dimensional (3D) IR GRE sequence allows rapid and complete acquisition of 3D images and covers the LV within one breath-hold. The CNR of late Gd-enhanced MR images was found to be threefold larger with the 3D sequence than with the 2D sequence (24). A high level of agreement was found between 2D and 3D sequences for evaluating the presence of MI, while the transmural extent of enhancement can be overestimated with the 3D sequence if the spatial resolution is not sufficient without using parallel imaging acquisition. Late Gd-enhanced MR images have been assessed by measuring the transmural extent of infarction for predicting recovery of impaired contractile function in patients after MI. In a study that evaluated 50 chronic patients with ventricular dysfunction before revascularization, the likelihood of improvement in regional contractility after revascularization negatively correlated with the transmural extent of enhancement (35). The contractility improved by revascularization in 78% of dysfunctional segments without enhancement, but the improvement was found in only 2% of the segments that exhibited transmural extent of more than 75%. The transmural extent of infarction on late CE-MR images can predict improvement in contractile function in patients with acute MI as well. Choi et al (36) studied 24 patients who presented with their first MI and underwent successful revascularization. The percentage of segments that showed improvement in contractile function eight to 12 weeks later progressively reduced MRI for Ischemic Heart Disease Figure 4. A patient with inferior MI six days after onset. Balanced TFE cine MR images in the diastole (a) and systole (b) demonstrate mild hypokinesis in the inferior wall. c: T2weighted black-blood FSE MR image exhibits transmural high intensity in the inferior wall, indicating myocardial edema. d: 3D late CE-MR image reveals subendocardial MI in the inferior wall with preserved non-necrotic myocardium in the epicardial side of the LV wall. Notice that the area showing edema is substantially larger than infarcted myocardium on the late CE-MR image. as the transmural extent of infarction increased. The percentage of the segments that showed recovery was 77% for the segments without infarction, 67% for the segments with 1% to 25% transmural extent, 56% with 26% to 50% transmural extent, 35% with 51% to 75% transmural extent, and 5% with 76% to 100% transmural extent in their study. Differentiation between acute and chronic MI is a frequent demand for clinical decision-making in patients with MI, but both acute and chronic MI exhibit late enhancement regardless of their age. T2-weighted MRI depicts infarct-related myocardial edema as a marker of acute MI, and is useful for differentiating acute from chronic MI (37) (Fig. 4). In addition to the patients with a diagnosis of MI, late Gd-enhanced MRI is of great value for classifying patients with heart failure in relation to the presence or absence of underlying CAD. Soriano et al (38) reported that 81% of the patients with coronary arterial stenoses on X-ray coronary angiography showed subendocardial and/or transmural enhancement, whereas only 9% of an angiographically negative group demonstrated late enhancement. Thus late CE-MRI offers a valid alternative to X-ray coronary angiography for the detection of CAD in patients with heart failure. First-pass CE-MRI in the resting state has been shown to be useful in predicting functional recovery in patients with acute MI. An area of perfusion defect on first-pass CE-MR images, which is related to “microvascular obstruction” or “no reflow,” indicates greater myocardial damage, and poor functional recovery and prognosis (39). Gerber et al (40) evaluated the diagnostic accuracies of first-pass CE-MRI and late CE-MRI in 7 predicting functional improvement in patients with acute MI. The presence of early hypoenhancement had a high positive predictive value of 68% and a high specificity of 89% for predicting persistent dysfunction. However, the absence of early hypoenhancement had a low specificity of 19%, resulting in a limited accuracy of 49%. Late Gd-enhanced MRI demonstrated a sensitivity of 82%, specificity of 64%, and accuracy of 74%, and they concluded that lack of late enhancement has better diagnostic accuracy for predicting functional improvement in dysfunctional segments in acute MI (Fig. 5). Myocardial perfusion SPECT is an established procedure for diagnosing infarction. However, subendocardial MI is frequently missed by SPECT. In a study done by Wager et al (41), late CE-MRI identified 92% of the segments with subendocardial infarction in animal models, whereas SPECT detected only 28%. A reason for this poor sensitivity is that the spatial resolution of SPECT images is nearly comparable to the entire thickness of LV wall. In contrast, MRI typically yields 5–10 pixels within the LV wall, which makes it possible to reliably detect subendocardial infarction. In a study by another group (42), the diagnostic accuracy of late CEMRI and rest Tl-201 SPECT were compared in the prediction of functional recovery of regional myocardial contraction in patients after acute MI. The sensitivity, specificity, and accuracy of late CE-MRI in the prediction of functional recovery were significantly higher compared to Tl-201 SPECT. In addition, because of the high negative predictive value of late enhanced MRI (92.7%) as compared to Tl-201 SPECT (66.1%), segments with a low likelihood of recovery can be identified with high confidence by using CE-MRI instead of SPECT. The false-negative segments on Tl-201 SPECT images were frequently found in the inferior wall, in 14 of 19 segments (74%), which is most likely related to Figure 5. Late CE-MR images from a patient with acute inferior MI acquired with an IR 3D TFE sequence using SENSE. MR images were obtained six days after onset of MI. Late Gd-enhanced MR images show high signal intensity in the posterior wall extending to the epicardial border of the LV wall. Non-enhanced tissue is observed in the subendocardial side of this transmural infarction, indicating the presence of microvascular obstruction. 8 attenuation artifacts on SPECT. These results indicate that late CE-MRI can substitute for 201Tl SPECT in evaluating patients with MI. Infarct size on late Gd-enhanced MRI in patients with acute MI appears to diminish on follow-up CE-MRI (43). In a recent study that assessed changes in enhanced tissue and non-enhanced myocardium from acute to chronic states (44), the total volume of abnormally enhanced tissue was significantly reduced by approximately 32%. Segmental analyses revealed that the mean thickness of enhanced tissue in the infarct segments decreased by 30%, and the mean thickness of non-enhanced myocardium in the infarct segments increased by 27%. As mentioned previously, viable myocardium with preserved intracellular space is shown as non-enhanced myocardium on late enhanced MR images. Thus, regional myocardial viability can be assessed by measuring the amount of non-enhanced tissue rather than the transmural extent of necrotic tissue. One study indicated that the diagnostic performance of late enhanced MRI for predicting normal contractile function in the chronic state can be improved by measuring the thickness of non-enhanced myocardium instead of measuring the transmural extent in patients with acute MI (44). Coronary MRA Catheter X-ray coronary angiography has been used as the gold standard for identifying CAD. However, this method entails small but definable risks (45), and a considerable number of patients undergoing elective X-ray coronary angiography are found to have no significant CAD. CE multislice CT has rapidly emerged as a noninvasive method that can provide reliable detection of the CAD (46). In a recent work by Mollet et al (46), the estimated radiation dose during 64-slice CT coronary angiography (15.2 and 21.4 mSv for men and women, respectively) was higher than the radiation dose associated with conventional coronary angiography. While coronary MRA does not expose the patients to radiation, noninvasive MRI of the coronary artery is technically demanding due to the small size and tortuous course of the coronary arteries and their complex motion caused by cardiac contraction and respiration. In the past few years the image quality, volume coverage, acquisition speed, and arterial contrast of 3D coronary MRA have been substantially improved with the use of SSFP sequences and parallel imaging techniques, permitting the acquisition of high-quality 3D MR angiograms encompassing the entire coronary arteries within a reasonably short imaging time. Breath-hold 3D coronary MRA has advantages in terms of time efficiency compared to free-breathing 3D coronary MRA (47). In a study reported by van Guens et al (48), 69% segments were assessable by breath-hold 3D coronary MRA with a volume-targeted imaging approach, with a sensitivity and specificity for detecting ⬎50% luminal stenoses of 92% and 68%. Another benefit of breath-hold 3D coronary MRA is that this method can utilize first-pass contrast enhancement of the coronary arteries following an intravenous injection of conventional extracellular MR contrast medium. Regenfus Sakuma et al (49) obtained breath-hold 3D coronary MRA in 50 patients by injecting extracellular MR contrast medium at a flow rate of 1 mL/second. The sensitivity and specificity of this approach were 94% and 57%, respectively, for detecting patients with significant CAD. Breath-hold 3D coronary MRA has several important limitations. A short imaging time is achieved at the expense of spatial resolution and 3D volume coverage, and patients with heart or pulmonary disease cannot hold their breath for a long time. Another limitation is that breath-holding does not completely eliminate respiratory blurring of the coronary artery on 3D MRA, as a continued drift of the diaphragm position was observed during breathholding (50). Free-breathing, respiratory-gated 3D coronary MRA is currently the most commonly used MR approach for assessing coronary arteries in patients with heart disease. In a multicenter study reported by Kim in 2001 (51), free-breathing 3D coronary MR angiograms were obtained with a double oblique targeted volume method and 3D GRE sequence. The sensitivity and specificity were respectively 93% and 42% for identifying patients having significant CAD, and 100% and 85% for detecting patients with left main CAD and triple vessel disease. Reliable detection of CAD beyond the left main coronary artery and proximal coronary arteries necessitates further improvements in MRI sequences. With the introduction of SSFP sequences, the blood signal intensity on 3D coronary MRA is considerably augmented without the use of MR contrast medium in comparison to 3D GRE sequence (52). In a study done by Spuentrup et al (46), radial k-space sampling was shown to be useful for reducing motion artifacts and improving vessel sharpness on steady-state 3D coronary MRA (53). Jahnke et al (54) compared the diagnostic performances of breath-hold 3D coronary MRA and free-breathing 3D coronary MRA by utilizing the same SSFP sequence. Free-breathing coronary MRA was superior to breath-hold coronary MRA in terms of both image quality and diagnostic accuracy, with an overall sensitivity and specificity of 72% and 92% for the freebreathing approach, and 63% and 82% for the breathhold approach. Kefer et al (55) compared the diagnostic accuracy of free-breathing 3D coronary MRA using an SSFP sequence with that of 16-slice multislice CT in 42 patients. By using quantitative coronary angiography as a gold standard, the sensitivity and specificity of coronary MRA for the detection of luminal narrowing were 75% and 77%, respectively. These MR results were similar to the sensitivity (82%, P ⫽ n.s.) and specificity (79%, P ⫽ n.s.) of 16-slice multislice CT. SSFP sequences permit the acquisition of a 3D axial volume that encompasses the entire heart without losing arterial contrast, because signal intensity on steady-state 3D coronary MRA is primarily determined by the T2/T1 ratio, instead of the in-flow effect of the blood (56 –58) (Figs. 6 and 7). By using the whole-heart approach, one can visualize all three major coronary arteries with a reduced total examination time in comparison to targeted double oblique 3D GRE MRA. In addition, planning of whole-heart coronary MRA becomes quite simple, eliminating the time-consuming three-point planning required for the targeted double oblique approach. Coronary MRA acquired with this MRI for Ischemic Heart Disease Figure 6. Whole-heart coronary MRA acquired with a freebreathing SSFP sequence in a subject with normal coronary arteries. The volume-rendered image from whole-heart coronary MRA is useful for 3D anatomical recognition of the RCA and the LAD and its branches. approach is useful in the evaluation of the luminal narrowing of the coronary artery that exhibits heavy calcification in the vessel wall on multislice CT (Fig. 8). A recent study demonstrated that acquisition of wholeheart coronary MRA was successful in 34 of 39 patients (87.2%), with an average acquisition duration of 13.8 ⫾ 3.8 minutes (58). In that study, a trigger delay time and an interval of minimal motion of the right coronary artery (RCA) were determined on cine MR images for the subsequent whole-heart coronary MRA acquisition. The use of a subject-specific acquisition window (59) is important to reduce motion blurring of the coronary artery on whole-heart coronary MRA. In a more recent study evaluating 113 patients (60), whole-heart coronary MRA allowed for the noninvasive detection of significant narrowing in coronary arterial segments with a diameter of 2 mm or greater, with moderate sensitivity of 82% and high specificity of 90% in a patient-based analysis. In a vessel-based analysis, the sensitivity was 85% for the RCA, 77% for the anterior descending artery, and 70% for the circumflex artery. However, MR acquisition was not successful in approximately 14% of the patients who demonstrated an unstable breathing Figure 7. Reformatted whole-heart coronary MRA in a subject with normal coronary arteries. a: Curved MPR (multiplanar reformation) image clearly depicts the RCA and left circumflex (LCX) arteries. b: Oblique axial curved multiplanar reformatted image visualizes the left main coronary artery, LAD, proximal RCA, and LCX arteries. 9 Figure 8. A 61-year-old-male with chest pain on effort. a: A curved MPR image of CE-CT coronary angiography acquired with a 64-slice scanner demonstrates heavy calcification of the arterial wall in the proximal LAD, which makes it difficult to evaluate luminal narrowing of the coronary artery. b: A curved MPR image of free-breathing 3D whole-heart coronary MRA clearly reveals luminal narrowing in the proximal LAD. pattern or drift of the diaphragm position during the scan. A low navigator efficiency of less than 20% generally indicated unsuccessful acquisition of freebreathing coronary MRA. Coronary MRA has been shown to have high sensitivity and specificity for detecting anomalous coronary arteries and delineating proximal courses of the vessels (61). It should be also noted that anomalous coronary arteries can be accurately assessed by CE multislice CT as well (62). Coronary MRA provides noninvasive detection and size measurement of coronary artery aneurysms in patients with Kawasaki disease, and can be used as an alternative imaging method when the image quality of transthoracic echocardiography is insufficient (63). Coronary MRA and X-ray coronary angiography show excellent agreement in the diagnosis of coronary artery aneurysm, and also in the measurements of the maximal diameter and length of the aneurysm (64). Noninvasive visualization of the coronary vessel wall may enhance risk stratification by quantifying subclinical coronary atherosclerotic plaque burden. However, MR visualization of coronary atherosclerotic plaque is highly challenging because it is much thinner than carotid plaque and exhibits complex motion due to respiration and cardiac contraction. Fayad et al (65) initially demonstrated the feasibility of plaque MRI of the human coronary arteries by using breath-hold 2D black-blood fast spin-echo (FSE) MRI. The free-breathing black-blood spiral MR approach proposed by Kim et al (66) allows for isotropic 3D visualization of the coronary vessel wall. Recently there has been increasing interest in molecular MRI with tissue-targeted contrast-agents. Spuentrup et al (67) demonstrated that fibrin-targeted contrast medium permits selective visualization of acute thrombi in the coronary and pulmonary arteries. MRI of coronary thrombosis with tissuetargeted contrast medium may be an ideal noninvasive imaging approach for the visualization of thrombi associated with plaque rupture. 10 There is an increasing interest in high-field coronary MRI because the SNR increases approximately linearly with field strength, and improvement in the SNR is expected with 3.0T MR imagers. Stuber et al (68) demonstrated the feasibility of coronary MRA using a 3.0T MR imager in healthy volunteers. Coronary MR angiograms with submillimeter spatial resolution were demonstrated at 3.0T. Sommer et al (69) evaluated the feasibility, image quality, and accuracy of coronary MRA at 3.0T in patients with suspected CAD. The average increase in CNR at 3.0T with respect to 1.5T was 21.8% for the left coronary artery (LCA) and 23.5% for the RCA. However, coronary MRA at 3.0T did not result in significant improvement in the overall image quality score by visual assessment, and no significant difference was observed in the diagnostic accuracy between 1.5T and 3T. Susceptibility-related local magnetic field variations, increased sensitivity to motion artifacts, and impaired ECG R-wave triggering are cited as factors related to increased artifacts at 3.0T. Another major limitation of 3.0T for cardiac MRI is RF-induced heating. With further advances in hardware and optimization of pulse sequences for high-field cardiac MRI, the 3.0T MR imager might become a platform of choice for high-resolution coronary MRA and vessel wall imaging. MR of Coronary Artery Bypass Graft The assessment of occlusion and stenosis of coronary artery bypass grafts is required postoperatively in many circumstances. While the patency and stenosis of coronary artery bypass grafts can be assessed reliably with conventional X-ray angiography, this technique is invasive and involves some risk. MRI has been shown to be useful for demonstrating the occlusion of coronary artery bypass graft with the use of spin-echo MRI (sensitivity/specificity of 90%/72%) (70), cine MRI (88%/ 100%) (71), and CE 3D MRA (95%/81%) (72). Recently Bunce et al (72) evaluated the accuracy of SSFP multislice MR images and CE 3D MRA for the detection of coronary artery bypass patency in 25 patients. Although the sensitivity values of steady-state MRA and CE-MRA were similar (84% vs. 85%), SSFP MRI resulted in more false-positive findings for occlusions and reduced visualization of the arterial grafts. In addition to the detection of graft occlusion, noninvasive identification of graft stenoses is important for evaluating patients who present with chest pain after bypass graft surgery. Langeral et al (74) evaluated the accuracy of high-resolution navigator-gated 3D MRA for detecting vein graft disease. The averaged sensitivity and specificity for identifying graft occlusion, graft stenosis ⱖ 50%, and graft stenosis ⱖ 70% were 83/99%, 74/85%, and 73/84%, respectively, indicating that high-resolution free-breathing 3D MRA enables the assessment of vein graft stenoses with a fair diagnostic accuracy. MR Flow Measurement in Coronary Circulation Phase-contrast cine MRI can provide flow quantification in the coronary artery bypass graft and native coronary artery. MR flow measurement in coronary artery Sakuma bypass graft was validated with Doppler flow measurement using a flow phantom by Langerak et al (75). Excellent correlations in average peak velocity (r ⫽ 0.99, P ⬍ .001) and diastolic peak velocity (r ⫽ 0.99, P ⬍ .001) were demonstrated in vitro between MR and Doppler flow measurements, with less than 5% interstudy variability. In order to validate the accuracy of MR flow quantification of the coronary artery bypass grafts in patients, the maximal diastolic blood flow velocity in the bypass graft was compared with the diastolic peak velocity measured by using a Doppler guidewire (76). The diastolic peak velocity measured with MRI showed a significant linear correlation with the diastolic peak velocity obtained by using the Doppler guidewire, with a correlation coefficient of 0.78 and slope of 0.85 (P ⬍ .05). One study evaluated the diagnostic value of breath-hold MR flow measurement for detecting significant stenosis in the internal mammary artery to the coronary artery bypass conduit, with conventional Xray angiography used as the reference standard (75). The mean diastolic-to-systolic peak velocity ratio (0.61 ⫾ 0.44 ) and the mean blood flow (16.9 mL/ minute ⫾ 5.5) in the subjects with graft stenoses were significantly lower than in those without stenoses (1.88 ⫾ 0.96, P ⬍ 0.01 and 79.8 mL/minute ⫾ 38.2, P ⬍ 0.01), and the authors concluded that MR blood flow measurement in the baseline state is useful for predicting significant stenosis in the internal mammary arterial graft. The value of MR measurements of graft flow and flow reserve in differentiating significant from nonsignificant vein graft disease was evaluated by Bedaux et al (77). By combining basal volume flow ⬍20 mL/ minute and graft flow reserve ⬍2, MR flow measurements showed a sensitivity of 78% and specificity of 80% for detecting grafts with significant stenosis or impaired run-off . In a study recently reported by Salm et al (78), a head-to-head comparison between SPECT perfusion imaging and MR determined flow velocity reserve was performed for the detection of significant angiographic lesions in bypass grafts. Excellent agreement was found between SPECT and MR flow velocity reserve measurement in 80% of all grafts. When the grafts that perfused a territory with myocardial scar were excluded, the agreement between SPECT and MR improved to 84%. They also reported that MR flow velocity mapping can provide excellent detection of graft stenoses by measuring either volume flow or flow velocity, with a sensitivity of 92% and 93%, respectively (79). MR flow quantification can be used for the functional assessment of native coronary arteries (80,81). Serial changes in the coronary flow velocity reserve were evaluated for noninvasive detection of restenosis after coronary stent implantation by using fast phase-contrast cine MRI (82). A significant reduction of MR-determined coronary flow velocity reserve in the arterial lumen distal to the stent was observed in patients with restenosis. The flow velocity reserve was 2.26 ⫾ 0.49 at one month and 1.52 ⫾ 0.09 (P ⬍ 0.05) at six months after stent implantation in subjects with restenosis. In a recent study by Nagel et al (83), coronary flow velocity reserve in the artery distal to the stent was measured with MR in 38 patients after successful stent placements. Using a threshold of 1.2 for MR flow velocity MRI for Ischemic Heart Disease reserve, a sensitivity of 83% and a specificity of 94% were achieved for detecting ⱖ75% stenoses on coronary angiography. CONCLUSIONS With recent technical advances and an increasing number of publications, cardiac MRI is now recognized as a method that can provide valuable information that may not be obtained from other diagnostic modalities, such as echocardiography and nuclear cardiology, in patients with ischemic heart disease. The high spatial resolution of MRI can distinguish transmural from subendocardial ischemia or infarction. Cardiac MRI is noninvasive and does not require the use of potentially nephrotoxic iodinated contrast agents or radiation. However, MRI has a substantial functional overlap with echocardiography, nuclear SPECT imaging, and multislice CT. For example, stress myocardial perfusion MRI is not the only alternative approach to stress myocardial perfusion SPECT for the detection of myocardial perfusion abnormalities in CAD. A multicenter study by Jeetley et al (84) demonstrated that myocardial contrast echocardiography with vasodilator stress is comparable to stress SPECT in the detection of CAD. George et al (85) recently determined the accuracy of multislice CT to measure differences in regional myocardial perfusion during stress in a canine model of coronary artery stenosis, and found that stress myocardial perfusion CT provides semiquantitative measurements of altered myocardial perfusion. There are several important points that currently influence the expansion of cardiac MRI in clinical practice. The acquisition of cardiac MR images is time-consuming and the patient throughput with MR is substantially lower compared to multislice CT. Acquisition techniques for cardiac MRI are still complicated, and a relatively small number of institutions perform cardiac MRI on a day-to-day basis, which has limited recognition of the usefulness of MRI by physicians. Other factors that considerably affect the expansion of cardiac MRI are the limited availability of MR imagers and insufficient reimbursement. Most importantly, administration of Gd contrast medium in cardiac MRI has been considered off-label use in the United States. Practical education and training for physicians and technologists, standardization of MRI protocols, cost-effectiveness studies to improve reimbursement, and efforts to raise awareness of the value of cardiac MRI among clinicians and the general public seem to be essential for expanding the use of cardiac MRI in clinical practice. 11 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. REFERENCES 1. Grothues F, Smith GC, Moon JC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol 2002;90:29 –34. 2. Moon JC, Lorenz CH, Francis JM, Smith GC, Pennell DJ. Breathhold FLASH and FISP cardiovascular MR imaging: left ventricular volume differences and reproducibility. Radiology 2002;223:789 – 797. 3. Ichikawa Y, Sakuma H, Kitagawa K, et al. Evaluation of left ventricular volumes and ejection fraction using fast steady-state cine 21. 22. 23. MR imaging: comparison with left ventricular angiography. J Cardiovasc Magn Reson 2003;5:333–342. Bellenger NG, Davies LC, Francis JM, Coats AJ, Pennell DJ. Reduction in sample size for studies of remodeling in heart failure by the use of cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2000;2:271–278. Baer FM, Theissen P, Schneider CA, et al. Dobutamine magnetic resonance imaging predicts contractile recovery of chronically dysfunctional myocardium after successful revascularization. J Am Coll Cardiol 1998;31:1040 –1048. Motoyasu M, Sakuma H, Ichikawa Y, et al. Prediction of regional functional recovery after acute myocardial infarction with low dose dobutamine stress cine MR imaging and contrast enhanced MR imaging. J Cardiovasc Magn Reson 2003;5:563–574. Wellnhofer E, Olariu A, Klein C, et al. Magnetic resonance low-dose dobutamine test is superior to SCAR quantification for the prediction of functional recovery. Circulation 2004;109:2172–2174. Hundley WG, Hamilton CA, Thomas MS, et al. Utility of fast cine magnetic resonance imaging and display for the detection of myocardial ischemia in patients not well suited for second harmonic stress echocardiography. Circulation 1999;100:1697–1702. Nagel E, Lehmkuhl HB, Bocksch W, et al. Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of highdose dobutamine stress MRI: comparison with dobutamine stress echocardiography. Circulation 1999;99:763–770. Paetsch I, Jahnke C, Wahl A, et al. Comparison of dobutamine stress magnetic resonance, adenosine stress magnetic resonance, and adenosine stress magnetic resonance perfusion. Circulation 2004;110:835– 842. Axel L, Dougherty L. Heart wall motion: improved method of spatial modulation of magnetization for MR imaging. Radiology 1989;172: 349 –350. Zerhouni EA, Parish DM, Rogers WJ, Yang A, Shapiro EP. Human heart: tagging with MR imaging: a method for noninvasive assessment of myocardial motion. Radiology 1988;169:59 – 63. Gotte MJ, van Rossum AC, Twisk JWR, Kuijer JPA, Marcus JT, Visser CA. Quantification of regional contractile function after infarction: strain analysis superior to wall thickening analysis in discriminating infarct from remote myocardium. J Am Coll Cardiol 2001;37:808 – 817. Kuijpers D, Ho KY, van Dijkman PR, Vliegenthart R, Oudkerk M. Dobutamine cardiovascular magnetic resonance for the detection of myocardial ischemia with the use of myocardial tagging. Circulation 2003;107:1592–1597. Bree D, Wollmuth JR, Cupps BP, et al. Low-dose dobutamine tissue-tagged magnetic resonance imaging with 3-dimensional strain analysis allows assessment of myocardial viability in patients with ischemic cardiomyopathy. Circulation 2006;114(Suppl I):I33–I36 Kraitchman DL, Sampath S, Castillo E, et al. Quantitative ischemia detection during cardiac magnetic resonance stress testing by use of FastHARP. Circulation 2003;107:2025–2030. Kim D, Gilson WD, Kramer CM, Epstein FH. Myocardial tissue tracking with two-dimensional cine displacement-encoded MR imaging: development and initial evaluation. Radiology 2004;230: 862– 871. Pennell DJ. Cardiovascular magnetic resonance and the role of adenosine pharmacologic stress. Am J Cardiol 2004;94(2A):26D– 31D. Christian TF, Rettmann DW, Aletras AH, et al. Absolute myocardial perfusion in canines measured by using dual-bolus first-pass MR imaging. Radiology 2004;232:677– 684. Elkington AG, Gatehouse PD, Cannell TM, et al. Comparison of hybrid echo-planar imaging and FLASH myocardial perfusion cardiovascular MR imaging. Radiology 2005;235:237–243. Schreiber WG, Schmitt M, Kalden P, Mohrs OK, Kreitner KF, Thelen M. Dynamic contrast-enhanced myocardial perfusion imaging using saturation-prepared TrueFISP. J Magn Reson Imaging 2002; 16:641– 652 Schwitter J, Nanz D, Kneifel S, et al. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation 2001;103:2230 –2235. Nagel E, Klein C, Paetsch I, et al. Magnetic resonance perfusion measurements for the noninvasive detection of coronary artery disease. Circulation 2003;108:432– 437. 12 24. Wolff SD, Schwitter J, Coulden R, et al. Myocardial first-pass perfusion magnetic resonance imaging: a multicenter dose-ranging study. Circulation 2004;110:732–737. 25. Ishida M, Sakuma H, Kato N, et al. Contrast-enhanced MR imaging for evaluation of coronary artery disease before elective repair of aortic aneurysm. Radiology 2005;237:458 – 464. 26. Ishida N, Sakuma H, Motoyasu M, et al. Noninfarcted myocardium: correlation between dynamic first-pass contrast-enhanced myocardial MR imaging and quantitative coronary angiography. Radiology 2003;229:209 –216. 27. Sakuma H, Suzawa N, Ichikawa Y, et al. Diagnostic accuracy of stress first-pass contrast-enhanced myocardial perfusion MRI compared with stress myocardial perfusion scintigraphy. AJR Am J Roentgenol 2005;185:95–102. 28. Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 1999;100:1992–2002. 29. Kim RJ, Shah DJ, Judd RM. How we perform delayed enhancement imaging. J Cardiovasc Magn Reson 2003;5:505–514. 30. Arheden H, Saeed M, Higgins CB, et al. Measurement of the distribution volume of gadopentetate dimeglumine at echo-planar MR imaging to quantify myocardial infarction: comparison with 99mTc-DTPA autoradiography in rats. Radiology 1999;211:698 – 708. 31. Messroghli DR, Radjenovic A, Kozerke S, et al. Modified LookLocker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 2004;52:141–146. 32. Kellman P, Arai AE, McVeigh ER, Aletras AH. Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement. Magn Reson Med 2002;47:372– 383. 33. Huber AM, Schoenberg SO, Hayes C, et al. Phase-sensitive inversion-recovery MR imaging in the detection of myocardial infarction. Radiology 2005;237:854 – 860. 34. Kuhl HP, Papavasiliu TS, Beek AM, Hofman MB, Heusen NS, van Rossum AC. Myocardial viability: rapid assessment with delayed contrast-enhanced MR imaging with three-dimensional inversionrecovery prepared pulse sequence. Radiology 2004;230:576 –582. 35. Kim RJ, Wu E, Rafael A, Chen EL, et al. The use of contrastenhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 2000;343:1445–1453. 36. Choi KM, Kim RJ, Gubernikoff G, Vargas JD, Parker M, Judd RM. Transmural extent of acute myocardial infarction predicts longterm improvement in contractile function. Circulation 2001;104: 1101–1107. 37. Abdel-Aty H, Zagrosek A, Schulz-Menger J, et al. Delayed enhancement and T2-weighted cardiovascular magnetic resonance imaging differentiate acute from chronic myocardial infarction. Circulation 2004;109:2411–2416. 38. Soriano CJ, Ridocci F, Estornell J, Jimenez J, Martinez V, De Velasco JA. Noninvasive diagnosis of coronary artery disease in patients with heart failure and systolic dysfunction of uncertain etiology, using late gadolinium-enhanced cardiovascular magnetic resonance. J Am Coll Cardiol 2005;45:743–748. 39. Wu KC, Zerhouni EA, Judd RM, et al. Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation 1998;97:765– 772. 40. Gerber BL, Garot J, Bluemke DA, Wu KC, Lima JA. Accuracy of contrast-enhanced magnetic resonance imaging in predicting improvement of regional myocardial function in patients after acute myocardial infarction. Circulation 2002;106:1083–1089. 41. Wagner A, Mahrholdt H, Holly TA, et al. CE-MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet 2003;361:374 –379. 42. Kitagawa K, Sakuma H, Hirano T, Okamoto S, Makino K, Takeda K. Acute myocardial infarction: myocardial viability assessment in patients early thereafter comparison of contrast-enhanced MR imaging with resting (201)Tl SPECT. Single photon emission computed tomography. Radiology 2003;226:138 –144. 43. Ingkanisorn WP, Rhoads KL, Aletras AH, Kellman P, Arai AE. Gadolinium delayed enhancement cardiovascular magnetic resonance correlates with clinical measures of myocardial infarction. J Am Coll Cardiol 2004;43:2253–2259. 44. Ichikawa Y, Sakuma H, Suzawa N, et al. Late gadolinium-enhanced magnetic resonance imaging in acute and chronic myocardial in- Sakuma 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. farction. Improved prediction of regional myocardial contraction in the chronic state by measuring thickness of nonenhanced myocardium. J Am Coll Cardiol 2005;45:901–909. Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol 1999;33:1756 –1824. Mollet NR, Cademartiri F, van Mieghem CA, et al. High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 2005;112:2318 –2323. Foo TK, Ho VB, Saranathan M, et al. Feasibility of integrating high-spatial-resolution 3D breath-hold coronary MR angiography with myocardial perfusion and viability examinations. Radiology 2005;235:1025–1030 van Geuns RJ, Wielopolski PA, de Bruin HG, et al. MR coronary angiography with breath-hold targeted volumes: preliminary clinical results. Radiology 2000;217:270 –227 Regenfus M, Ropers D, Achenbach S, et al. Noninvasive detection of coronary artery stenosis using contrast-enhanced three-dimensional breath-hold magnetic resonance coronary angiography. J Am Coll Cardiol 2000;36:44 –50. Holland AE, Goldfarb JW, Edelman RR. Diaphragmatic and cardiac motion during suspended breathing: preliminary experience and implications for breath-hold MR imaging. Radiology 1998;209:483– 489. Kim WY, Danias PG, Stuber M, et al. Coronary magnetic resonance angiography for the detection of coronary stenoses. N Eng J Med 2001;345:1863–1869. McCarthy RM, Shea SM, Deshpande VS, et al. Coronary MR angiography: true FISP imaging improved by prolonging breath holds with preoxygenation in healthy volunteers. Radiology 2003;227: 283–288. Spuentrup E, Katoh M, Buecker A, et al. Free-breathing 3D steadystate free precession coronary MR angiography with radial k-space sampling: comparison with Cartesian k-space sampling and cartesian gradient-echo coronary MR angiography—pilot study. Radiology 2004;231:581–586. Jahnke C, Paetsch I, Schnackenburg B, et al. Coronary MR angiography with steady-state free precession: individually adapted breath-hold technique versus free-breathing technique. Radiology 2004;232:669 – 676. Kefer J, Coche E, Legros G, et al. Head-to-head comparison of three-dimensional navigator-gated magnetic resonance imaging and 16-slice computed tomography to detect coronary artery stenosis in patients. J Am Coll Cardiol 2005;46:92–100. Weber OM, Martin AJ, Higgins CB. Whole-heart steady-state free precession coronary artery magnetic resonance angiography. Magn Reson Med 2003;50:1223–1228. Jahnke C, Paetsch I, Nehrke K, et al. Rapid and complete coronary arterial tree visualization with magnetic resonance imaging: feasibility and diagnostic performance. Eur Heart J 2005;26:2313–2319. Sakuma H, Ichikawa Y, Suzawa N, et al. Assessment of coronary arteries with total study time of less than 30 minutes by using whole-heart coronary MR angiography. Radiology 2005;237:316 – 321. Plein S, Jones TR, Ridgway JP, Sivananthan MU. Three-dimensional coronary MR angiography performed with subject-specific cardiac acquisition windows and motion-adapted respiratory gating. AJR Am J Roentgenol 2003;180:505–512. Sakuma H, Ichikawa Y, Chino S, Hirano T, Makino K, Takeda K. Detection of coronary artery stenosis with whole heart coronary magnetic resonance angiography. J Am Coll Cardiol 2006;48:1946 –1950. Bunce NH, Lorenz CH, Keegan J, et al. Coronary artery anomalies: assessment with free-breathing three-dimensional coronary MR angiography. Radiology 2003;227:201–208. Datta J, White CS, Gilkeson RC, et al. Anomalous coronary arteries in adults: depiction at multi-detector row CT angiography. Radiology 2005;235:812– 818. Greil GF, Stuber M, Botnar RM, et al. Coronary magnetic resonance angiography in adolescents and young adults with Kawasaki disease. Circulation 2002;105:908 –911. MRI for Ischemic Heart Disease 64. Mavrogeni S, Papadopoulos G, Douskou M, Kaklis S, Seimenis I, Baras P, Nikolaidou P, Bakoula C, Karanasios E, Manginas A, Cokkinos DV. Magnetic resonance angiography is equivalent to X-ray coronary angiography for the evaluation of coronary arteries in Kawasaki disease. J Am Coll Cardiol 2004;43:649 – 652. 65. Fayad ZA, Fuster V, Fallon JT, et al. Noninvasive in vivo human coronary artery lumen and wall imaging using black-blood magnetic resonance imaging. Circulation 2000;102:506 –510. 66. Kim WY, Stuber M, Bornert P, Kissinger KV, Manning WJ, Botnar RM. Three-dimensional black-blood cardiac magnetic resonance coronary vessel wall imaging detects positive arterial remodeling in patients with nonsignificant coronary artery disease. Circulation 2002;106:296 –299. 67. Spuentrup E, Buecker A, Katoh M, et al. Molecular magnetic resonance imaging of coronary thrombosis and pulmonary emboli with a novel fibrin-targeted contrast agent. Circulation 2005;111: 1377–1382. 68. Stuber M, Botnar RM, Fischer SE, et al. Preliminary report on in vivo coronary MRA at 3 Tesla in humans. Magn Reson Med 2002; 48:425– 429. 69. Sommer T, Hackenbroch M, Hofer U, et al. Coronary MR angiography at 3.0 T versus that at 1.5 T: initial results in patients suspected of having coronary artery disease. Radiology 2005;234:718 –725. 70. Rubinstein RI, Askenase AD, Thickman D, Feldman MS, Agarwal JB, Helfant RH. Magnetic resonance imaging to evaluate patency of aortocoronary bypass grafts. Circulation 1987;76:786 –791. 71. Aurigemma GP, Reichek N, Axel L, Schiebler M, Harris C, Kressel HY. Noninvasive determination of coronary artery bypass graft patency by cine magnetic resonance imaging. Circulation 1989; 80: 1595–1602. 72. Wintersperger BJ, Engelmann MG, Von Smekal A, et al. Patency of coronary bypass grafts: assessment with breath-hold contrast-enhanced MR angiography—value of a non-electrocardiographically triggered technique. Radiology 1998;208:345–351. 73. Bunce NH, Lorenz CH, John AS, Lesser JR, Mohiaddin RH, Pennell DJ. Coronary artery bypass graft patency: assessment with true fast imaging with steady-state precession versus gadolinium-enhanced MR angiography. Radiology 2003;227:440 – 446. 74. Langerak SE, Vliegen HW, de Roos A, et al. Detection of vein graft disease using high-resolution magnetic resonance angiography. Circulation 2002;105:328 –333. 13 75. Langerak SE, Kunz P, Vliegen HW, et al. MR flow mapping in coronary artery bypass grafts: a validation study with Doppler flow measurements. Radiology 2002;222:127–135. 76. Ishida N, Sakuma H, Cruz BP, et al. MR flow measurement in the internal mammary artery-to-coronary artery bypass graft: comparison with graft stenosis at radiographic angiography. Radiology 2001;220:441– 447. 77. Bedaux WL, Hofman MB, Vyt SL, Bronzwaer JG, Visser CA, van Rossum AC. Assessment of coronary artery bypass graft disease using cardiovascular magnetic resonance determination of flow reserve. J Am Coll Cardiol 2002;40:1848 –1855. 78. Salm LP, Bax JJ, Vliegen HW, et al. Functional significance of stenoses in coronary artery bypass grafts. Evaluation by singlephoton emission computed tomography perfusion imaging, cardiovascular magnetic resonance, and angiography. J Am Coll Cardiol 2004;44:1877–1882. 79. Salm LP, Langerak SE, Vliegen HW, et al. Blood flow in coronary artery bypass vein grafts: volume versus velocity at cardiovascular MR imaging. Radiology 2004;232:915–920. 80. Sakuma H, Blake LM, Amidon TM, et al. Coronary flow reserve: noninvasive measurement in humans with breath-hold velocityencoded cine MR imaging. Radiology 1996;198:745–750. 81. Sakuma H, Saeed M, Takeda K, et al. Quantification of coronary artery volume flow rate using fast velocity-encoded cine MR imaging. AJR Am J Roentgenol 1997;168:1363–1367. 82. Saito Y, Sakuma H, Shibata M, et al. Assessment of coronary flow velocity reserve using fast velocity-encoded cine MRI for noninvasive detection of restenosis after coronary stent implantation. J Cardiovasc Magn Reson 2001;3:209 –214. 83. Nagel E, Thouet T, Klein C, et al. Noninvasive determination of coronary blood flow velocity with cardiovascular magnetic resonance in patients after stent deployment. Circulation 2003;107: 1738 –1743. 84. Jeetley P, Hickman M, Kamp O, et al. Myocardial contrast echocardiography for the detection of coronary artery stenosis: a prospective multicenter study in comparison with single-photon emission computed tomography. J Am Coll Cardiol 2006;47:141–145. 85. George RT, Silva C, Cordeiro MA, et al. Multidetector computed tomography myocardial perfusion imaging during adenosine stress. J Am Coll Cardiol 2006;48:153–160.